Controlling Pain
QUESTION: I care for many patients with moderate to severe pain. With so many opioids available, how can I determine which type suits a patient best? ANSWER: Understanding how and why each opioid type works will help you make the best choice for your patient. Opioids available in the United States fall into two main groups: the morphine-like mu agonists (also called pure or full agonists) and agonist-antagonists. An agonist is a drug that binds to one of the opioid receptor sites involved in analgesia (mu, delta, or kappa). An antagonist also binds to an opioid receptor, but without causing analgesia. Because it competes with an agonist for the binding site, an antagonist reduces the agonist's ability to provide analgesia. A closer look at mu agonists The largest and most commonly prescribed group of opioids, mu agonists are the mainstay of analgesia for moderate to severe acute pain, breakthrough pain (intermittent episodes of increased pain), and cancer pain, and are increasingly used for chronic nonmalignant pain.
Mu agonists have no ceiling on their analgesia and produce comparable analgesia if doses are adjusted appropriately. However, certain mu agonists such as meperidine should be avoided because of active metabolites. Others, such as codeine, should be reserved for mild to moderate pain only because of adverse effects at higher doses.
Combining a mu agonist with a nonopioid or adjuvant analgesic can improve pain control and may allow a reduction in opioid dose, thus minimizing opioid-related adverse effects, such as oversedation, respiratory depression, and constipation.
Using agonist-antagonists
Agonist-antagonists aren't recommended as first-line drugs for pain. Drawbacks include limited routes of administration and a ceiling for pain relief. Once the analgesic ceiling is reached, dosage increases won't increase analgesia, so these drugs aren't appropriate for severe, escalating pain. They also may reverse the analgesia of mu agonists or precipitate withdrawal in patients who are physically dependent on mu agonists.
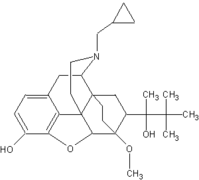
Agonist-antagonists can be subdivided into two groups: mixed agonist-antagonists, such as butorphanol (Stadol) and pentazocine (Talwin), and the only partial agonist available in the United States, buprenorphine (Buprenex).
Administer opioids by the least invasive and safest route that's effective. The dose should be titrated to achieve effective pain relief with minimal or acceptable adverse effects. If the patient has unacceptable and unmanageable adverse effects, switch to another opioid. As a rule, use only one route of opioid administration at a time; make the oral route your first choice, when possible, because of its safety, convenience, and price.
SELECTED REFERENCE
McCaffery, M., and Pasero, C.: Pain: Clinical Manual, 2nd edition. St. Louis, Mo., Mosby, Inc., 1999.
BY MARGO MCCAFFERY, RN, MS, FAAN
Consultant in the Nursing Care of Patients with Pain * Los Angeles, Calif.
Copyright Springhouse Corporation Oct 2001
Provided by ProQuest Information and Learning Company. All rights Reserved