Definition
Allergies are abnormal reactions of the immune system which occur in response to otherwise harmless substances.
Description
Allergies are among the most common of medical disorders. It is estimated that 60 million Americans, or more than one in every five people, suffer from some form of allergy, with similar proportions throughout much of the rest of the world. Allergy is the single largest reason for school absence and is a major source of lost productivity in the workplace.
An allergy is a type of immune reaction. Normally, the immune system responds to foreign microorganisms or particles, like pollen or dust, by producing specific proteins called antibodies that are capable of binding to identifying molecules, or antigens, on the foreign particle. This reaction between antibody and antigen sets off a series of reactions designed to protect the body from infection. Sometimes, this same series of reactions is triggered by harmless, everyday substances. This is the condition known as allergy, and the offending substance is called an allergen.
Allergens enter the body through four main routes: the airways, the skin, the gastrointestinal tract, and the circulatory system.
People with allergies are not equally sensitive to all allergens. Some may have severe allergic rhinitis but no food allergies, for instance, or be extremely sensitive to nuts but not to any other food. Allergies may get worse over time. For example, childhood ragweed allergy may progress to year-round dust and pollen allergy. On the other hand, a person may lose allergic sensitivity. Infant or childhood atopic dermatitis disappears in almost all people, for example. More commonly, what seems to be loss of sensitivity is instead a reduced exposure to allergens or an increased tolerance for the same level of symptoms.
- Airborne allergens cause the sneezing, runny nose, and itchy, bloodshot eyes of hay fever (allergic rhinitis). Airborne allergens can also affect the lining of the lungs, causing asthma, or the conjunctiva of the eyes, causing conjunctivitis (pink eye).
- Allergens in food can cause itching and swelling of the lips and throat, cramps, and diarrhea. When absorbed into the bloodstream, they may cause hives (urticaria) or more severe reactions involving recurrent, non-inflammatory swelling of the skin, mucous membranes, organs, and brain (angioedema). Some food allergens may cause anaphylaxis, a potentially life-threatening condition marked by tissue swelling, airway constriction, and drop in blood pressure.
- In contact with the skin, allergens can cause reddening, itching, and blistering, called contact dermatitis. Skin reactions can also occur from allergens introduced through the airways or gastrointestinal tract. This type of reaction is known as atopic dermatitis.
- Injection of allergens, from insect bites and stings or drug administration, can introduce allergens directly into the circulation, where they may cause system-wide responses (including anaphylaxis), as well as the local ones of swelling and irritation at the injection site.
Causes & symptoms
Causes
Mast cells, one of the major players in allergic reactions, capture and display a particular type of antibody, called immunoglobulin type E (IgE) that binds to allergens. Inside mast cells are small chemical-filled packets called granules. Granules contain a variety of potent chemicals, including histamine.
Immunologists separate allergic reactions into two main types: immediate hypersensitivity reactions, which are mainly mast cell-mediated and occur within minutes of contact with allergen, and delayed hypersensitivity reactions, mediated by T cells (a type of white blood cells) and occurring hours to days after exposure.
Inhaled or ingested allergens usually cause immediate hypersensitivity reactions. Allergens bind to IgE antibodies on the surface of mast cells, which spill the contents of their granules out onto neighboring cells, including blood vessels and nerve cells. Histamine binds to the surfaces of these other cells through special proteins called histamine receptors. Interaction of histamine with receptors on blood vessels causes increased leakiness, leading to the fluid collection, swelling and increased redness. Histamine also stimulates pain receptors, making tissue more sensitive and irritable. Symptoms last from one to several hours following contact.
In the upper airways and eyes, immediate hypersensitivity reactions cause the runny nose and itchy, bloodshot eyes typical of allergic rhinitis. In the gastrointestinal tract, these reactions lead to swelling and irritation of the intestinal lining, which causes the cramping and diarrhea typical of food allergy. Allergens that enter the circulation may cause hives, angioedema, anaphylaxis, or atopic dermatitis.
Allergens on the skin usually cause delayed hypersensitivity reaction. Roving T cells contact the allergen, setting in motion a more prolonged immune response. This type of allergic response may develop over several days following contact with the allergen, and symptoms may persist for a week or more.
The role of inheritance
While allergy to specific allergens is not inherited, the likelihood of developing some type of allergy seems to be, at least for many people. If neither parent has allergies, the chances of a child developing allergy is approximately 10-20%; if one parent has allergies, it is 30-50%; and if both have allergies, it is 40-75%.One source of this genetic predisposition is in the ability to produce higher levels of IgE in response to allergens. Those who produce more IgE will develop a stronger allergic sensitivity.
Common allergens
The most common airborne allergens are the following:
- Plant pollens
- Animal fur and dander
- Body parts from house mites (microscopic creatures found in all houses)
- House dust
- Mold spores
- Cigarette smoke
- Solvents
- Cleaners.
Common food allergens include the following:
- Nuts, especially peanuts, walnuts, and Brazil nuts
- Fish, mollusks, and shellfish
- Eggs
- Wheat
- Milk
- Food additives and preservatives.
The following types of drugs commonly cause allergic reactions:
- Penicillin or other antibiotics
- Flu vaccines
- Tetanus toxoid vaccine
- Gamma globulin.
Common causes of contact dermatitis include the following:
- Poison ivy, oak, and sumac
- Nickel or nickel alloys
- Latex.
Insects and other arthropods whose bites or stings typically cause allergy include the following:
- Bees, wasps, and hornets
- Mosquitoes
- Fleas
- Scabies.
Symptoms
Symptoms depend on the specific type of allergic reaction. Allergic rhinitis is characterized by an itchy, runny nose, often with a scratchy or irritated throat due to post-nasal drip. Inflammation of the thin membrane covering the eye (allergic conjunctivitis) causes redness, irritation and increased tearing in the eyes. Asthma causes wheezing, coughing, and shortness of breath. Symptoms of food allergies depend on the tissues most sensitive to the allergen and whether it is spread systemically by the circulatory system. Gastrointestinal symptoms may include swelling and tingling in the lips, tongue, palate or throat; nausea; cramping; diarrhea; and gas. Contact dermatitis is marked by reddened, itchy, weepy skin blisters.
Whole body or systemic reactions may occur from any type of allergen, but are more common following ingestion or injection of an allergen. Skin reactions include the raised, reddened, and itchy patches called hives. A deeper and more extensive skin reaction, involving more extensive fluid collection, is called angioedema. Anaphylaxis is marked by airway constriction, blood pressure drop, widespread tissue swelling, heart rhythm abnormalities, and in some cases, loss of consciousness.
Diagnosis
Allergies can often be diagnosed by a careful medical history, matching the onset of symptoms to the exposure to possible allergens. Allergy tests can be used to identify potential allergens. These tests usually begin with prick tests or patch tests, which expose the skin to small amounts of allergen to observe the response. Reaction will occur on the skin even if the allergen is normally encountered in food or in the airways. RAST testing is a blood test that measures the level of reactive IgE antibodies in the blood. Provocation tests, most commonly done with airborne allergens, present the allergen directly through the route normally involved. Food allergen provocation tests require abstinence from the suspect allergen for two weeks or more, followed by ingestion of a measured amount. Provocation tests are not used if anaphylaxis is is a concern due to the patient's medical history. For a complete description, see the article on allergy testing.
Treatment
A large number of prescription and over-the-counter drugs are available for treatment of immediate hypersensitivity reactions. Most of these work by decreasing the ability of histamine to provoke symptoms. Other drugs counteract the effects of histamine by stimulating other systems or reducing immune responses in general.
Antihistamines
Antihistamines block the histamine receptors on nasal tissue, decreasing the effect of histamine released by mast cells. They may be used after symptoms appear, though they may be even more effective when used preventively, before symptoms appear. A wide variety of antihistamines are available.
Older antihistamines often produce drowsiness as a major side effect. Such antihistamines include the following:
- Diphenhydramine (Benadryl and generics)
- Chlorpheniramine (Chlor-trimeton and generics)
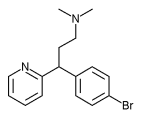
- Brompheniramine (Dimetane and generics)
- Clemastine (Tavist and generics).
Newer antihistamines that do not cause drowsiness are available by prescription and include the following:
- Astemizole (Hismanal)
- Loratidine (Claritin)
- Fexofenadine (Allegra)
- Azelastin HCl (Astelin).
Hismanal has the potential to cause serious heart arrhythmias when taken with the antibiotic erythromycin, the antifungal drugs ketoconazole and itraconazole, or the antimalarial drug quinine. Taking more than the recommended dose of Hismanal can also cause arrhythimas. Seldane (terfenadine), the original non-drowsy antihistamine, was voluntarily withdrawn from the market by its manufacturers in early 1998 because of this potential and because of the availability of an equally effective, safer alternative drug, fexofenadine.
Decongestants
Decongestants constrict blood vessels to counteract the effects of histamine. Nasal sprays are available that can be applied directly to the nasal lining and oral systemic preparations are available. Decongestants are stimulants and may cause increased heart rate and blood pressure, headaches, and agitation. Use of topical decongestants for longer than several days can cause loss of effectiveness and rebound congestion, in which nasal passages become more severely swollen than before treatment.
Topical corticosteroids
Topical corticosteroids reduce mucous membrane inflammation and are available by prescription. Allergies tend to become worse as the season progresses because the immune system becomes sensitized to particular antigens and can produce a faster, stronger response. Topical corticosteroids are especially effective at reducing this seasonal sensitization because they work more slowly and last longer than most other medication types. As a result, they are best started before allergy season begins. Side effects are usually mild, but may include headaches, nosebleeds, and unpleasant taste sensations.
Mast cell stabilizers
Cromolyn sodium prevents the release of mast cell granules, thereby preventing the release of histamine and other chemicals contained in them. It acts as a preventive treatment if it is begun several weeks before the onset of the allergy season. It can also be used for year round allergy prevention. Cromolyn sodium is available as a nasal spray for allergic rhinitis and in aerosol (a suspension of particles in gas) form for asthma.
Immunotherapy
Immunotherapy, also known as desensitization or allergy shots, alters the balance of antibody types in the body, thereby reducing the ability of IgE to cause allergic reactions. Immunotherapy is preceded by allergy testing to determine the precise allergens responsible. These tests are described in full in the article on allergy testing. Injections involve very small but gradually increasing amounts of allergen, over several weeks or months, with periodic boosters. Full benefits may take up to several years to achieve and are not seen at all in about one in five patients. Individuals receiving all shots will be monitored closely following each shot because of the small risk of anaphylaxis, a condition that can result in difficulty breathing and a sharp drop in blood pressure.
Bronchodilators
Because allergic reactions involving the lungs cause the airways or bronchial tubes to narrow, as in asthma, bronchodilators, which cause the smooth muscle lining the airways to open or dilate, can be very effective. Some bronchodilators used to treat acute asthma attacks include adrenaline, albuterol, or other "adrenoceptor stimulants," most often administered as aerosols. Theophylline, naturally present in coffee and tea, is another drug that produces brochodilation. It is usually taken orally, but in a severe asthma attack is may be given intravenously. Other drugs, including steroids, are used to prevent asthma attacks and in the long-term management of asthma.
Treatment of contact dermatitis
Calamine lotion applied to affected skin can reduce irritation somewhat. Topical corticosteroid creams are more effective, though overuse may lead to dry and scaly skin.
Treatment of anaphylaxis
The emergency condition of anaphylaxis is treated with injection of adrenaline, also known as epinephrine. People who are prone to anaphylaxis because of food or insect allergies often carry an "Epi-pen" containing adrenaline in a hypodermic needle. Prompt injection can prevent a more serious reaction from developing.
Alternative treatment
Any alternative treatment for allergies begins with finding the cause and then helping the patient to avoid or eliminate the allergen, although this is not always possible. Various categories of alternative remedies may also be helpful in allergy treatment, including:
- Antihistamines: vitamin C and the bioflavonoid hesperidin act as natural anithistamines
- Decongestants: vitamin C, the homeopathic remedies Ferrum phosphoricum and Kali muriaticum (used alternately), and the dietary supplement N-acetylcysteine are believed to have decongestant effects
- Mast cell stabilizers: the bioflavonoids quercetin and hesperidin may help stabilize mast cells
- Immunotherapy: the herbs echinacea (Echinacea spp.) and astragalus or milk-vetch root (Astragalus membranaceus) may help strengthen the immune system
- Bronchodilators: the herbal remedies ephedra (Ephedra sinica, also known as ma huang in traditional Chinese medicine), khellin (Ammi visnaga) and cramp bark (Viburnum opulus) are believed to help open the airways.
Treatment of contact dermatitis
A variety of herbal remedies, either applied topically or taken internally, can assist in the treatment of contact dermatitis. A poultice (crushed herbs applied directly to the affected area) made of jewelweed (Impatiens spp.) or chickweed (Stellaria media) can soothe the skin. A cream or wash containing calendula (Calendula officinalis), a natural antiseptic and anti-inflammatory agent, can help heal the rash when applied topically. Homeopathic treatment may include such remedies as Rhus toxicodendron, Apis mellifica, or Anacardium taken internally. A homeopathic practitioner or book should be consulted to match the symptoms with the correct remedy.
Prognosis
Allergies can improve over time, although they often worsen. While anaphylaxis and severe asthma are life-threatening, other allergic reactions are not. Learning to recognize and avoid allergy-provoking situations allows most people with allergies to lead normal lives.
Prevention
Avoiding allergens is the best means of limiting allergic reactions. For food allergies, there is no effective treatment except avoidance. By determining the allergens that are causing reactions, most people can learn to avoid allergic reactions from food, drugs, and contact allergens such as poison ivy or latex. Airborne allergens are more difficult to avoid, although keeping dust and animal dander from collecting in the house may limit exposure. Cromolyn sodium can prevent mast cell degranulation, thereby limiting the allergic response.
Key Terms
- Allergen
- A substance that provokes an allergic response.
- Allergic rhinitis
- Inflammation of the mucous membranes of the nose and eyes in response to an allergen.
- Anaphylaxis
- Increased sensitivity caused by previous exposure to an allergen that can result in blood vessel dilation and smooth muscle contraction. Anaphylaxis can result in sharp blood pressure drops and difficulty breathing.
- Angioedema
- Severe non-inflammatory swelling of the skin, organs, and brain that can also be accompanied by fever and muscle pain.
- Antibody
- A specific protein produced by the immune system in response to a specific foreign protein or particle called an antigen.
- Antigen
- A foreign protein to which the body reacts by making antibodies.
- Asthma
- A lung condition in which the airways become narrow due to smooth muscle contraction, causing wheezing, coughing, and shortness of breath.
- Atopic dermatitis
- Infection of the skin as a result of exposure to airborne or food allergens.
- Conjunctivitis
- Inflammation of the thin lining of the eye called the conjunctiva.
- Contact dermatitis
- Inflammation of the skin as a result of contact with a substance.
- Delayed hypersensitivity reactions
- Allergic reactions mediated by T cells that occur hours to days after exposure.
- Granules
- Small packets of reactive chemicals stored within cells.
- Histamine
- A chemical released by mast cells that activates pain receptors and causes cells to become leaky.
- Immune hypersensitivity reaction
- Allergic reactions that are mediated by mast cells and occur within minutes of allergen contact.
- Mast cells
- A type of immune system cell that is found in the lining of the nasal passages and eyelids, displays a type of antibody called immunoglobulin type E (IgE) on its cell surface, and participates in the allergic response by releasing histamine from intracellular granules.
- T cells
- Immune system cells or more specifically, white blood cells, that stimulate cells to create and release antibodies.
Further Reading
For Your Information
Books
- Lawlor G.J., Jr, T.J. Fischer, and D.C. Adelman. Manual of Allergy and Immunology. Boston: Little, Brown and Co., 1995.
- Novick, N.L. You Can Do Something About Your Allergies. New York: Macmillan, 1994.
- Weil, A. Natural Health, Natural Medicine: A Comprehensive Manual for Wellness and Self-Care. Boston: Houghton Mifflin, 1995.
Gale Encyclopedia of Medicine. Gale Research, 1999.