Abbreviations: IGF = insulin-like growth factor; SMC = 5-methylcytosine
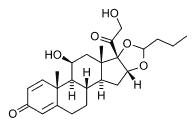
The effects of limited treatment with budesonide, an effective chemopreventive agent, on 5-methylcytosine (SMC) levels, and on the specific hypomethylation and expression of the insulin-like growth factor (IGF) II gene in mouse lung tumors was determined. Female strain A mice were administered two weekly doses of vinylcarbamate intraperitoneally. Thirty-four weeks later, mice were administered dietary budesonide (2.4 or 0.6 ppm in diet) or vehicle control for a period of 7 days and then were killed. We found that the level of 5MC in lung tumor's, measured immunologically, was reduced roughly 60% when compared with normal lung parenchyma, which is in agreement with generalized hypomethylation in many tumors. In contrast, tumors treated with budesonide for 7 days exhibited a dose-dependent increase in 5MC, with the higher dose giving 5MC levels similar to control lung parenchyma.
We subsequently examined gene expression and methylation patterns for the IGF II gene in both control tumors and tumors treated for 1 week with budesonide. Expression levels of the IGF II gene were increased roughly 2.5-fold in tumors vs normal lung parenchyma. This overexpression was reversed by treatment with budesonide for a period of 7 days. We also examined the methylation at CpG sites within the DMR2 region, which includes exons 4, 5, and 6. Within the examined region of roughly 600 nucleotides, there were 27 CpG sites. The determination of methylation in this region employed DNA isolation and bisulfite treatment, followed by amplification, cloning, and subsequent sequencing. The percentage of methylated CpG sites was 70% for normal lung parenchyma, 5% for control lung tumors, and 16% and 46% for lung tumors treated with budesonide (0.6 or 2.4 ppm, respectively, in diet) for 1 week. Thus, a chemopreventive agent, budesonide, could rapidly reverse both the generalized and specific hypomethylation observed in mouse lung tumors.
* From the Chemopreventive Agent Development Research Group-Division of Cancer Prevention (Dr. Lubet), National Cancer Institute, Rockville, MD; and the Department of Pathology (Drs. Tao, Wang, Kramer, and Perreira), Medical College of Ohio, Toledo, OH.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (e-mail: permissions@chestnet.org).
Correspondence to: Ronald A. Lubet, PhD, Program Director, NCI-DCP, Rm 2110, 6130 Executive Dr. Rockville, MD 20852; e-mail: rl57q@nih.gov
COPYRIGHT 2004 American College of Chest Physicians
COPYRIGHT 2004 Gale Group