As a panel of experts neared completion of the national guidelines for asthma treatment, serious complications and some deaths have been linked to the most commonly prescribed antiasthma drugs. Implicated are the bronchodilators-theophylline and a group of drugs called beta-agonists. The new treatment guidelines, which are expected to produce radical changes in the care of children and adults with asthma, will be announced early this month by the National Asthma Education Program. They will provide much-needed guidance to physicians who use these and many other drugs to treat asthma.
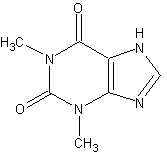
The possibility that the commonly prescribed antiasthma drugs may be contributing to the disease's rising rate of death and complications was raised at the physicians' international conference on lung health, held last year in Boston. (See HEALTHFACTS' reporting of that conference, July 1990.) That suspicion was underscored last fall when the Association of Trial Lawyers of America (ATLA) issued a "legal consumer alert" warning of the hazards of theophylline. It told of 26 cases in which ATLA members provided legal representation in incidents citing theophylline as the cause of serious injuries (e.g., brain damage following seizure in an asthmatic girl) and preventable deaths. The ATLA urged a ban on all over-the-counter theophylline drugs (e.g., Bronkaid, Primatene) and stronger warnings of potential dangers in the prescription drug's packet insert to physicians. Theophylline has been prescribed for asthma and other lung diseases for over 50 years. It is sold by prescription under more than 35 different brand names, including Bronkodyl, Choledyl, and Quibron.
The British medical journal, The Lancet (8 December 1990), recently reported evidence of heart damage from two studies that looked at the effects of regular use of a high-dose inhaled beta-agonist drug. The beta-agonists form a class of drugs that has been used to treat asthma for over 20 years. They are adrenalin-like drugs that are longer lasting and act more directly on the airways to the lungs than adrenalin, but supposedly, without adverse effects on the heart. There are five beta-agonist drugs on the market, each sold under different brand names, including Ventolin, Proventil, and Brethaire.
U.S. manufacturers of beta-agonists were quick to point out that fenoterol, the drug used in the two Lancet studies, is a longer-acting beta-agonist not available in this country. But strong evidence of fenoterol's potential for heart attacks raises a serious question about the entire class of beta-agonists. HEALTHFACTS consulted A. Sonia Buist, M.D., president of the American Thoracic Society and member of the coordinating committee that formed the new treatment guidelines. "We don't know whether the [adverse] effect found in these studies can be attributed to the whole class of beta-agonist drugs," she said in a telephone interview. "I personally think if it's a real effect, it's probably a class effect."
Dr. Buist explained that the new guidelines will advise doctors to use anti-inflammatory drugs, such as inhaled corticosteroids and cromolyn (a drug that is also antiallergy), as the primary treatment for most people with moderate to severe asthma. Beta-agonist drugs should be used as rescue medications-that is, only when needed.
This was certainly the message HEALTHFACTS brought back from the international conference on lung health, and if the new guidelines take hold, there will be a radical change in how asthma is treated. At present, most American physicians prescribe bronchodilators like theophylline and inhaled beta-agonists as the first-line treatment. Although these drugs provide immediate relief by opening up the air passages to the lungs, they treat only the symptom without affecting the inflammatory response that is present in all cases of asthma. The bronchodilators provide a false sense of security because the inflammation, if left untreated, will continue to close off the air passages.
As for the risks of theophylline: "More care should be exerted in using this drug. Doctors often prescribe it in doses that are too high," said Albert L. Sheffer, M.D., clinical professor of medicine at Harvard Medical School, in a telephone interview. Dr. Sheffer, chairman of the expert panel that developed the new guidelines, explained that this can produce toxic reactions when the person takes certain other drugs like antibiotics or the antiulcer drug, Tagamet. "Many doctors do not treat asthma properly," said Dr. Sheffer, who believes that the best care is given by a specialist.
The trend toward greater use of anti-inflammatory drugs, particularly inhaled steroids, as the primary treatment for asthma has been well underway in England, New Zealand, Australia, and Canada. A new Canadian study showing beneficial effects of regular use of inhaled steroids by 32 adult asthmatics was published recently in the American Review of Respiratory Diseases. The participants were randomly assigned to receive either inhaled steroids or placebo inhalations twice daily for one year. At the end of this study, the placebo-treated participants showed a small worsening of their condition. But the steroid-treated people showed improvement in airway responsiveness and a reduction in the severity of their asthma.
What makes this study unique is its length. Most clinical trials of anti-inflammatory drugs for asthma have been less than two months in duration. And now we come to the heart of the problem: There have been no long-term clinical trials to determine the best way to treat asthma. Until these studies are published, doctors and asthmatics must rely on the National Asthma Education Program's (NAEP) new guidelines, which are based on a consensus of expert opinion from more than 30 organizations. Periodic changes in these guidelines are to be expected as more studies are conducted.
Write to the NAEP for a Summary of the Guidelines for Asthma Management, c/o NHLBI Education Programs Information Center, 4733 Bethesda Ave., Suite 530, Bethesda, MD 20814-4820. Discussing the new guidelines with your physician will be the first step toward receiving what is currently viewed as the best care.
Call 1(800) 822-2762, the 24-hour hotline of the American Academy of Allergy and Immunology for a list of asthma specialists in your part of the country.
COPYRIGHT 1991 Center for Medical Consumers, Inc.
COPYRIGHT 2004 Gale Group