QUESTION. My postoperative patient acknowledges active abuse of opioids. How can I effectively treat his acute pain without reinforcing his addiction?
ANSWER: Never withhold opioids from someone with acute pain who's suffering from addictive disease. No scientific evidence exists to show that providing opioid analgesia to these patients in any way worsens the disease-or that withholding opioid analgesia increases the likelihood of recovery.
To treat your patient's acute postoperative pain, determine the types and amount of opioid drugs to which he's addicted. Although addiction generalizes across substances, try to avoid exposing the patient to the drug he's been abusing.
Always treat severe pain immediately. Start with opioids. In addition, use nonopioid and adjuvant analgesics and nonpharmacologic pain-relief measures when appropriate.
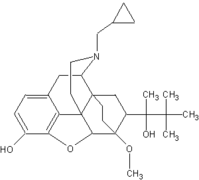
When possible, therapy should involve just one opioid, not several. Avoid a mixed opioid agonistantagonist, such as butorphanol (Stadol) or a partial agonist such as buprenorphine (Buprenex), because these may precipitate withdrawal symptoms.
Provide analgesia around the clock to maintain opioid blood levels and prevent withdrawal symptoms. Use supplemental doses to handle breakthrough pain.
Keep in mind that a patient who's tolerant to opioids will need much higher dosages to manage pain control than an opioid-naive patient would.
With the patient's participation, consider a written agreement or treatment plan. This may reassure him of your commitment to pain relief and encourage him to cooperate with treatment.
Although controversial for treating addicted patients, patientcontrolled analgesia (PCA) may improve pain control and reduce drugseeking behavior, according to limited research. Include guidelines and expectations for appropriate PCA use in the patient's treatment agreement.
As acute pain decreases, plan with the patient to taper the analgesic gradually to prevent withdrawal symptoms, which can exacerbate pain and lead to drug-seeking behavior or illicit drug use. Use oral long-acting opioid formulations to treat the pain and provide stable blood levels.
Monitor the patient at least every 4 hours for withdrawal symptoms such as yawning, tearing, gastrointestinal symptoms, and anxiety/ dysphoric mood. If these symptoms emerge, treat symptoms aggressively with a more gradual taper of the opioid and consider the addition of clonidine to reduce sympathetic hyperactivity.
Assess the patient's motivation for drug addiction treatment, but only after his pain is under control. Have treatment referral references on hand.
Source: Pain: Clinical Manual, 2nd edition, M. McCaffery and C. Pasero, Mosby, Inc., 1999.
BY PEGGY COMPTON, RN, PhD
Assistant Professor - University of California, Los Angeles School of Nursing - Los Angeles, Calif.
MARGO McCAFFERY, RN, MS, FAAN
Consultant in the Nursing Care of Patients with Pain - Los Angeles, Calif.
Copyright Springhouse Corporation Jan 2001
Provided by ProQuest Information and Learning Company. All rights Reserved