INTRODUCTION: Drug induced eosinophilic pleural effusion (EPE) is well documented in literature. EPE is not a disease rather an interesting laboratory finding, defined as >10% eosinophils in pleural fluid, exclusive of erythrocytes. Pleural fluid eosinophilia may be associated with blood eosinophilia e.g. Loeffler syndrome, Churg Strauss syndrome etc. Conversly EPE can also occur without blood eosinophilia e.g. Pulmonary Infarction, Pneumonia or Trauma. We report a case of bilateral EPE secondary to Artemisnin with no peripheral eosinophilia.
CASE PRESENTATION: AM 46-year-old female presented to OPD because of bilateral dull aching chest pain, which increased, on taking deep breath. Five days before the presenting illness she also had high grade fever with chills for which she received injection Artemisinin on the suspicion of malaria in another tertiary health care center. The patient demonstrated no symptom, sign or laboratory data of any infectious process, Chest X-Ray PA revealed bilateral pleural effusion more on right side & no parenchymal infiltrates. Patient underwent right thoracentesis, revealing protein-4.2 g/dl, 60%-lymphocyte, 26%-eosinophils, 10%-mesothelial cells & 4%-polymorphs. Next day, left thoracentesis revealed protein-4.4 g/dl, 56%-lymphocytes, 32%-eosinophils, 8%-mesothelial cell & 4%-polymorphs. Pleural biopsy showed mixed lymphocytic & eosinophilic infiltrates within pleura. The bacterial, fungal & mycobacterial smear & culture of fluid & biopsy specimen were negative after 6 weeks. Her serology was negative for Anti-Nuclear Antibody, LE cells, & Rheumatoid factor. There was no history of contact of pulmonary tuberculosis & Montoux test was negative. A detailed history of illness (including absence of any significant past medical history), drug intake & complete evaluation strongly pointed out towards a possible drug (Artemisnin) induced pleural effusion, hence after informed consent & with permission of ethical society of institution, injection Artemisnin 40mg IM x 5 days was given, as challenge dose & on 7th day patient again developed bilateral chest pain & Chest X-Ray revealed bilateral minimal pleural effusion. Patient was started on prednisolone 60 mg/day for 7 Days & pleura] effusion disappeared completely, hence confirming the diagnosis.
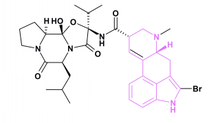
DISCUSSIONS: Air & Blood are the most common cause of EPE. Other causes of EPE1 are Bronchial or Pleural malignancy, hypersensitivity reactions, pulmonary infarction & infection with viruses, fungus (2) (Coccidiodomycosis, Histoplasmosis) & parasites (Echinococcus, Amoebiasis, Ascariaris, Schistosomiasis, Ankylostomiasis etc.). Drug reactions like Dantrolene, Bromocriptine, Nitrofurantoin. Procarbazine, Ergot, Methotrexate has been implicated in EPE. Allergic disease like Asthma, Tropical Pulmonary Eosonipbilia, Churg-Strauss syndrome may also lead to Eosinophilic Pleural Effusion. (3) In this case the absence of other causes for the EPE & its complete resolution after withdrawal of Artemisnin, reappearance on challenging with low dose supports a causative relationship of this drug with the development of EPE. This is probably the first case report of EPE secondary to Artemisnin.
CONCLUSION: Artemisnin must be included in the list of drugs causing EPE, however the exact mechanism is not known, but, if the drug is considered as a cause of EPE, the drug should be immediately discontinued. Clinical Implications: a high degree of suspicion should always be kept in mind to prove the drug as an etiologic agent in undiagnosed EPE, and a challenge test with all due precautions should always be done to prove or disprove this etiology.
REFERENCES:
(1) Campbell GD, Webb WR: Eosinophilic Pleural Effusion, Amer. Rev. Resp. Dis. 1964, 90, 194.
(2) Curran WS, Williams AW: Eosinophilic Pleural Effusion, Arch. Inern. Med. (Chiacgo) 1963, 111, 809.
(3) Erzurum SE, Underwood GA, Hamilos DL, Waldron JA: Pleural eff
DISCLOSURE: Mayank Vats, None.
Mayank Vats MD * Rakesh C. Gupta MD Deepa V. Khandelwal MBBS Manohar L. Gupta MD Neeraj Gupta MD Mukesh Tailor MBBS J.L.N. Medical College, Ajmer, Rajasthan, India
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group