INTRODUCTION
Heroin dependence remains a largely untreated medical condition in the United States. Recent research reveals that there are approximately 600,000 heroin dependent individuals who are not receiving drug-abuse treatment services (1). High relapse rates following detoxification (2,3) and restrictions on methadone maintenance (4) have prompted efforts to evaluate alternative pharmacotherapies and settings for maintenance of patients with heroin dependence (1). The Institute of Medicine (4), an NIH consensus panel (1), and the Office on National Drug Control Policy (5) have recommended a restructuring of the regulatory processes involved in the treatment of heroin-dependent patients including increased primary care physician involvement.
Primary care settings represent an attractive site to increase the number of patients receiving treatment for heroin dependence (6-10). Potential advantages of primary care include the large number and geographic dispersal of physicians and sites, increased attention to comorbid medical conditions, decreased stigma associated with treatment in this setting, and decreased contact with other heroin users (7). Prior research has demonstrated successful detoxification and maintenance by clinicians in a primary care clinic designed to provide services to patients with substance-abuse disorders (7,8). In addition, successful maintenance with methadone has been demonstrated in a primary care setting (9,10).
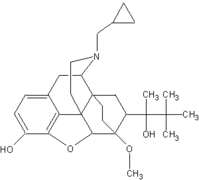
Buprenorphine, currently under review by the Food and Drug Administration (FDA) for maintenance treatment of opioid dependence, has unique pharmacologic properties that suggest its suitability for use outside of traditional narcotic treatment programs, such as primary care (7,11). Buprenorphine is a partial agonist at the muopioid receptor and an antagonist at the kappa-opioid receptor (12,13). Buprenorphine blocks the euphoria of exogenous opioids, prevents opioid withdrawal (13) and has decreased potential for abuse or overdose compared to methadone or other full mu-agonists (14). Buprenorphine has demonstrated efficacy in maintenance therapy, is available alone or in combination with naloxone, and can be dispensed using thrice weekly dosing (7).
Prior research has focused on the efficacy of transferring stabilized patients to office-based settings (9,10,15) or care provided by primary care clinicians aligned with a substance-abuse treatment facility (7). Therefore, the current study was designed to determine the feasibility and potential efficacy of providing buprenorphine maintenance along with psychosocial support to patients in primary care.
METHODS
Patients
Individuals seeking opioid agonist maintenance treatment were recruited for this 13-week trial from those presenting to a drug-treatment program. Inclusion criteria were Diagnostic and Statistical Manual, Fourth Edition (DSM--IV) criteria for opioid dependence (16), opioid-positive urine toxicology, and FDA criteria (17) (e.g., at least 18 years old with 1 year history of opioid addiction and evidence of physiologic dependence) for methadone maintenance. Patients were excluded if they were currently dependent on alcohol, cocaine, benzodiazepines, or sedatives, were a suicide or homicide risk, or had acute medical or psychiatric conditions. Women had to agree to adequate contraception and to monthly pregnancy monitoring throughout the study.
Treatment Setting, Staff Training, and Clinical Supervision
The study was performed in the Primary Care Center of Yale--New Haven Hospital, an urban academically affiliated medical center. Nurses were recruited from the Center's staff and had no prior experience in substance-abuse treatment. Training in Medical Management occurred via a specifically designed manual (18), and included three one-hour sessions on heroin dependence, buprenorphine pharmacology, and counseling. Weekly review of counseling issues with the supervising physician and a doctorate level clinical psychologist was provided.
Buprenorphine Dosing
Buprenorphine was provided in tablet form, which was administered sublingually. Following a one week induction, treatment was administered at 24 mg on Monday and Wednesday and 36 mg on Friday. The dosing protocol allowed for two dose upgrades to 28, 28, and 40 mg for the first upgrade and 32, 32, and 48 mg for the second upgrade. The dose of buprenorphine was increased for continued positive urine toxicology or patient discomfort due to withdrawal. During detoxification, treatment was administered at 16mg on Monday and Wednesday and 24 mg on Friday for the first week and 8 mg on Monday and 4 mg on Wednesday and Friday of the second week.
Psychosocial Support
Patients received Medical Management (MM), which is a manual-guided (18) treatment provided in thrice weekly sessions with a nurse lasting approximately 20 min. Additionally, patients met monthly for approximately 20 min with a general internist physician. All sessions used a brief counseling format that has previously demonstrated efficacy (7). The sessions covered: (1) a review of recent drug use or efforts to maintain abstinence, (2) a review of attendance at self-help groups, (3) support for efforts to reduce drug use or remain abstinent, (4) brief advice on how to achieve or maintain abstinence, and (5) thrice weekly urine sample collection and review. Half of the patients received MM plus manual guided drug counseling (19) provided on-site during weekly 45-minute sessions.
Treatment Assignment
Patients were assigned to the two counseling conditions to form groups balanced by gender and employment status.
Treatment Outcomes
The primary study outcome was illicit opioid use assessed by urine toxicology. Secondary outcomes were self-reported heroin use, urine toxicology for cocaine use, retention and adherence to treatment regimen (e.g., attendance at scheduled visits), overall health status as measured by the Medical Outcomes Study 36-Item Short Form Health Survey (SF-36) (20), and patient satisfaction.
Statistical Analysis
Baseline characteristics and outcomes were compared using the chi-square or Fisher's exact for dichotomous variables and the t-test for continuous variables. Retention rates were evaluated using the Kaplan--Meier product limit method and the generalized Wilcoxon test. Mixed models were used to conduct repeated measures analysis with fixed and random effects on the primary outcome measures. To develop a continuous measure for the urine toxicology results for use in random regression models, urine results were aggregated into an initial induction period and five successive 2-week periods during maintenance (three urine samples per week). The proportion of tests positive during weeks 1 and 2, 3 and 4, 5 and 6, 7 and 8, and 9 and 10 was calculated.
RESULTS
Demographic and Clinical Characteristics
The demographic and clinical characteristics of the 14 patients are shown in Table 1.
Illicit Drug Use
Opioids
Overall, there were significant reductions over time in opioid-positive urine toxicology tests for the 14 patients (p < 0.05) (Fig. 1). The proportion of opioid-positive urine toxicologies declined progressively from induction (95%) through weeks 1 and 2 (56%), 3 and 4 (34%), 5 and 6 (34%), 7 and 8 (29%), and 9 and 10 (25%). Eleven of the 14 patients (79%) achieved at least one week of opioid abstinence as documented by at least three consecutive negative toxicology tests. Nine patients (64%) had greater than or equal to three weeks of opioid abstinence as documented by at least nine consecutive negative toxicology tests. Self-reported heroin use declined from a mean of 6.4 bags at baseline to 0.08 bags per day during week 12 (p < 0.05) and from 7 days at baseline to 0.20 days per week during week 12 (p < 0.05).
[FIGURE 1 OMITTED]
Cocaine
Ten of the 14 patients (71%) had at least one positive urine toxicology for cocaine during the treatment period. There were no significant increases in the proportion of cocaine-positive urine toxicologies during induction (15%), weeks 1 and 2 (13%), 3 and 4 (12%), 5 and 6 (17%), 7 and 8 (21%), 9 and 10 (21%) (p = 0.21). All patients had greater than or equal to one week of cocaine-free urine toxicologies. Ten patients (71%) had greater than or equal to three weeks of cocaine-free urine toxicologies.
Opioids and Cocaine
The proportion of opioid or cocaine-positive urine toxicologies during weeks 1 and 2 (59%), 3 and 4 (39%), 5 and 6 (45%), 7 and 8 (49%), 9 and 10 (38%) (p < 0.05). Nine of the 14 patients (64%) had greater than or equal to one week of opioid- and cocaine-free urine toxicologies. Seven patients (50%) had greater than or equal to three weeks of opioid- and cocaine-free urine toxicologies.
Retention and Adherence to Treatment
Eleven of the 14 patients (79%) completed maintenance. Two patients receiving MM alone discontinued treatment (weeks 2 and 5), while one patient receiving MM plus drug counseling discontinued treatment (week 8). Overall, patients attended 86% of the medication and MM sessions during maintenance. In addition, patients receiving drug counseling attended 90% of these sessions.
Health Status
Health status was assessed at eight weeks in the 12 patients remaining in treatment. Significant improvements were seen compared to baseline, in patients' scores on the physical functioning (88 vs. 81), social functioning (93 vs. 75), mental health index (82 vs. 69) and standardized mental component (55 vs. 47) (p < 0.05 for all comparisons) sub-scales of the SF-36.
Patient Satisfaction
Patient satisfaction was assessed at eight weeks in the 12 patients remaining in treatment. Ten patients reported that they were "very satisfied", one that they were "somewhat satisfied", and one that they were "somewhat dissatisfied" with their treatment. Eleven patients agreed with the statements "The nurses are interested in helping your substance-abuse problem" and "The services in the primary care center have helped you deal more effectively with your drug problem."
Comparing Counseling Interventions
There was a significant decrease in opioid-positive urine toxicology over time for the groups receiving both counseling conditions. Three of the seven patients (43%) who received MM alone compared to six of the seven (86%) who received MM plus supplemental drug counseling had greater than or equal to one week of opioid-free urine toxicologies (p = 0.28). In addition, 62% of urines were free of opioids among those who received MM plus supplemental drug counseling compared to 47% in those who received MM alone (p = 0.30).
DISCUSSION
This is the first study to demonstrate the feasibility of buprenorphine, along with psychosocial counseling, for the treatment of heroin dependence in a general primary care setting. The results demonstrate a 70% absolute reduction in opioid-positive urine toxicology, 79% retention in treatment, and 86% attendance for maintenance medication sessions. In addition, there were measurable benefits in overall health status, and good patient satisfaction with treatment. Finally, there was a trend towards improved abstinence in patients who received formal drug counseling in addition to thrice weekly brief counseling.
The current investigation replicates and extends the findings of O'Connor et al. by performing treatment in a general primary care setting (7,21). Previous trials have reported 71-78% treatment retention (7,19) with 43% of patients achieving three or more consecutive weeks of abstinence (7). The current results compare favorably to maintenance using methadone in which heroin use is reported to occur in up to 29% of patients (3,22-24).
Several limitations to this study should be acknowledged. First, the eligibility criteria limit the generalizability of the findings to patients without psychiatric or substance-use comorbidities. While previous studies have documented the increased rate of psychiatric comorbidities in patients with substance-use disorders (25,26), the recent expansion of heroin use (27,28) indicates that a wide spectrum of patients will require care in primary care and other settings. Second, reductions in heroin use were accompanied by increased use of cocaine in some patients. Third, a physician and clinical psychologist provided ongoing support for nurse counseling and this level of professional involvement may not be practical in some settings. Finally, the treatment period was limited to 13 weeks. Although the effectiveness of this treatment beyond this period is unknown, the findings of persistent reductions in illicit-drug use with time, support investigation of longer periods of buprenorphine maintenance. Given the limited success of detoxification for long-term abstinence (2,3), current recommendations support long-term opioid agonist maintenance for patients with opioid dependence (1).
Buprenorphine is likely to be approved as an alternative pharmacotherapy for treatment of heroin dependence and be available for office-based treatment. The current investigation demonstrates the feasibility of maintenance therapy with this medication, along with psychosocial counseling, in a primary care setting. The observed trend in favor of drug counseling raises questions about the appropriate level of counseling and other psychosocial services needed for buprenorphine maintenance in the primary care setting and warrants further evaluation. Buprenorphine may provide an alternative treatment strategy and aid efforts to extend care to the majority of heroin dependent patients currently without treatment.
ACKNOWLEDGMENTS
Dr. Fiellin is supported by the National Institute on Drug Abuse Physician Scientist Award (NIDA # K12 DA00167).
REFERENCES
(1.) National Consensus Development Panel on Effective Medical Treatment of Opiate Addiction; Effective Medical Treatment of Opiate Addiction. J. Am. Med. Assoc. 1998, 280, 1936-1943.
(2.) O'Connor, P.G.; Kosten, T.R. Rapid and Ultrarapid Opioid Detoxification Techniques. J. Am. Med. Assoc. 1998, 279, 229-234.
(3.) Ball, J.C.; Ross, A. The Effectiveness of Methadone Maintenance Treatment; Springer-Verlag Inc.: New York, NY, 1991.
(4.) Rettig, R.A.; Yarmolinsky, A. Federal Regulation of Methadone Treatment; Institute of Medicine/National Academy Press: Washington, DC, 1995.
(5.) Office of National Drug Control Policy. Policy Paper--Opioid Agonist Treatment. Executive Office of the President, Office of National Drug Control Policy: Washington, DC
(6.) O'Connor, P.G.; Waugh, M.E.; Carroll, K.M.; Rounsaville, B.J.; Diagkogiannis, I.A.; Schottenfeld, R.S. Primary Care-Based Ambulatory Opioid Detoxification: The Results of a Clinical Trial. J. Gen. Intern. Med. 1995, 10, 255-260.
(7.) O'Connor, P.G.; Oliveto, A.H.; Shi, J.M.; Triffleman, E.G.; Carroll, K.M.; Kosten, T.R.; Rounsaville, B.J.; Pakes, J.A.; Schottenfeld, R.S. A Randomized Trial of Buprenorphine Maintenance for Heroin Dependence in a Primary Care Clinic for Substance Users Versus a Methadone Clinic. Am. J. Med. 1998, 105, 100-105.
(8.) O'Connor, P.G.; Carroll, K.M.; Shi, J.M.; Schottenfeld, R.S.; Kosten, T.R.; Rounsaville, B.J. Three Methods of Opioid Detoxification in a Primary Care Setting. A Randomized Trial. Ann. Intern. Med. 1997, 127, 526-530.
(9.) Novick, D.M.; Joseph, H.; Salsitz, E.A.; Kalin, M.F.; Keefe, J.B.; Miller, E.L.; Richman, B.L. Outcomes of Treatment of Socially Rehabilitated Methadone Maintenance Patients in Physicians' Offices (Medical Maintenance): Follow-up at Three and a Half to Nine and a Fourth Years. J. Gen. Intern. Med. 1994, 9, 127-130.
(10.) Novick, D.M.; Pascarelli, E.F.; Joseph, H.; et al., Methadone Maintenance Patients in General Medical Practice. A Preliminary Report. J. Am. Med. Assoc. 1988, 259, 3299-3302.
(11.) Ling, W.; Charuvastra, C.; Collins, J.F.; Batki, S.; Brown, L.S.; Kintaudi, P.; Wesson, D.R.; McNicholas, L.; Tusel, D.J.; Malkerneker, U.; Renner, J.A.; Santos, E.; Casadonte, P.; Pye, C.; Stine, S.; Wang, R.I.H.; Segal, D. Buprenorphine Maintenance Treatment of Opiate Dependence: A Multicenter, Randomized Clinical Trial. Addiction 1998, 93, 475-486.
(12.) Walsh, S.L.; Preston, K.L.; Bigelow, G.E.; Stitzer, M.L. Acute Administration of Buprenorphine in Humans: Partial Agonist and Blockade Effects. J. Pharmacol. Exp. Ther. 1995, 274, 361-372.
(13.) Jasinski, D.R.; Pevnick, J.S.; Griffith, J.D. Human Pharmacology and Abuse Potential of the Analgesic Buprenorphine. A Potential Agent for Treating Narcotic Addiction. Arch. Gen. Psychiatry 1978, 35, 501-516.
(14.) Walsh, S.L.; Preston, K.L.; Stitzer, M.L.; Cone, E.J.; Bigelow, G.E. Clinical Pharmacology of Buprenorphine: Ceiling Effects at High Doses. Clin. Pharmacol. Ther. 1994, 55, 569-580.
(15.) Senay, E.C.; Barthwell, A.G.; Marks, R.; Boros, P.; Gillman, D.; White, G. Medical Maintenance: A Pilot Study. J. Addict. Dis. 1993, 12, 59-76.
(16.) American Psychiatric Association, Diagnostic and Statistical Manual of Mental Disorders, 4th Ed.; American Psychiatric Press: Washington, DC, 1994.
(17.) U.S. Department of Health and Human Services, State Methadone Treatment Guidelines; U.S. Department of Health and Human Services: Rockville, 1993; Vol. 1.
(18.) Fiellin, D. A.; Pantalon, M. V.; Gordon, L.; Schottenfeld, R. S.; O'Connor, P. G. Manual for Standard Medical Management of Opioid Dependence with Buprenorphine. Unpublished manual.
(19.) Mercer, D.; Carpenter, G.; Daley, D.; Petterson, C.; Volpicelli, J. Group Drug Counseling Manual; University of Pennsylvania: Philadelphia, 1992.
(20.) Ware, J.E.; Sherbourne, C.D. The MOS 36-Item Short-Form Health Survey (SF-36). I. Conceptual Framework and Item Selection. Med. Care 1992, 30, 473-481.
(21.) O'Connor, P.G.; Oliveto, A.H.; Shi, J.M.; Triffleman, E.; Carroll, K.M.; Kosten, T.R.; Rounsaville, B.J. A pilot Study of Primary-Care-Based Buprenorphine Maintenance for Heroin Dependence. Am. J. Drug Alcohol Abuse 1996, 22, 523-531.
(22.) D'Aunno, T.D.; Vaughn, T.E. Variations in Methadone Treatment Practices. J. Am. Med. Assoc. 1992, 267, 253-258.
(23.) Hubbard, R.L.; Craddock, S.G.; Flynn, P.M.; Anderson, J.; Etheridge, R.M. Overview of 1-Year Follow-up Outcomes in the Drug Abuse Treatment Outcome Study (DATOS). Psychol. Addict. Behav. 1997, 11, 261-278.
(24.) Yancovitz, S.R.; Des Jarlais, D.C.; Peyser, N.P.; Drew, E.; Friedman, P.; Trigg, H.L.; Robinson, J.W. A Randomized Trial of an Interim Methadone Maintenance Clinic. Am. J. Public Health 1991, 1185-1191.
(25.) Regier, D.A.; Farmer, M.E.; Rae, D.S.; Locke, B.Z.; Keith, S.J.; Judd, L.L.; Goodwin, F.K. Comorbidity of Mental Disorders with Alcohol and Other Drug Abuse. Results from the Epidemiologic Catchment Area (ECA) Study. J. Am. Med. Assoc. 1990, 264, 2511-2518.
(26.) Kessler, R.C.; McGonale, K.Z.; Shanyang, Z.; et al., Lifetime and 12 Month Prevalence of DSM-III-R Psychiatric Disorders in the United States: Results from the National Comorbidity Survey. Arch. Gen. Psychiatry 1994, 51, 8-18.
(27.) SAMHSA, National Household Survey on Drug Abuse: Main Findings 1997; Department of Health and Human Services, Substance Abuse and Mental Health Services Administration: Rockville, MD, 1999.
(28.) SAMHSA, Drug Abuse Warning Network Series: Year-End Preliminary Estimates from the 1996 Drug Abuse Warning Network; Department of Health and Human Services, Substance Abuse and Mental Health Services Administration: Rockville, MD, 1997.
David A. Fiellin, (1), * Michael V. Pantalon, (2) Juliana P. Pakes, (2) Patrick G. O'Connor, (1) Marek Chawarski, (2) and Richard S. Schottenfeld (2)
Departments of (1) Internal Medicine and (2) Psychiatry, Yale University School of Medicine, 333 Cedar St., P.O. Box 208025, New Haven, CT 06520-8025
* Corresponding author. Fax: (203) 688-4092; E-mail: david.fiellin@yale.edu
COPYRIGHT 2002 Marcel Dekker, Inc.
COPYRIGHT 2003 Gale Group