ABSTRACT. Background: The primary goal of this study was to investigate hepatic fatty acid (FA) metabolism after severe thermal injury. Methods: Sixteen pigs were divided into control (n = 8) and burn (n = 8, with 40% full thickness total body surface area burned) groups. Catheters were inserted in the right common carotid artery, portal vein, and hepatic vein for blood sampling. Flow probes were placed around the hepatic artery and portal vein for blood flow measurements. Animals were given pain medication and sedated until the tracer study on day 4 after burn. The pigs were infused for 4 hours with U-1C, -palmitate in order to quantify hepatic FA kinetics and oxidation. Results: Liver triglyceride (TG) content was elevated from 162 16 (control) to 297 + 28 wmol TG/g dry liver wt. (p
similar between the 2 groups, as were malonyl-coenzyme A (CoA) levels and activities of acetyl-CoA carboxylase and adenosine monophosphate (AMP)-activated protein kinase. In contrast, incorporation of plasma-free fatty acids into hepatic TG was elevated (p
Fatty liver has been commonly observed after burn injury. More than 60% of autopsies of burned children showed liver fatty metamorphosis.1 Herndon et a12 reported that 100% of adult patients who died from severe burn developed fatty infiltration cholestasis and antemortem liver function abnormality. Liver weight can be doubled in as short as 15 to 30 days after burn, presumably reflecting fatty liver formation even in surviving patients. Animal studies indicate that fatty liver increases the risk for infectious complications, and therefore may be a causative factor in the development of postburn sepsis. In patients, liver size may become increased sufficiently to inhibit ventilation. The mechanism leading to increased fat accumulation in the liver after burn is unclear, since studies of fatty liver after burn injury have been limited to histologic observations. It was, therefore, our goal to clarify the mechanism responsible for the formation of fatty liver after burn.
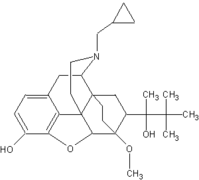
Under almost all conditions, the predominant source of hepatic triglyceride (TG) is free fatty acids (FFA) taken up from plasma.6 Accelerated hepatic TG formation can thus result from increased FFA uptake or increased channeling of fatty acids to TG within the liver. The most likely mechanism by which fatty acids would be channeled to TG within the liver is the inhibition of oxidation. In that light, the regulation of fatty acid oxidation in the liver is largely dictated by the activity of the carnitine palmityltransferase (CPT) enzyme system that is responsible for transfer of longchain fatty acids into the mitochondria. CPT is in turn regulated by malonyl CoA, which is formed by the addition of C02 to acetyl-coenzyme A (CoA) via the enzyme acetyl-CoA carboxylase (ACC).s The activity of ACC is dependent on its state of phosphorylation, which is regulated by adenosine monophosphate (AMP)-activated protein kinase (AMPK).9 To assess the effect of burn on hepatic fatty acid oxidation, we have quantified in vivo rates of FFA uptake and oxidation and related those rates to tissue measurements of the malonyl CoA-ACC-AMPK system.
Regardless of the rate of formation of hepatic TG, it will accumulate in the liver if it is not secreted at the rate at which it is produced. Thus, fatty liver after burn represents an imbalance between TG formation and excretion as very low density lipoprotein TG (VLDL-- TG). For that reason, in addition to quantifying the rates of fatty acid uptake and oxidation in the study, we have also quantified the rate of VLDL-TG secretion. This approach enables the evaluation of whether fatty liver results from altered interhepatic metabolism of fatty acids, or impaired mechanisms of secretion of TG.
CLINICAL RELEVANCY STATEMENT
Our results suggest that fat accumulation in the liver is part of the metabolic response to burn, irrespective of the nature of nutritional support. However, hepatic triglyceride accumulation can be minimized by providing nonprotein energy intake with a slightly hypocaloric amount of carbohydrate with lipid added only in sufficient quantity to avoid essential fatty acid deficiency.
METHODS
Sixteen Yorkshire swine were randomly divided into control (n = 8, 17.1 + 0.6 kg) and burned (n = 8, 18.0 0.8 kg) groups. The animals were studied in pairs. The study was approved by the Animal Care and Use Committee of the University of Texas Medical Branch (ACUC 98-04-029).
Experimental Procedures
The animals were preanesthetized with ketamine (10 mg/kg, IV), and anesthesia was maintained with 1.5% to 2.5% halothane. A midline laparotomy was performed with the necessary dissection to place perivascular flow probes (Transonic Animal Research Flowmeter, Transonic Systems Inc, Ithaca, NY) around the common hepatic artery and the portal vein. Care was taken to preserve the perivascular nerves. Catheters for collecting blood samples were inserted into the portal vein, hepatic vein, and right common carotid artery. A venous catheter was also inserted via the jugular vein for the infusion of resuscitation fluid, analgesia, and isotope tracers. A gastrostomy for feeding was performed through the anterior wall of the stomach, and the tip of the catheter was positioned in the distal part of the duodenum. All the catheters and flow probes were secured intraabdominally, tunneled, and secured again through a hole in the skin in the right caudal quadrant of the abdomen.
After the surgical procedures, deep anesthesia was maintained, and one-half of the animals were flame burned. An area of approximately 40% of total body surface was outlined, and a flame from a meeker burner was applied to the skin until it was contracted. The burner was then moved to a new skin area until the entire outlined area was burned. The full-thickness lesion of the burned skin was confirmed by histologic examination.
All the animals were placed in a sling and allowed to awaken (-2 hours). They remained in the sling until the end of the tracer infusion on day 4. Buprenex (0.3 mg IV) was used as needed for pain analgesia, and valium (10 mg IV) was given as needed to reduce agitation throughout the experiment. On day 1, burned pigs were resuscitated by infusion of lactate Ringer's, according to the Parkland formula,10 which is 4 mL x body weight (kg) x percentage of body burned, starting 60 minutes after the burn injury. One-half of the total resuscitation fluid was given in the first 8 hours post-- burn and the remainder over the next 16 hours. Afterwards, the burned pigs were maintained with resuscitation at 3 mL/kg per hour (as in the control group) until the end of the study.
Feeding started via the gastrostomy tube when the animals awakened from the surgery. Liquid diets, made from Vivonex (Sandoz Nutrition Corp, Minneapolis, MN), polycose (as carbohydrate supplement), and ProMOD (protein supplement; Ross Products Division, Abbott Laboratories, Inc, Columbus, OH), according to standard daily ration of minipig grower diet from Purina Mills Inc (St. Louis, MO), was infused via vented pumps (Kangaroo; Sherwood Medical Co, Plano, TX). Feeding was maintained continuously until the end of isotope tracer infusion study on day 4.
Mean arterial pressure, mean pulmonary artery pressure, heart rate, and body temperature were monitored continuously and recorded every 4 hours throughout the entire study. Blood gas, cardiac output, urine output, and blood flow rates in the hepatic artery and portal vein were measured every 4 hours throughout the entire study.
Tracer Infusion Protocol
The isotope infusion was performed on day 4 after burn injury. After baseline blood samples from the hepatic artery, portal vein, and hepatic vein were collected, a 4-hour continuous infusion of U-13C 16-palmitate (0.08 wmol/kg per minute in control and 0.16 lmol/kg per minute in burn) was started with NaH 13 C03 prime (100 v,mol/kg in control and 150 p,mol/kg in burn). Blood samples were taken from artery, portal vein, and hepatic vein simultaneously at 60- (3 mL each), 120- (3 mL each), 180- (3 mL each), 195- (6 mL each), 210- (6 mL each), 225- (6 mL each), and 240-minute (6 mL each) intervals. After the last blood samples were taken, liver biopsy samples were taken rapidly after anesthetization and frozen with aluminum block tongs at liquid nitrogen temperature. Afterwards, animals were killed with ketamine followed by a solution of saturated potassium chloride. The liver was removed, weighted (439.5 13.4 g in control and 491 10.1 g in burn), and stored at -80'C freezer. The isotope infusion was then stopped.
Blood Flow Measurement
Blood flows in hepatic artery and portal vein were measured using ultrasonic blood flow meters (Transonic Systems, Ithaca, NY). The flow probes (Transonic Animal Research Flowmeter, Transonic Systems) were placed around the common hepatic artery and portal vein during the day 1 surgical procedure. Blood flow in the hepatic vein was calculated as the sum of blood flows in the hepatic artery and the portal vein. Plasma flow was calculated by multiplying blood flow by 1 the hematocrit.
DISCUSSION
Accumulation of fat in the liver is a consistent autopsy finding in patients who die from severe burn injury. 3 In the current study, we found that liver TG was almost doubled in only 4 days after injury, thereby indicating that the process of fatty infiltration of the liver begins well before the agonal phase before death. Rather, the enlarged livers common in most severely burned patients3 likely reflect a persistent accumulation of TG throughout hospitalization. Studies in animals indicate that hepatic fat accumulation decreases resistance to bacterial challenge, and therefore can be a significant factor contributing to morbidity and mortality.4-5,16-17
An accumulation of TG in the liver results from an imbalance between formation and secretion in the form of VLDL-TG. Such an imbalance could result from an altered metabolism of fatty acids within the liver or an impaired secretion. In this study, we investigated the hypothesis that fatty acids taken up by the liver were channeled to TG because of a deficiency in hepatic fatty acid oxidation. However, we found hepatic fatty acid oxidation to be normal in the burned animals. Consistent with the kinetic observation, we found no changes in hepatic malonyl CoA or the factors regulating malonyl CoA content. Nonetheless, we found a significant increase in the rate of TG synthesis from plasma FFA in the burned animals. Since there was no difference between groups in the availability of fatty acids for TG synthesis (ie, uptake-oxidation), the accelerated TG formation in the burned animals reflected a specific stimulation of the synthetic pathway.
We performed this experiment in the fed state to model the clinical situation, in that patients are virtually constantly always fed. The pigs were fed a highcarbohydrate diet, as per the optimal growing chow for normal pigs. It is likely this persistent high-carbohydrate intake suppressed lipolysis and thus delivery of fatty acids to the liver. In the basal state, elevated lipolysis has been well-documented in animals and humans after burn injury.16,18-21 Thus, it is possible that if the animals had been studied in the fasted state and delivery of fatty acids to the liver of the burned animals had been increased to a greater extent than in control animals, then hepatic TG synthesis would have increased simply because of increased availability of precursor. However, such an increased synthesis would not be the result of altered hepatic fatty acid metabolism.
It is also possible that the high carbohydrate diet increased fatty acid synthesis, and thereby hepatic TG. However, it is likely that any contribution of de novo fatty acid synthesis to hepatic TG was minor. First, we found no difference between groups in malonyl CoA concentrations, and malonyl CoA is an important intermediate in the de novo synthesis of fatty acids. Also, we gave the diet in accord with normal caloric requirements. This means that the diet was somewhat hypocaloric for the burned animals, since metabolic rate is stimulated by the presence of a major burn.2 Whole body fat synthesis does not occur when caloric requirements are not met, even with pure carbohyate.21,22 Even when hypercaloric amounts of carbohydrate are provided, hepatic de novo synthesis is not extensive. We previously found in normal volunteers that only 1% of hepatic TG synthesis came from de novo synthesis in the basal state, and even after 4 days of continuous feeding of carbohydrate at 50% above caloric requirement, only 21% of hepatic TG synthesis came from de novo synthesized fatty acids.22 Similarly, in burn patients receiving large amounts of carbohydrate and insulin therapy, fatty acids released peripherally were the major source of TG synthesized in the liver.23 Thus, whereas it is possible that under some clinical conditions accelerated de novo fatty acid synthesis can occur, under the conditions of our experiment we have no evidence that this was a major source of hepatic TG formation.
The impairment of TG secretion from the liver appeared to be the principle mechanism responsible for the increased hepatic TG content. Liver TG are secreted predominantly in the form of VLDL-TG. Under normal conditions, an increase in lipolysis and hepatic fatty acid uptake that causes increased TG production (eg, due to exercise) is balanced by an increased rate of VLDL-TG secretion so that TG accumulation does not occur. A number of factors can potentially limit the secretion of VLDL-TG. A deficiency in apo-B, a protein involved in packaging the VLDL-TG, is one possibility, since a general protein catabolic state exists after burn.24-25 Another possibility is that there was a choline deficiency after burn. Choline is a precursor of phosphatidylcholine synthesis, which is an important component of VLDL and has been reported to play an important role in secretion of VLDL-TG. We have found that plasma choline concentration was significantly lower in burned patients (3.96 0.5 lmol/L) (unpublished results), and choline deficiency is known to cause fatty liver.26-27 However, it has yet to be determined if choline supplementation will increase VLDL-TG secretion after burn.
Despite the decrease in the secretion of VLDL-TG after burn, the plasma concentration of VLDL-TG was significantly elevated due to impaired peripheral clearance. In fact, it is possible that the impaired peripheral clearance contributed to the reduced VLDL-TG secretion, if secretion rate is responsive to the prevailing plasma concentration. The impaired VLDL-TG clearance probably resulted from a decreased activity of lipoprotein lipase (LPL). LPL is the endothelial-bound enzyme that hydrolyzes circulating TG in order for tissues to take up fatty acids. A decreased LPL activity in adipose tissue has been reported in gram-negative septic rats and critically ill patients.21-31 Similarly, Rouzer and Cerami 32 found a deficient lipase activity in postheparin plasma in infected rabbits with elevated VLDL-TG concentration. To the contrary, Verschoor et al 133 found that VLDL-TG clearance was unrelated to changes in adipose LPL activity in rats, and no data directly address the effect of burn on LPL activity. Thus, although a decrease in clearance would be expected to follow from a decreased activity of LPL, the role for changes in LPL activity in our study remains speculative.
The major clinical implication of our findings relates to the source and amount of nonprotein calories provided after severe burn. Our results suggest that, to at least some extent, fat accumulation in the liver is part of the metabolic response to burn, irrespective of the diet. This is consistent with the correlation found in seriously ill patients between the severity of disease and the extent of fatty infiltration of the liver rather than the nature or amount of nutrition support provided.34 On the other hand, since TG produced in the liver after burn is not readily exported, anything that promotes hepatic TG formation would be expected to further augment TG storage. Thus, both excessive carbohydrate intake sufficient to stimulate hepatic lipid synthesis, or excessive lipid intake that would increase delivery of fatty acids to the liver, would be expected to increase the amount of hepatic TG. Thus, only by ensuring that total caloric intake is minimized can hepatic TG not be increased by nutrition support. Even in the circumstance of hypocaloric feeding, however, hepatic TG accumulation would be expected to occur, owing to a high rate of lipolysis, an accelerated incorporation of plasma FFA into TG, and an impaired rate of secretion of VLDL-TG. In that regard, it would be expected that a hypocaloric amount of carbohydrate intake might actually limit hepatic TG formation, as peripheral lipolysis would be reduced and de novo lipid synthesis from the carbohydrate would be minimal. Thus, one can predict from these findings that the optimal nonprotein energy intake in burn injury insofar as minimizing hepatic TG would be to provide a slightly hypocaloric amount of carbohydrate with lipid added only in sufficient quantity to avoid essential fatty acid deficiency. Regardless of the nature of nutrition support, however, hepatic TG accumulation is likely to occur unless the inhibition of hepatic VLDL-TG secretion can be overridden.
ACKNOWLEDGMENTS
This investigation was supported by National Institutes of Health grant DK34871 and Shriners Hospital grants 8450 and 8490.
REFERENCES
1. Linares HA: A report of 115 consecutive autopsies in burned children: 1966-1980. Burns 8:263-270, 1981
2. Herndon DN, Stein MD, Rutan TC, et al: Failure of total parenteral nutrition (TPN) supplementation to improve liver function, immunity, and mortality in thermally injured patients. J Trauma 27:195-204, 1987
3. Aarsland A, Chinkes DL, Wolfe RR, et al: Beta-blockade lowers peripheral lipolysis in burn patients receiving growth hormone. Ann Surg 223:777-789, 1996
4. Hirsch RL, McKay DG, Travers RI: Hyperlipidemia, fatty liver and bromsulfophthalein retention in rabbits injected with bacterial endotoxin. J Lipid Res 5:563-568, 1976
5. Yang SQ, Lin HZ, Lane MD, et al: Obesity increases sensitivity to endotoxin liver injury: Implications for the pathogenesis of steatohepatitis. Proc Natl Acad Sci USA 94:2557-2562, 1997
6. Aarsland A, Wolfe RR: Hepatic secretion of VLDL fatty acids during stimulated lipogenesis in man. J Lipid Res 39:12801286, 1998
7. McGarry JD, Mills SE, Long CS, et al: Observations on the affinity of carnitine, and malonyl-CoA sensitivity of carnitine palmitoltransferase I in animal and human tissues. Biochem J 214:21-28, 1983
8. Robinson IN, Zammit VA: Sensitivity of carnitine acyltransferase I to malonyl-CoA inhibition in isolated rat liver mitochondria is quantitatively related to hepatic malonyl-CoA concentration in vivo. Biochem J 206:177-179, 1982
9. Winder WW, Hardie DG: Inactivation of acetyl-CoA carboxylase and activation of AMP-activated protein kinase in muscle during exercise. Am J Physiol 270:E299-E304, 1996
10. Baxter C: Fluid volume and electrolyte changes of the early postburn period. Clin Plast Surg 1:693-709, 1974
11. Martini WZ, Irtun 0, Chinkes DL, et al: Glucose effects on lung surfactant kinetics in conscious pigs. Am J Physiol 279:E920E926, 2000
12. Uji Y, Noma A, Shiraki M, et al: Separation and quantitation of plasma free fatty acids as phenacyl esters by HPLC. Biomed Chromatogr 2:110-114, 1987
13. McGarry JD, Stark MJ, Foster DW: Hepatic malonyl-CoA levels of fed, fasted and diabetic rats as measured using a simple radioisotope assay. J Biol Chem 253:8291-8293, 1978 14. Rasmussen BB, Winder WW: Effect of exercise intensity on skeletal muscle malonyl-CoA and Acetyl-CoA carboxylase. J Appl Physiol 83:1104-1109, 1997
15. Frayn, KN, Maycock PF: Skeletal muscle triacylglycerol in the rat: Methods for sampling and measurement, and studies of biological variability. J Lipid Res 21:139-144, 1980
16. Mittendorfer B, Jeschke MG, Wolf SE, et al: Nutritional hepatic steatosis and mortality after burn injury in rats. Clin Nutr 17:293-299, 1998
17. Frayn KN: Are plasma non-esterified fatty acid concentrations a risk marker for coronary heart disease and other chronic diseases? Clin Scien 90:243-253, 1993
18. Goodenough, RD, Wolfe RR: Effect of total parental nutrition on free fatty acid metabolism in burned patients. JPEN 8:357-360, 1983
19. Wolfe RR, Herndon DN, Peters EJ, et al: Regulation of lipolysis in severely burned children. Ann Surg 206:214-221, 1987
20. Wolfe RR, Herndon DN, Jahoor F, et al: Effect of severe burn injury on substrate cycling by glucose and fatty acids. N Engl J Med 317:403-408, 1987
21. Wolfe RR, Peters EJ: Lipolytic response to glucose infusion in human subjects. Am J Physiol 252:E218-E223, 1987
22. Aarsland A, Chinkes DL, Wolfe RR: Contribution of de novo synthesis of fatty acid and lipolysis to VLDL secretion during prolonged hyperglycemia/hyperinsulinemia in normal man. J Clin Invest 98:2008-2017, 1996
23. Aarsland A, Chinkes DL, Sakurai Y, et al: Insulin therapy in burn patients does not contribute to hepatic trigylceride production. J Clin Invest 101:2233-2239, 1998
24. Hart DW, Wolf SE, Mlcak R, et al: Persistence of muscle catabolism after severe burn. Surgery 128:312-319, 2000
25. Marcos E, Mazur A, Cardot P, et al: Serum apolipoprotein B and A-I and naturally occurring fatty liver in dairy cows. Lipids 25:575-577, 1990
26. Yamamoto A, Sano M, Isozaki M: Studies on phosphalipid metabolism in choline deficient fatty liver. J Biochem 65:85-91, 1969
27. Nolan JP, Vilayat M: Endotoxin and the liver. I. Toxicity in rats with choline deficient fatty livers. Proc Soc Exp Biol Med 129: 29-31, 1968
28. Alvares C, Ramos A: Lipids, lipoproteins, and apoproteins in serum during infection. Clin Chem 32:142-145, 1986
29. Grundy SM: Hypertriglyderidemia: Mechanisms, clinical significance, and treatment. Med Clinics North Am 66:519-535, 1982 30. Lanza-Jacoby S, Lansey SC, Cleary MP, et al: Alterations in
lipogenic enzymes and lipoprotein lipase activity during gramnegative sepsis in the rat. Arch Surg 117:144-147, 1982
31. Liao W: Endotoxin, cytokines, and hyperlipidemia. Scand J Gastroenterol 28:97-103, 1993
32. Rouzer CA, Cerami A: Hypertriglyceridemia associated with Trypanpsoma Brucei brucei infection in rabbits: Role of defective triglyceride removal. Mol Biochem Parasitol 2:21-38, 1980
33. Verschoor L, Chen YI, Reaven GM: In search of a relationship between physiologically-induced variations in adipose tissue lipoprotein lipase activity and very low density lipoprotein kinetics in normal rats. Metabolism 31:499-503,1982
34. Wolfe BM, Walker BK, Shaul DB, et al: Effect of TPN on hepatic histology. Arch Surg 123:1084-1090, 1988
Wenjun Z. Martini, PhD; Oivind Irtun, MD; David L. Chinkes, PhD; Blake Rasmussen, PhD; Daniel L. Traber, PhD; and Robert R. Wolfe, PhD
From the Shriners Burns Hospital and the Departments of Surgery and Anesthesiology, The University of Texas Medical Branch, Galveston
Received for publication, February 9, 2001. Accepted for publication, June 25, 2001.
Correspondence: Robert R Wolfe, PhD, Chief of Metabolism, Shriners Burns Hospital, 815 Market Street, Galveston, TX 77550.
Copyright American Society for Parenteral and Enteral Nutrition Nov/Dec 2001
Provided by ProQuest Information and Learning Company. All rights Reserved