The 1999 Federal regulations extend the treatment options of methadone-maintained opioid-dependent patients from specialized clinics to office-based opioid therapy (OBOT). OBOT allows primary care physicians to coordinate methadone therapy in this group with ongoing medical care. This patient group tends to be poorly understood and underserved. Methadone maintenance therapy is the most widely known and well-researched treatment for opioid dependency. Goals of therapy are to prevent abstinence syndrome, reduce narcotic cravings and block the euphoric effects of illicit opioid use. In the first phase of methadone treatment, appropriately selected patients are tapered to adequate steady-state dosing. Once they are stabilized on a satisfactory dosage, it is often possible to address their other chronic medical and psychiatric conditions. The maintenance phase can be used as a long-term therapy until the patient demonstrates the qualities required for successful detoxification. Patients who abuse narcotics have an increased risk for human immunodeficiency virus infection, hepatitis, tuberculosis and other conditions contributing to increased morbidity and mortality. Short- or long-term pain management problems and surgical needs are also common concerns in opioid-dependent patients and are generally treatable in conjunction with methadone maintenance. (Am Fam Physician 2001;63:2404-10.)
Opioid dependence is a chronic, often relapsing, disorder that contributes to major medical challenges such as human immunodeficiency virus (HIV)-related illnesses, hepatitis and other chronic diseases.(1-3) While opioid-dependent patients are generally treated within rehabilitation programs that specifically target their addiction, family physicians, with their emphasis on regular and ongoing health maintenance, have the opportunity to treat a patient's addiction as well as other medical concerns.(4,5) Major issues in the medical management of opioid dependency are outlined in Table 1.
Epidemiology
Between 500,000 and 1 million Americans are believed to be opioid dependent at any point in time.(2,6,7) Gender differences exist, with opioid-related disorders more prevalent in men than women by a ratio of up to 4:1.2,(8) Opioid dependency is often linked to a history of drug-related criminal activity.(2) Antisocial personality disorder is more prevalent in opioid-dependent persons than in the general population,(2,8,9) and opioid-dependent persons frequently have coexisting mood disorders, especially depression.(2,4,9)
Treatment Options for Opioid Dependence
Methadone is the most widely known pharmacologic treatment for opioid dependence and is effective in reducing illicit narcotic use,(10-12) retaining patients in treatment and decreasing illegal drug use.(11,12) Ongoing methadone maintenance decreases the risk of contracting and transmitting HIV, hepatitis B (HBV) and hepatitis C (HCV)(13,14) and is considered a cost-effective intervention.(15) Long-term methadone maintenance is more successful in averting relapse than shorter-term treatment.(12)
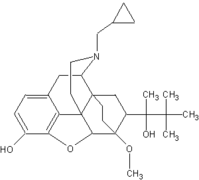
Alternatives to methadone therapy include levomethadyl (Orlaam), buprenorphine (Buprenex), naltrexone (Trexan) and Narcotics Anonymous (NA). Levomethadyl's efficacy lasts as long as three days, while methadone requires daily dosing. Thus, levomethadyl therapy is appropriate in patients who do not require intensive care, but it is less effective in those who need daily monitoring. Buprenorphine (available for investigational use only) demonstrates dose-response ceiling effects, a factor that may operate as a safeguard and limit the potential for abuse or diversion.(16) Methadone produces better treatment retention rates than buprenorphine,(17,18) although results of studies of its superiority in decreasing illicit narcotic use are mixed.(17-19) In contrast to methadone, naltrexone produces no physical dependence but has poor patient compliance rates. NA, a nonpharmacologic intervention, is a self-help peer recovery group that provides social support.
Appropriate Candidates for Methadone Therapy
Federal regulations stipulate that to be eligible for methadone maintenance therapy, patients must demonstrate at least a one-year history of physiologic dependence on a narcotic and meet the minimum age requirement of 18 years. However, an exception is available for patients between the ages of 16 and 18 who present with a documented history of at least two prior unsuccessful detoxification efforts and have parental consent.(20) Specific criteria for opioid dependence are listed in Table 2. Identifying opioid dependence is relatively straightforward when patients are candid about their symptoms and actively request treatment of addiction. Unfortunately, not all patients are forthcoming about their condition.
The physician needs to be alert to signs of drug-seeking behavior or evidence of a recent relapse in a formerly addicted patient. Both of these situations warrant further assessment to establish whether current opioid dependence exists. Warning signs of possible drug seeking include a pattern of behavior in which a patient finishes narcotic prescriptions early, insists on replacement prescriptions and concurrently solicits prescriptions from multiple physicians. Evidence of a short-term relapse is perhaps best characterized by opioid intoxication (e.g., pupillary constriction, drowsiness, slurred speech, impaired attention or memory).(2)
Traditionally, methadone maintenance is managed through dedicated clinics, which provide dosing and a broad array of counseling and rehabilitative services. Methadone maintenance programs currently exist in 42 states, the District of Columbia, Puerto Rico and the U.S. Virgin Islands. These treatment programs are listed in the Narcotic Treatment Program Directory.(21) Physicians can access this resource on the Internet to locate a nearby methadone clinic and obtain referral information for a prospective patient (Table 3). The cost of treatment in a methadone maintenance program averages $4,500 annually and is sometimes subsidized by private insurance or Medicaid.
Another treatment option is dispensing methadone through a general medical practice. In this circumstance, a physician provides methadone pharmacotherapy contingent on registration with the Drug Enforcement Administration, the U.S. Food and Drug Administration and the state methadone authority. Physicians and patients must comply with methadone maintenance program requirements. This is a useful treatment option for patients who have limited access to specialized clinics, especially those who live in rural areas. Nevertheless, the burden of the federal and state requirements make this option unpopular with physicians. Moreover, this form of treatment is as restrictive to patients as traditional methadone clinic care.
Recent changes in the Federal regulations advocate less restrictive alternatives, highlighting an increasing interest in providing care outside of traditional methadone clinics as a means of extending access to narcotic addiction treatment. Federal regulations established in 1999 endorse office-based opioid therapy (OBOT), in which primary care physicians provide methadone pharmacotherapy within comprehensive medical care for a segment of the methadone-maintained population.(22)
To practice OBOT, physicians must have training in addiction medicine, be affiliated with a methadone clinic or be monitored by the medical director of a methadone clinic. Physicians may incorporate up to 30 methadone-maintained patients into their practice. Eligible patients are referred exclusively from methadone clinics and must be stabilized and have achieved three years of successful methadone maintenance. The advantage of OBOT to patients is the fact that primary care physicians can dispense up to a 30-day supply of methadone, thus easing the scheduling demands characteristic of traditional methadone clinics.
Some research suggests that methadone treatment from a general medical practice is as effective as that provided in specialty clinics.(5) Office-based methadone treatment is currently in operation in other countries.(23)
Methadone Dosing and Maintenance
The goals of the early induction dosages of methadone are to attenuate withdrawal symptoms, diminish opioid craving and arrive at a tolerance threshold, while preventing euphoria and sedation from overmedication.(24-26) Initial daily dosages of 20 to 30 mg are usually safe and appropriate.(24,25) Because of the long half-life of methadone, between four and 10 days are necessary to achieve steady-state maintenance dosing.
Subsequent induction dosages are adjusted on the basis of dose response, particularly an evaluation of abstinence symptoms. The maintenance phase of dosing is attained when the patient's dosage is satisfactory and effective for at least 24 hours. The length of the maintenance phase lasts as long as treatment benefits the patient. Periodic dosage increases are warranted in cases of patients who relapse or abuse other drugs. For example, because alcohol, barbiturates and sedative-hypnotics accelerate methadone metabolism, they foster withdrawal symptoms. In addition, patients sometimes need a dosage increase when taking prescribed medicines (e.g., rifampin [Rifadin], phenytoin [Dilantin], carbamazepine [Tegretol]) that speed methadone metabolism.(3,25)
Detoxification
Detoxification is indicated when a patient demonstrates consistent, long-term abstinence and possesses adequate supportive resources (e.g., productive use of time, a stable home life). Patient receptiveness to community resources for opiate addicts, such as NA, is a good sign. NA is a useful tool in relapse prevention. Local chapters of NA are listed in the telephone book. Further resources are provided in Table 3.
Methadone detoxification involves the induction of opioid withdrawal symptoms and typically refers to either a short- or a long-term process. Short-term detoxification does not exceed 30 days.(20) Long-term detoxification lasts from 31 to 180 days. Gradual detoxification tends to be more successful than a sudden dose discontinuation.(6) Detoxification is difficult for the physician to manage because some opiate withdrawal symptoms are subjective and thus are hard to accurately assess. The physician runs the risk of either overestimating or underestimating the intensity of withdrawal.
For these reasons, detoxification must be undertaken on a case-by-case basis. Generally, it is a good idea to taper the methadone level to a low dose (e.g., 10 mg) before initiating adjunct medications, a process that prepares the patient for the final tapering of methadone.(27) Clonidine demonstrates some success in controlling early withdrawal symptoms.(4,8,27) Between 0.3 and 0.5 mg per day of clonidine is appropriate in the first few days, either in divided doses or using the transdermal delivery system. Pain and discomfort are best managed with nonnarcotic agents. If diarrhea develops, it is helpful to recommend loperamide (Immodium) in a dosage of 2 mg following each loose stool over a few days until stools are formed. For insomnia, a short course of hypnotics may be appropriate.
Medical Conditions During Methadone Therapy
Opioid-dependent patients undergoing methadone treatment are susceptible to a number of medical problems. They may also experience unusual manifestations or require specific modifications to therapy for a wide range of health problems. Because some of these conditions or diseases are communicable (e.g., HIV, hepatitis, tuberculosis), it is critical that the physician encourage a dialog between the patient and family members to avert further disease transmission. Moreover, it is helpful for the physician to act in an instructive capacity and educate family members, especially partners, about the chronic, often relapsing, course of opioid dependence. Physicians should urge family members to make use of the support services, resources and information listed in Table 3, particularly Nar-Anon, a self-help support group for family members of addicts.
HIV INFECTION
The prevalence of HIV infection is as high as 60 percent in opioid-dependent persons.(2,6) In addition to the burdens of its own clinical course, HIV worsens the prognosis for other infectious diseases such as hepatitis and tuberculosis.(2) It is critical to offer HIV counseling and testing, and to stress avoidance of high-risk behaviors. Retesting is warranted six months after any possible HIV exposure.
HIV-seropositive status requires a medical evaluation, including a physical examination, a baseline CD4 T-lymphocyte count, viral load and tuberculin skin tests, and an update of the patient's immunizations.(3,28) Based on the results, family physicians should explain the merits of antiviral therapy.
HEPATITIS
Opioid-dependent patients are at increased risk for HBV and HCV infection. In this population group, HBV infection rates are approximately 60 to 80 percent,(3,29) and HCV is even more prevalent.(29,30) It is important to screen patients to distinguish those who have acute infection, chronic carrier status, undetected symptomatic chronic active disease or negative status.(2,3) HBV screening should include an analysis of the antihepatitis core antibody, hepatitis surface antigen and surface antibody blood test results.(3) Patients with active HBV infection require liver function tests and further medical evaluation. Those whose core antibody, surface antigen and surface antibody test results are negative are candidates for HBV vaccination. HCV screening should include the anti-HCV antibody test. Patients with active HCV infection should be evaluated for antiviral treatment.
TUBERCULOSIS
An increase in tuberculosis cases in this country is attributed to both new infection and reactivation of latent infections in HIV-seropositive intravenous drug users.(2,3) Federal regulations require that patients receive tuberculosis screening, using the Purified Protein Derivative (PPD) skin test, when they are admitted to a methadone clinic, unless they have documented seropositive status, and annually thereafter as long as they remain seronegative.(20) Physicians should evaluate the need for treatment or prophylaxis in patients with positive PPD test results.
PAIN MANAGEMENT AND SURGICAL PROCEDURES
A common misconception in evaluating pain is that a patient maintained on a stable dosage of methadone does not require additional pain relief for a medical or surgical procedure.(24) Methadone-maintained patients are often tolerant to their dosage, however, and receive no analgesic effect. General guidelines for treating acute pain in these patients include continuing daily methadone maintenance at the prescribed dosage. It is also reasonable to divide a patient's dose in half and administer one half intramuscularly before a surgical procedure and the other half afterward.
Physicians should refrain from temporarily increasing a methadone dose to combat acute pain because this practice only affords six hours of pain relief.
Nonnarcotic agents should be considered the first option for the treatment of pain. If nonnarcotic analgesics are inadequate in managing acute pain, it is appropriate to prescribe short-acting opioid agonists. The latter should be prescribed in larger and more frequent doses (because of cross-tolerance) than would usually be the case. Short-acting opioid agonists should be prescribed in conjunction with (not in lieu of) ongoing methadone maintenance. However, it is critical to avoid prescribing the following mixed opioid agonist-antagonists: pentazocine (Talwin), butorphanol (Stadol), nalbuphine (Nubain) and buprenorphine. Because of their partial opiate antagonist effect, these drugs induce opioid withdrawal. As soon as feasible, patients should be switched to nonnarcotic analgesics.
Chronic pain is more difficult to treat than acute pain in this population. These patients typically have a history of multiple surgical procedures, unsuccessful pain treatment and increased drug abuse. Despite prior treatment failures, referral to a pain clinic is often helpful. Pain clinics offer a broad spectrum of interventions to address chronic pain syndromes. Adjunctive therapies such as biofeedback, acupuncture, behavioral management and neuroablative procedures are often available at such clinics.
REFERENCES
(1.) Dole VP. What is "methadone maintenance treatment"? J Maintenance Addict 1997;1:7-8.
(2.) American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, D.C.: American Psychiatric Association, 1994:175-255.
(3.) Neshin S. HIV and other infectious diseases. In: Parrino MW. State methadone treatment guidelines. Rockville, Md.: U.S. Department of Health and Human Services, Public Health Service, Substance and Mental Health Services Administration, Center for Substance Abuse Treatment. Treatment improvement protocol (TIP) series, 1993; DHHS publication no. (SMA) 93-1991:95-118.
(4.) Sullivan E, Fleming M. A guide to substance abuse services for primary care clinicians. Rockville, Md.: U.S. Department of Health and Human Services, Public Health Service, Substance and Mental Health Services Administration, Center for Substance Abuse Treatment, 1997; DHHS publication no. 97-3139:1-48.
(5.) Byrne A, Wodak A. Census of patients receiving methadone treatment in a general practice. Addict Res 1996;3(4):341-9.
(6.) Nadelmann E, McNeely J. Doing methadone right. Public Interest 1996;Spring(N123):83-93.
(7.)National Institute on Drug Abuse. Heroin abuse and addiction. Rockville, Md.: U.S. Department of Health and Human Services, National Institutes of Health, National Institute on Drug Abuse 2000. Research report series; NIH publication no. 00-4165.
(8.) Maxmen JS, Ward NG. Substance-related disorders. In: Essential psychopathology and its treatment. 2d ed. New York: Norton, 1995:132-72.
(9.) Mason BJ, Kocsis JH, Melia D, Khuri ET, Sweeney J, Wells A, et al. Psychiatric comorbidity in methadone maintained patients. J Addict Dis 1998;17:75-89.
(10.) Aszalos R, McDuff DR, Weintraub E, Montoya I, Schwartz R. Engaging hospitalized heroin-dependent patients into substance abuse treatment. J Subst Abuse Treat 1999;17:149-58.
(11.) Abbott PJ, Moore B, Delaney H, Weller S. Retrospective analyses of additional services for methadone maintenance patients. J Subst Abuse Treat 1999;17:129-37.
(12.) Sees KL, Delucchi KL, Masson C, Rosen A, Clark HW, Robillard H, et al. Methadone maintenance vs 180-day psychosocially enriched detoxification for treatment of opioid dependence: a randomized controlled trial. JAMA 2000;283:1303-10.
(13.) Stenbacka M, Leifman A, Romelsjo A. The impact of methadone on consumption of inpatient care and mortality, with special reference to HIV status. Subst Use Misuse 1998;33(14):2819-34.
(14.) Stark K, Bienzle U, Vonk R, Guggenmoos-Holzmann I. History of syringe sharing in prison and risk of hepatitis B virus, hepatitis C virus, and human immunodeficiency virus infection among injecting drug users in Berlin. Int J Epidemiol 1997;26(6): 1359-66.
(15.) Barnett PG. The cost-effectiveness of methadone maintenance as a health care intervention. Addiction 1999;94(4):479-88.
(16.) Walsh SL, Preston KL, Bigelow GE, Stitzer ML. Acute administration of buprenorphine in humans: partial agonist and blockade effects. J Pharmacol Exp Ther 1995;274:361-72.
(17.) Fischer G, Gombas W, Eder H, Jagsch R, Peternell A, Stuhlinger G, et al. Buprenorphine versus methadone maintenance for the treatment of opioid dependence. Addiction 1999;94:1337-47.
(18.) Kosten TR, Schottenfeld R, Ziedonis D, Falcioni J. Buprenorphine versus methadone maintenance for opioid dependence. J Nerv Ment Dis 1993;181: 358-64.
(19.) Oliveto AH, Feingold A, Schottenfeld R, Jatlow P, Kosten TR. Desipramine in opioid-dependent cocaine abusers maintained on buprenorphine vs methadone. Arch Gen Psychiatry 1999;56:812-20.
(20.) Code of Federal Regulations. Food and drugs. Human services, part 291--drugs used for treatment of narcotic addicts. U.S. Government Printing Office via GPO Access; cite 21CFR291.505:157-78.
(21.) U.S. Food and Drug Administration. FDA narcotic treatment programs directory. Rockville, Md.: U.S. Department of Health and Human Services, Public Health Service, Food and Drug Administration, 1995.
(22.) Code of Federal Regulations. Food and drugs. Human services, part 291--narcotic drugs in maintenance and detoxification treatment of narcotic dependence. U.S. Government Printing Office via GPO Access; cite 21CFR291.
(23.) Matheson C, Bond CM, Hickey F. Prescribing and dispensing for drug misusers in primary care: current practice in Scotland. Fam Pract 1999;16(4):375-9.
(24.) Kauffman JF, Woody GE. Matching treatment to patient needs in opioid substitution therapy. Rockville, Md.: U.S. Department of Health and Human Services, Public Health Service, Substance and Mental Health Services Administration, Center for Substance Abuse Treatment. Treatment improvement protocol (TIP) series, 1995; DHHS publication no. (SMA) 95-3049:1-46.
(25.) Payte JT, Khuri ET. Principles of methadone dose determination. In: Parrino MW. State methadone treatment guidelines. Rockville, Md.: U.S. Department of Health and Human Services, Public Health Service, Substance aand Mental Health Services Administration, Center for Substance Abuse Treatment. Treatment improvement protocol (TIP) series, 1993; DHHS publication no. (SMA) 93-1991:47-58.
(26.) Martin J, Payte JT, Zweben JE. Methadone maintenance treatment: a primer for physicians. J Psychoactive Drugs 1991;23(2):165-76.
(27.) Janiri L, Mannelli P, Persico AM, Serretti A, Tempesta E. Opiate detoxification of methadone maintenance patients using lefetamine, clonidine and buprenorphine. Drug Alcohol Depend 1994;36(2):139-45.
(28.) Batki SL, Selwyn PA. Substance abuse treatment for persons with HIV-AIDS. Rockville, Md.: U.S. Department of Health and Human Services, Public Health Service, Substance Abuse and Mental Health Services Administration, Center for Substance Abuse Treatment, treatment improvement protocol (TIP) series, 2000; DHHS publication no. (SMA) 00-3410:23-68.
(29.) Malliori M, Sypsa V, Psichogiou M, Touloumi G, Skoutelis A, Tassopoulos N, et al. A survey of bloodborne viruses and associated risk behaviours in Greek prisons. Addiction 1998;93:243-51.
(30.) Diamantis I, Bassetti S, Erb P, Ladewig D, Gyr K, Battegay M. High prevalence and coinfection rate of hepatitis G and C infections in intravenous drug addicts. J Hepatol 1997;26(4):794-7.
The Authors
LAURIE LIMPITLAW KRAMBEER, PH.D., is adjunct assistant professor of psychiatry at the University of Kansas Medical Center and program director of the Kansas City Metro Methadone Program, operated by the Center's Department of Psychiatry and Behavioral Sciences in Kansas City, Kan.
WILLIAM VON MCKNELLY, JR., M.D., is professor of psychiatry at the University of Kansas Medical Center and medical director of the Kansas City Metro Methadone Program.
WILLIAM F. GABRIELLI, JR., M.D., PH.D., is professor and chairman of the Department of Psychiatry, University of Kansas Medical Center.
ELIZABETH C. PENICK, PH.D., is professor and director of the Division of Psychology, Department of Psychiatry and Behavioral Sciences, University of Kansas Medical Center.
Address correspondence to Laurie Limpitlaw Krambeer, Ph.D., Department of Psychiatry and Behavioral Sciences, University of Kansas Medical Center, 3901 Rainbow Blvd., Kansas City, KS 66160-7341. Reprints are not available from the authors.
COPYRIGHT 2001 American Academy of Family Physicians
COPYRIGHT 2001 Gale Group