M[acute{o}]nica Avil[acute{e}]s
Abstract
This article describes the results of otoacoustic emissions testing in five patients with sensorineural hearing loss. We conducted an audiologic evaluation and performed image and cerebral function studies on each patient. Our investigation revealed that all five had spontaneous otoacoustic emissions and/or distortion product otoacoustic emissions. Pharmacologic treatment with anxiolytics, antidepressants, and anticonvulsant drugs was successful in alleviating symptoms in three patients. An organic and a central functional cause of symptoms was found in the remaining two patients. Before pharmacologic therapy, the spontaneous otoacoustic emissions were of high intensity, and the distortion product emissions were minimal. Following drug therapy, the former disappeared and the latter appeared.
Introduction
Kemp's description of otoacoustic emissions in 1978 spurred great interest in cochlear micromechanics and the modulation mechanisms involved in the transmission of auditory information. [1] Since then, many investigations have shown that otoacoustic emissions are the result of the rapid contraction of the outer hair cells. [2-4] With their interconnected endoplasmic reticular structure and the presence of numerous contractile proteins (e.g., nonpolymerized actin, alpha-active myosin, fibrin, and tubulin), these cells have the capacity to move the tectorial and basilar membranes to a frequency of 30 kHz.
Different stimuli, both internal and external, are capable of producing a depolarization and contraction of the outer hair cells. They include direct electrical stimuli, mechanical stimuli brought about by the deflection of cilia, and chemical stimuli produced by iontophoresis with acetylcholine, a neurotransmitter present in the cochlear efferent pathway.
Schuknecht [5] and Warr and Guinan [6] described the presence of a large number of neurons in the auditory cortex that extend parallel to the cochlear afferent pathway. These neurons are connected to the lowest hearing centers and the organ of Corti. Years ago, Rasmussen described the presence of 300 to 600 nerve fibers that extend from the upper olivary complex, through the anastomotic branch of Oort, to the lower vestibular nerve, and down to the inner and primarily the outer hair cells. [7]
The fibers that originate in the lateral area of the upper olivary complex extend through the ipsilateral cochlea and end under the nerve fibers on the inner hair cells. The fibers that originate in the median area of the upper olivary complex extend through the contralateral cochlea down to the outer hair cells.
According to Spoendlin, three or four fibers end on each outer hair cell, but none ends directly on the inner hair cells. [8] Lim wrote that cochlear afferent pathway activity can be adjusted by efferent impulses through the subsynaptic cisterns of the inner hair cells. [2] His findings are consistent with the experience of other authors, who have observed a decrease or disappearance of otoacoustic emissions following the application of contralateral auditory stimulation in humans and other mammals. [9-11]
In this article, we describe the results of our study of five patients with sensorineural hearing loss who underwent otoacoustic emissions testing. Our findings lead us to believe that different disorders of the mechanisms of auditory regulation and modulation might be directly responsible for hearing loss, tinnitus, and vertigo of retrocochlear origin. We believe that these disorders might be studied or diagnosed with the use of otoacoustic emissions.
Case reports
In 1993 and 1994, we identified five patients whose hearing tests had yielded interesting results. We registered their otoacoustic emissions with two pieces of equipment: the Virtual 330 and the Madsen Celesta 503. Both of these devices were equipped with a PC 486 Dx 80 MHz and a color laser printer.
We recorded the spontaneous otoacoustic emissions (SOAE) and distortion product otoacoustic emissions (DPOAE) of each patient. Patients were considered to have SOAE when their emission levels were 3 dB of sound pressure level (SPL) higher than the average level of environmental noise. We classified SOAE into four categories: light (3 to 5 dB SPL), moderate (6 to 10), intense (11 to 15), and very intense ([geq]16). To register DPOAE, we used two pure tones (F1 AND F2) of 65 and 75 dB SPL as a stimulus. Tests were performed sequentially at 0.5 to 8 kHz. The DPOAE following 2F1-F2 are graphically displayed as "distortion product-gram" (DPgram). We use the same four classification categories for the DPOAE results.
Case 1. A previously healthy 25-year-old woman complained of a sudden hearing loss in her left ear, which was accompanied by continuous and intense white-noise tinnitus. She had visited a number of otolaryngologists and had been prescribed various treatments (e.g., corticosteroids, vitamins, and vasodilators). When there was no improvement in her condition, she was diagnosed as having apparent viral damage. The woman was described as a perfectionist, and she was very nervous and tense. Prior to her hearing loss, she had gone through a period of family problems that had put a strain on her state of mind.
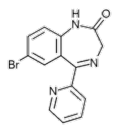
Our examination revealed a sensorineural hearing loss in both the high and low frequencies. Pneumocistemography and computed tomography (CT) of the cerebellopontine angle ruled out the presence of a neuroma. Otoacoustic emissions testing revealed that an SOAE was present in both ears (figure 1). The SOAE was intense in the right ear (12dB SPL) and intense in the left (15 dB SPL). DPOAE was absent in the left ear and intense at 1 to 2 kHz in the right. She was prescribed the benzodiazepine bromazepam (1.5mg ql2h po) and fixedcombination (12.5/5 mg) amitriptyline/chlordiazepoxide (once daily po) for 4 months.
At the conclusion of her drug regimen, we performed another emissions test (figure 2). Repeat testing showed a significant attenuation of SOAE in the left ear (3 to 4dB SPL) and a complete resolution in the right. A moderate DPOAE was observed in the left ear (6 dB SPL at 1.5 to 4 kHz), and the DPOAE in the right had increased. Audiometry results remained normal in the right ear, the tinnitus in the left had disappeared, and hearing loss completely resolved.
Case 2. A 48-year-old man experienced rotatory dizziness and imbalance that became worse with head movement and was associated with tinnitus in the left ear. Audiometry revealed a slight bilateral and symmetrical sensorineural hearing loss in the high and low frequencies, with good discrimination. Other hearing test results were normal.
Emissions testing detected a very intense (22 dB SPL) SOAE in both ears and a moderate DPOAE at4 and 8 kHz. The man was prescribed a treatment regimen similar to that given to patient 1. One month later, repeat testing showed a significant reduction in the SOAE (10 dB SPL) in both ears and no change in DPOAE in either ear.
Case 3. For several months, a 49-year-old man had experienced rotatory dizziness, imbalance, nausea, and vomiting, which were followed by a hearing loss and a sensation of pressure in the left ear. These episodes lasted approximately 1 hour and they tended to abate following a long period of sleep. The patient said that the onset of his symptoms coincided with a period of intense stress at work.
Audiometry showed a sensorineural hearing loss in the left ear at the medium frequencies (0.5 kHz to 50 dB and 1 kHz to 35 dB) and normal hearing in the right. He had good discrimination, good timing on the auditory brain (evoked) response (ABR) test, and a normal glycerol test. Magnetic resonance imaging (MRI) was performed on the brain and the posterior fossa, and results were normal. The otoacoustic emissions study showed a very intense SOAE in both ears (16 dB SPL); the patient also had a DPOAE in both ears to a level of 2 to 4 kHz, but it was virtually absent in the other frequencies. A computerized analysis of electroencephalographic brain mapping showed an irritative epileptiform focus in the left temporal subcortical area. The man was prescribed bromazepam (1.5 mg ql2h po) and the anticonvulsant carbamazepine (200 mg q12h po).
After 1 week of drug treatment, the patient had begun to experience an alleviation of the dizziness and an improvement in hearing. After 5 months of therapy, repeat testing revealed that the patient's hearing was normal and that the SOAE in both ears had disappeared. His DPOAE had increased and was present in both the high and low frequencies.
Case 4. A 4-year-old boy had an untreated right temporoparietal hematoma of perinatal origin, which caused insomnia and frequent agitation. He had been brought to the clinic for evaluation of a long-evolving deep bilateral hearing loss.
Audiometry showed a deep sensorineural hearing loss, descending from 55 dB at 128Hz to 110 dB at 4kHz in the right ear and showing profound deafness in the left. Impedance test results were normal, and the ABR test showed a good response only in the right ear at 80 dB. Otoacoustic emissions testing showed an intense SOAE in both ears (10 to 12 dB SPL) and a moderate DPOAE, especially in the high frequencies. Electroencephalographic brain mapping showed the presence of focal epileptiform irritative activity in the right central regions of the frontal lobe.
Case 5. Four months before coming to our clinic, a 62-year-old woman had suddenly experienced a sensation that both of her ears were full. This feeling had been accompanied by left tinnitus, rotatory dizziness, imbalance, and vomiting, which worsened with head movement. The following day, she said her right ear had returned to normal, but the tinnitus and hearing loss in the left had persisted. An otolaryngologist had prescribed different treatments, but her condition did not improve.
The ENT physical examination was normal. Audiometry revealed a severe sensorineural hearing loss in the left ear. The woman's ABR conduction time was normal, but her otoacoustic emissions analysis detected a very intense SOAE and DPOAE in the right ear, and an intense SOAE and no DPOAE in the left.
CT of the brain detected a lacunar infarct on the right side of the globus pallidus and the putamen of the right hemisphere.
Discussion
SOAE was found in the absence of DPOAE in patients 1, 2, and 3. In these three cases, drug therapy was prescribed, and these patients experienced a definite improvement, as their tinnitus, dizziness, and vertigo disappeared. Moreover, patient 3 also experienced an improvement in hearing. Repeat testing revealed how effective drug treatment was in modifying otoacoustic emissions, and we observed a reduction or resolution of SOAE and an increase in DPOAE.
In cases 4 and 5, SOAE and DPOAE were found in apparently cofotic ("dead") ears and in ears with severe hearing loss. CT and MRI allowed us to identify an organic and a central functional cause in patients 4 and 5, respectively.
Most investigators believe that otoacoustic emissions--whether they be spontaneous, product distortion, or evoked--are present in healthy cochleae. [12,13] Otoacoustic emissions testing is regarded as the only test capable of demonstrating the function of the organ of Corti, especially in the outer hair cells, in an objective, noninvasive, and reproducible way. There is also a consensus that different noxious factors that can affect the cochlea--such as ototoxics (acetylsalicylic acid, aminoglycosides, etc.) and acoustic disorders--diminish or eliminate otoacoustic emissions. [14-16] Finally, it is accepted that otoacoustic emissions are modified by stimulation of the efferent auditory system, as contralateral acoustic stimuli reduce distortion product and evoked emissions. [17-20] For these reasons, the use of otoacoustic emissions testing is widely acknowledged as useful for making auditory assessments of newborns and patients who have been exposed to ototoxics or environmental noise, and for controlling c ortipathy--that is, damage to or a lesion in the organ of Corti.
In the five patients we studied, the diagnosis was not clear, although in some of them, the possibility of endolymphatic hydrops, sudden hearing loss, etc., was proposed. However, the presence of otoacoustic emissions in these patients was a sign that the organ of Corti was undamaged, and this suggested the possibility that symptoms originated from a retrocochlear or central origin.
In our study, our attention was drawn to the relationship between SOAE and DPOAE in patients 1,2, and 3 and the resolution of symptoms following a course of pharmacologic treatment. There is no description in the literature of any correlation between these types of otoacoustic emissions in patients who experience sensorineural hearing loss, tinnitus, or vertigo, but there are some reports of otoacoustic emissions in patients who had sensorineural hearing loss. [21-25] The presence of otoacoustic emissions in patients 4 and 5, especially SOAE, led us to consider intense irritative activity and a lacunar infarct, respectively, as possible explanations for these patients' symptoms.
Based on the findings of our study, we pose a series of hypotheses:
* The presence of otoacoustic emissions, either SOAE or DPOAE, implies that the cochlea and outer hair cells are functionally normal.
* The presence of intense SOAE should be a common finding in patients who have an undamaged cochlear system but who have some retrocochlear or central disorder that impedes the normal inhibitory activity of the efferent auditory system.
* The presence of DPOAE in an ear with a sensorineural hearing loss is a sign that the patient has a healthy cochlea and normally functioning outer hair cells and efferent auditory system. Therefore, the problem probably has a central origin.
* Among the causes that might explain some organic pathologies are lacunar infarcts, sclerosis, brain lesions, and arteriovenous malformations.
* Among the etiologies of functional disorders are electrical causes, factors similar to those that cause epilepsy, depression, and stress, all of which have been proposed by other authors. [26,27]
* The use of antiepileptic, anxiolytic, and antidepressant drugs in some patients with audiovestibular disorders who are studied with otoacoustic emissions testing has led to a clinical improvement in many of them. Otoacoustic emissions testing helps us establish a diagnosis and allows us to monitor the effect of treatment.
To summarize, SOAE and DPOAE testing of patients who have a sensorineural hearing loss allows us to objectively evaluate the functional state of the organ of Corti and the efferent cochlear pathway. The presence of an intense SOAE and the absence of a DPOAE suggests a retrocochlear disorder of the efferent pathway from the brain, which in some cases can be reversed with drug therapy. The presence of DPOAE in an ear of a patient with a hearing loss indicates a possible brain failure. Along with auditory evoked potentials, MRI, and brain function studies, the study of otoacoustic emissions allows us to examine lesions of retrococlilear or central origin and of different etiologies (i.e., organic or functional). Otoacoustic testing sheds light upon a field of unknown dimensions in the diagnosis of central auditory pathology, and it can suggest a possible central or efferent origin to some balance disorders.
References
(1.) Kemp DT. Stimulated acoustic emissions from within the human auditory system. J Acoust Soc Am 1978;64:1386-91.
(2.) Lim DJ. Functional structure of the organ of Corti: A review. Hear Res 1986;22:117-46.
(3.) Kemp DT, Chum R. Properties of the generator of stimulated acoustic emissions. Hear Res 1980;2:213-32.
(4.) Norton SJ. Cochlear function and otoacoustic emissions. Seminars in Hearing 1992;13:1-21.
(5.) Schuknecht HF. Pathology of the Ear. 2nd ed. Philadelphia: Lea & Febiger, 1993:69.
(6.) Warr WB, Guinan JJ, Jr. Efferent innervation of the organ of Corti: Two separate systems. Brain Ret 1979;173:152-5.
(7.) Rasmussen GL. Further observations of the efferent cochlear bundle. J Comp Neurol 1953;99:61-74.
(8.) Spoendlin H. The afferent innervation of the cochlea. In: Naunton RF, Fernandez C, eds. Evoked Electrical Activity in the Auditory Nervous System. New York: Academic Press, 1978:21-41.
(9.) Siegel JH, Kim DO. Efferent neural control of cochlear mechanics? Olivocochlear bundle stimulation affects cochlear biomechanical nonlinearity. Hear Ret 1982;6:17 1-82.
(10.) ColIet L, Kemp DT, Veuillet E, et al. Effects of contralateral auditory stimuli on active cochlear micromechanical properties in human subjects. Hear Ret 1990;43:251-61.
(11.) Iviusiek FE. Otoacoustic emissions and the olivocochlear bundle. The Hearing Journal 1992;45(1l):12-5.
(12.) Burch-Sims P. The anatomic and physiologic bases of otoacoustic emissions. The Hearing Journal 1992;45(11):9-l0.
(13.) Probst R, Lonsbury-Martin BL, Martin GK. A review of otoacoustic emissions. J Acoust Soc Am 1991;89:2027-67.
(14.) Wier CC, Pasanen EG, McFadden D. Partial dissociation of spontaneous otoacoustic emissions and distortion products during aspirin use in humans. J Acoust Soc Am 1988;84:230-7.
(15.) Probst R, Lonsbury-Martin BL, Martin GK, Coats AC. Otoacoustic emissions in ears with hearing loss. Am J Otolaryngol 1987;8:73-81.
(16.) Moulin A, Collet L, Delli D, Morgon A. Spontaneous otoacoustic emissions and sensori-neural hearing loss. Acta Otolaryngol 1991;111:835-41.
(17.) Berlin CI, Hood LJ, Hurley A, Wen H. The First Jerger Lecture. Contralateral suppression of otoacoustic emissions: An index of the function of the medial olivocochlear system. Otolaryngol Head Neck Surg 1994;110:3-21.
(18.) Moulin A, Collet L, Morgon A. Influence of spontaneous otoacoustic emissions (SOAE) on acoustic distortion product input/output functions: Does the medial efferent system act differently in the vicinity of an SOAE? Acta Otolaryngol 1992;l12:210-4.
(19.) Williams EA, Brookes GB, Prasher DK. Effects of contralateral acoustic stimulation on otoacoustic emissions following vestibular neurectomy. Scand Audiol 1993;22:197-203.
(20.) Williams EA, Brookes GB, Prasher DK. Effects of olivocochlear bundle section on otoacoustic emissions in humans: Efferent effects in comparison with control subjects. Acta Otolaryngol 1994;114:121-9.
(21.) Laccourreye L, Francois M, Tran Ba Huy E, Narcy P. Bilateral evoked otoacoustic emissions in a child with bilateral profound hearing loss. Ann Otol Rhinol Laryngol 1996;105:286-8.
(22.) Prieve BA, Gorga MP, Neely ST. Otoacoustic emissions in an adult with severe hearing loss. Speech Hear Res 1991;34:379-85.
(23.) Lutman ME, Mason SM, Sheppard S, Gibbin KP. Differential diagnostic potential of otoacoustic emissions: A case study. Audiology 1989;28:205-l0.
(24.) Welzl-Muller K, Stephan K, Stadlmann A. Click-evoked otoacoustic emissions in a child with unilateral deafness. Eur Arch Otorhinolaryngol 1993;250:366-8.
(25.) Collet L, Gartner M, Moulin A. Evoked otoacoustic emissions and sensorineural hearing loss. Arch Otolaryngol Head Neck Surg 1989;115:1060-2.
(26.) Ried E, Ried E, Peragallo A, Adrian H. [Deafness syndrome caused by efferent retrocochlear inhibition]. Acta Otorrinolaringol Esp 1993;44:253-6.
(27.) Ried E, Ried E. [Otoacoustic emissions in retrocochlear auditory dysfunction]. Acta Otorrinolaringologica Colombia 1996;24:29-39.
COPYRIGHT 2000 Medquest Communications, Inc.
COPYRIGHT 2000 Gale Group