INTRODUCTION
Concurrent use of combinations of medications has been a helpful approach in neuropsychiatry to enhance treatment efficacy. Medication combinations, by acting simultaneously on multiple neuropharmacological mechanisms, may have an additive or synergistic effect on therapeutic action and may blunt neuroadaptive changes that might serve to limit the therapeutic action of a single medication. In addition, medication combinations may allow use of lower doses of each medication, thus minimizing side effects. A successful example of this approach is the use of two dopaminergic medications, bromocriptine and L-DOPA, in the treatment of Parkinson's disease (1).
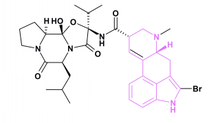
Medication combinations have been used in the treatment of cocaine addiction, for which no single medication has proven broad efficacy (2). One example is bromocriptine plus bupropion. Each of these medications enhances dopaminergic activity, albeit by different mechanisms: bromocriptine as a dopamine (primarily type D2) receptor agonist (3) and bupropion by blocking the presynaptic dopamine transporter (4). Enhancement of brain dopaminergic activity has been suggested as a pharmacotherapy approach to cocaine addiction because of the functional dopamine depletion associated with chronic cocaine use and withdrawal (2). Either bromocriptine (5,6) or bupropion (7,8) by itself has been reported effective in some open-label or small-scale clinical studies, but neither medication by itself has been shown consistently effective in double-blind controlled clinical trials (2). An open-label case series in 13 cocaine-dependent outpatients found the bromocriptine plus bupropion combination safe, with some promise of efficacy (9). After the favorable safety experience with the medication combination given on a slow dose escalation (SDE) schedule, we studied a second group of outpatients on a rapid dose escalation (RDE) schedule that gave them more time at presumed therapeutic dose levels. We report here the results from this larger open-label trial in 34 cocaine-dependent outpatients (including the 13 original patients) that compared SDE vs. RDE medication regimens.
METHODS
Subjects
Potential subjects recruited from the community received a thorough medical and psychological evaluation requiring two visits. Subject inclusion criteria were age 18-50 years, current cocaine dependence (by DSM-IIIR criteria), [greater than or equal to] 12 g of cocaine use in the prior three months, and at least one urine sample positive for cocaine. Subject exclusion criteria were current dependence on opiates; current institutional residence (e.g., half-way house); inability to comprehend the consent form or written tests; seizure disorder or history of seizures or head injury with loss of consciousness > 3 min; current medical or psychiatric symptoms that would impair ability to participate safely in the study; allergy to tricyclic antidepressants, bupropion, or bromocriptine; pregnancy or nursing; and being a woman of childbearing potential not using a medically accepted method of birth control.
The study was approved by the National Institute on Drug Abuse Institutional Review Board. Subjects were given their first clinic appointment within one week after giving written informed consent to participate.
Procedures
Subjects participated in an 8-week treatment program that required thrice weekly visits to the clinic (usually Monday, Wednesday, and Friday). At each clinic visit they ingested a medication dose under direct observation of a nurse, received additional medication to last until their next scheduled visit, gave a urine sample under staff observation, had blood pressure and pulse checked by a clinic nurse, reported on any medication side-effects, and provided self-report data on outcome measures. At one visit each week, they also received individual standardized drug abuse counseling with masters-trained counselors. The counseling was based on interpersonal psychotherapy (10) and had three phases: I--review of personal history, formulation of problems and goals, and development of a therapeutic alliance; II--development of strategies to achieve treatment goals and control drug craving and use; III--strengthening of strategies and skills that prevent drug use, learning to use available support resources, and resolution of separation and termination issues.
The primary outcome measures were cocaine use (determined by urine toxicology and self-report) and retention time in treatment. Secondary outcome measures were amount of money spent on cocaine and cocaine craving (measured by 100 mm visual-analog scale).
Urine samples were analyzed qualitatively for the cocaine metabolite benzoylecgonine (300 ng/ml cutoff concentration) using the enzyme-multiplied immunoassay technique (EMIT). Missing samples were considered positive for cocaine when either the previous or following sample was positive, and negative for cocaine only when both were negative. Urine toxicology results were available to the subjects' counselor, but the treatment program had no systematic behavioral contingencies based on the toxicology results.
Medication
All subjects took both bupropion and bromocriptine daily (bid or tid orally) in open-label fashion, but were blind to the actual dosing regimen, except for the maximum possible daily dose (disclosed in the consent form). The maximum bupropion dose (100 mg tid) was chosen because it showed some efficacy in an open-label pilot study (8), is the usual recommended dose for the treatment of depression, and is below the dose (450 mg daily) at which seizure risk increases (11). The maximum bromocriptine dose (2.5 mg tid) was chosen because it is at the upper end of the dose range used in prior studies of cocaine dependence (2) and well below the maximum dosage (100 mg) used for Parkinson's disease (3). Because of safety concerns, the first 18 subjects received a SDE regimen requiring three weeks to achieve the maximum medication dosage and spending only one week at the maximum dosage on both medications (Table 1). After the favorable safety experience with this group (9), the next 16 subjects received a more RDE regimen (Table 1) that gave them more exposure to likely therapeutic doses of the medications. The subject recruiting staff and procedures, subject eligibility criteria, and clinic staff and procedures were the same for both groups of subjects.
Data Analysis
Comparisons of baseline characteristics among groups were done by Fisher's exact test for categorical variables and analysis of variance for continuous variables. Baseline continuous variables with non-normal distributions were analyzed in terms of number of subjects in each quartile using Fisher's exact test. Retention in treatment was evaluated using Kaplan-Meier survival analysis (log rank statistic). Subjects who never attended their first clinic visit were assigned a length of stay (LOS) of zero days. Proportion of urine samples positive for cocaine metabolite was evaluated by 2-factor (medication group x time) analysis of variance using the SAS general linear model procedure. All analyses used a two-tailed alpha level of 0.05.
Treatment outcome was analyzed for the 26 subjects (13 in each group) who received medication for at least the first three clinic visits (one week), on the basis that only these subjects were evaluable in terms of medication effect (i.e., had received enough medication to potentially show a therapeutic effect). Pre vs. post evaluation of treatment effects was done by comparing subjects' status at treatment entry or during the first treatment week with their status during the last week of treatment. An intention-to-treat analysis including all 34 consented subjects could be done only for LOS in treatment because there was no outcome data on subjects who had less than three clinic visits (n = 8).
RESULTS
The 34 consented subjects had a mean (SD) age of 33.4 (4.8)years, were 67.6% male, 65% African-American, 41% with more than a high school education, 59% employed full-time, and 44% never married. Their mean income over the prior month was $1,084 (1,319), with 24% earning $500 or less. Subjects had lifetime cocaine use for 5.8 (4.5) years, with 19.2 (8.6) days of cocaine use in the prior month. Over the prior month, 76% had used alcohol more than once, 24% had used heroin, 47% had used cannabis, and they had spent $1,229 (1,484) on drugs. Fifty-three percent of subjects had prior drug abuse treatment. There were no significant differences in baseline characteristics among the three groups, except that the eight non-evaluable subjects were less likely to have had prior drug abuse treatment (12% vs. 69%, and 62%, respectively; p = 0.04 by Fisher's exact test).
Eight subjects did not keep their first three clinic appointments (5 SDE, 3 RDE); only two subjects completed the entire eight weeks. The RDE group had a significantly longer median LOS than the SDE group, whether considering all 34 consented subjects (20 days vs. 14 days; log rank = 5.12, p = 0.02) or only the 26 evaluable subjects (29 days vs. 19 days; log rank = 5.15, p = 0.02).
The proportion of urine samples positive for cocaine metabolite did not change significantly between the first week of treatment (mean [SD] of 0.82 [0.29] in SDE group, 0.79 [0.35] in RDE group) and the last week of treatment (0.85 [0.26] and 0.85 [0.29], respectively) in either medication group (F = 0.50, p = 0.49). In contrast, self-reported cocaine use declined significantly from the first week of treatment (mean [SD] of 3.2 [2.5] grams in SDE group, 5.8 [13.4] grams in RDE group) to the last week (0.6 [0.7] grams and 0.5 [0.5] grams, respectively) (F = 4.3, p = 0.05), as did the amount of money reported spent on cocaine (from $160 [$193] in SDE group and $137 [$159] in RDE group to $35 [$48], and $42 [$54], respectively) (F = 12.4, p = 0.002). Self-reported cocaine craving (100mm visual analog scale) declined modestly but significantly from the first (67 [26] in SDE group, 64 [34] in RDE group) to the last (53 [30] and 50 [37], respectively) week of treatment (F = 5.7, p = 0.03). There was no significant difference between medication groups and no significant group x time interaction for any of these four variables.
As expected from the study eligibility criteria, there was little use by subjects of other abusable drugs. Six subjects had urine samples positive for THC or opiates, four for amphetamines, and one each for benzodiazepines and PCP.
There were no serious adverse events and no subject required a change from the medication dosing schedule (Table 1). One subject was discharged for a concurrent medical problem unrelated to study medication. The only reported side effects were constipation (three subjects), nervousness (two subjects), headache, lightheadedness, sluggishness, itching, fatigue, nausea, and insomnia (each in one subject). There was no difference in side-effect frequency between the two medication groups (seven in SDE group, five in RDE group). Heart rate and blood pressure were within normal limits ([less than or equal to] 100 bpm, [less than or equal to] 140/90 mm Hg) at each visit for all subjects.
DISCUSSION
This 8-week, open-label clinical trial used two different dose escalation regimens to evaluate the safety and efficacy of the combination of bupropion and bromocriptine in the treatment of cocaine dependence. Both the SDE (one week at maximum doses) and RDE (three weeks at maximum doses) regimens (Table 1) were safe and well tolerated in this sample. There was no evidence of any clinically significant interaction with cocaine, even at clinic visits when subjects had recently used cocaine (as evidenced by cocaine-positive urine samples).
Evidence of efficacy was less clear-cut. Although subjects in the RDE group stayed significantly longer in treatment, both groups showed comparable improvement in self-report measures, i.e., significant decreases in amount of cocaine used, money spent on cocaine, and cocaine craving. The failure to observe any differences in outcome between the medication groups suggests either that the improvement was due to the psychosocial component of treatment (which was the same for both groups), rather than the medication, or that even the SDE regimen provided sufficient medication exposure to have a beneficial effect. In the absence of a placebo medication group, these two possibilities cannot be distinguished. Although medication group assignment was sequential, it is unlikely that secular trends biased the results because subject eligibility criteria and treatment staff and procedures remained unchanged throughout the study.
The changes in self-report measures were not reflected in improvement in the objective measure of proportion of urine samples positive for cocaine metabolite. This discrepancy suggests either that subjects do not recall/report their cocaine use accurately or that a thrice-weekly urine-sampling schedule fails to detect clinically relevant changes in cocaine use. Intentional under reporting of cocaine use should have been minimized by the absence of behavioral contingencies for drug use, i.e., study participation continued regardless of subjects' drug use status. Dichotomous (positive/negative) toxicology results from frequent urine sampling may overestimate the frequency of cocaine use because of carryover effects from one urine sample to the next (12). Thus, a subject may correctly report decreased cocaine use, while a urine sample is still qualitatively positive for cocaine metabolite from previous cocaine use. Application of decision rules to quantitative urine toxicology data has been suggested as a way to minimize this potential overestimation of cocaine use by qualitative urine toxicology data (12).
A major limitation of this study is the high dropout rate; 74% of subjects dropped out before completing the entire period of maximum medication dose. Other short-term studies of bromocriptine treatment for cocaine-dependent outpatients not receiving methadone maintenance treatment have also reported high dropout rates, e.g., 54% over three weeks (13), 69% over two weeks (5). It is possible that subjects' status at their last clinic visits was not representative of their overall response to treatment, or that longer exposure to medication would have yielded a more robust treatment response.
In summary, this open-label clinical trial found the bupropion and bromocriptine combination safe for use in cocaine-dependent outpatients, with no significant differences between slow and RDE regimens, but provides only equivocal evidence for its efficacy. A future double-blind, placebo-controlled clinical trial would be needed to definitively answer this question.
ACKNOWLEDGMENTS
This study was supported by NIDA intramural research funds. We thank Dr. Nicholas Carriero for help with data analysis.
[dagger] A preliminary report of these data was presented at the College on Problems of Drug Dependence, 57th Annual Scientific Meeting, Scottsdale, AZ, June, 1995 (National Institute on Drug Abuse Research Monograph 162:145, 1996).
REFERENCES
(1.) Montastruc, J.L.; Rascol, O.; Senard, J.M. Current Status of Dopamine Agonists in Parkinson's Disease Management. Drugs 1993, 46, 384-393.
(2.) Gorelick, D.A. Pharmacologic Therapies for Cocaine and Other Stimulant Addiction. In Principles of Addiction Medicine; Graham, A.W., Schultz, T.K., Eds.; American Society of Addiction Medicine: Chevy Chase, MD, 1998; 531-544.
(3.) Factor, S.A. Dopamine Agonists. Med. Clin. N. Am. 1999, 83, 415-443.
(4.) Ascher, J.A.; Cole, J.O.; Colin, J.-N.; Feighner, J.P.; Ferris, R.M.; Fibiger, H.C.; Golden, R.N.; Martin, P.; Potter, W.Z.; Richelson, E.; Sulser, F. Bupropion: A Review of Its Mechanism of Antidepressant Activity. J. Clin. Psychiatry 1995, 56, 395-401.
(5.) Moscovitz, H.; Brookoff, D.; Nelson, L. A Randomized Trial of Bromocriptine for Cocaine Users Presenting to the Emergency Department. J. Gen. Intern. Med. 1993, 8, 1-4.
(6.) Wang, R.I.H.; Kalbfleisch, J.; Cho, J.K.; Forbes, M. Bromocriptine, Desipramine, and Trazodone Alone and in Combination to Cocaine Dependent Patients. Natl Inst. Drug Abuse Res. Monogr. 1994, 141, 437.
(7.) Castaneda, R.; Sussman, N.; Levy, R.; Trujillo, M. A Treatment Algorithm for Attention Deficit Hyperactivity Disorder in Cocaine-Dependent Adults: a One-Year Private Practice Study with Long-Acting Stimulants, Fluoxetine, and Bupropion. Subst. Abuse 1999, 20, 59-71.
(8.) Margolin, A.; Kosten, T.; Petrakis, I.; Avants, S.K.; Kosten, T. Bupropion Reduces Cocaine Abuse in Methadone-Maintained Patients. Arch. Gen. Psychiatry 1991, 48, 87.
(9.) Montoya, I.D.; Preston, K.L.; Cone, E.J.; Rothman, R.; Gorelick, D.A. Safety and Efficacy of Bupropion Combined with Bromocriptine for Treatment of Cocaine Dependence. Am. J. Addict. 1996, 5, 69-75.
(10.) Rounsaville, B.J.; Gawin, F.H.; Kleber, H.D. Interpersonal Psychotherapy Adapted for Ambulatory Cocaine Abusers. Am. J. Drug. Alcohol Abuse 1985, 11, 171-191.
(11.) Peck, A.W.; Stern, W.C.; Watkinson, C. Incidence of Seizures During Treatment with Tricyclic Antidepressant Drugs and Bupropion. J. Clin. Psychiatry 1983, 44, 197-201.
(12.) Preston, K.L.; Silverman, K.; Schuster, C.R.; Cone, E.J. Assessment of Cocaine Use with Quantitative Urinalysis and Estimation of New Uses. Addiction 1997, 92, 717-727.
(13). Eiler, K.; Schaefer, M.R.; Salstrom, D.; Lowery, R. Double-Blind Comparison of Bromocriptine and Placebo in Cocaine Withdrawal. Am. J. Drug. Alcohol Abuse 1995, 21, 65-79.
Ivan D. Montoya, Kenzie L. Preston, Richard Rothman, and David A. Gorelick *
Intramural Research Program, National Institute on Drug Abuse, National Institutes of Health, 5500 Nathan Shock Drive, Baltimore, MD 21224
* Corresponding author. Fax: (410) 550-1528; E-mail: dgorelic@intra.nida.nih.gov
COPYRIGHT 2002 Marcel Dekker, Inc.
COPYRIGHT 2002 Gale Group