Childhood Asthma Management Program Research Group. Long-term effects of budesonide or nedocromil in children with asthma. N Engl J Med 2000; 343:1054-63.
* BACKGROUND It is well accepted that inhaled steroids help control childhood asthma. Questions remain, however, concerning long-term use of these medicines. This study evaluated the long-term outcomes of inhaled budesonide and nedocromil.
* POPULATION STUDIED A total of 1041 children were enrolled at 8 centers. The mean age was 8.9 years. Minorities represented 30% to 35% of the participants. The children had mild to moderate asthma defined as presence of symptoms, use of an inhaled bronchodilator twice or more times weekly, or daily medication for asthma. At baseline, the patients had been hospitalized 30 times per 100 person-years, averaged 10 episode-free days per month, and had pre-bronchodilator forced expiratory volume in 1 second ([FEV.sub.1]) values of 93% predicted. In general, this population seems similar to that of a typical family practice, although more information would be helpful about family income, education, tobacco exposure, and the type of clinical centers involved.
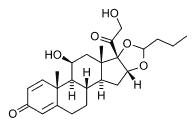
* STUDY DESIGN AND VALIDITY The participants were randomized to receive 200 [micro]g of inhaled budesonide twice daffy (n=311), 8 mg of inhaled nedocromil sodium twice daily (n=312), or placebo (n=418), in a single-blind fashion. Inhaled albuterol, oral prednisone, or inhaled beclomethasone was added as needed. Follow-up visits occurred 2 and 4 months after randomization and then at 4-month intervals.
The methodology of this study was strong; it had a prospective randomized design, concealed allocation, 98% follow-up for primary outcome, intention-to-treat analysis, and multivariate assessment of confounding. Lack of physician masking to treatment is a minor weakness. Of note, this was not a head-to-head comparison of budesonide with nedocromil, so clinicians should be cautious about inferring the superiority of budesonide over nedocromil.
* OUTCOMES MEASURED The primary outcome was the change in [FEV.sub.1] after a bronchodilator. Secondary outcomes included health services utilization such as hospitalization, symptom severity, airway responsiveness, physical growth, incidence of cataracts, and psychological development. Cost of treatment, side effects, and patient/parent satisfaction were not directly assessed.
* RESULTS The groups were similar at baseline. Children were followed for a mean of 4.3 years. Neither budesonide nor nedocromil significantly improved lung function more than placebo. Hospitalization rates decreased in all groups, but compared with placebo, patients receiving budesonide had significantly fewer hospitalizations (2.5 vs 4.4/100 person-years, or 1.9 hospitalizations prevented for 20 children treated for 5 years; P=.004), visits for urgent care (12 vs 22/100 person-years, or 10 urgent visits prevented for 20 patients treated for 5 years; P [is less than] .001), and courses of prednisone (70 courses vs 122/100 person-years, 52 courses prevented for 20 patients treated over 5 years; P [is less than] .001). Compared with the placebo group the nedocromil group had no significant difference in hospitalization rates but did have fewer urgent care visits (16 vs 22/100 personyears, or 5 fewer visits prevented for 20 patients treated over 5years; P [is less than] .02) and fewer prednisone courses (102 vs 122/100 patient years, or 20 fewer courses for 20 children treated for 5 years; P [is less than] .01) versus placebo. Children taking budesonide but not nedocromil recorded significantly fewer symptoms, less frequent use of albuterol, and more episode-free days than those receiving just placebo. Increase in height was significantly less for the budesonide group (22.7 cm vs 23.8 cm, P=.005), although there was no significant difference in overall growth velocity, Tanner stage, or projected final height among the 3 groups at the end of the treatment period.
RECOMMENDATIONS FOR CLINICAL PRACTICE
This study provides good evidence that inhaled budesonide or nedocromil may be given to all children with mild to moderate asthma to improve long-term control with little fear of long-term effects. Parents should be counseled that their child's growth may be slightly blunted, although the data offer some reassurance that final height will be normal. This study does not address the length of therapy, the management of patients with severe asthma, or the role of combination therapy.
Meri Feaver Stella, MD Warren Newton, MD, MPH University of North Carolina Chapel Hill E-mail: Warren_Newton@med.unc.edu
COPYRIGHT 2001 Appleton & Lange
COPYRIGHT 2001 Gale Group