INTRODUCTION
The incidence of abuse of opioid analgesics can be substantial in patients with a present or past history of drug abuse [1]. Thus, physicians are often reluctant to prescribe opioid analgesics ad-libitum to patients with a history of drug abuse. On the other hand, physicians are reluctant to deny analgesia to any patient in true severe pain.
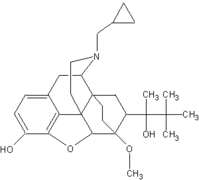
Buprenorphine, a mixed agonist/antagonist, differs from most opioid analgesics in several ways that may favor its use in patients with drug abuse histories. Compared to typical [mu]-agonist opioids, buprenorphine appears to produce less physical dependence [2-5], abuse liability [2,3], and respiratory depression [3]. In addition, buprenorphine blocks the euphoric effects of [mu]-agonist [6] and has a longer duration of analgesia (6-8 h), thus requiring infrequent self-administration [3]. On problem in using buprenorphine is that it can precipitate withdrawal from [mu]-agonist opioids [7]. It appears that buprenorphine can be administered soon after opioid use, but this is still somewhat unclear [8].
In this case study we illustrate the advantage of buprenorphine and report the absence of precipitated withdrawal or loss of analgesia when buprenorphine is given after omission of a single dose of morphine in a patient chronically maintained on morphine.
CASE REPORT
The patient was a 35-year old man with severe Crohn's disease which has required multiple surgeries and total parental nutrition for 7 years. The patient had a past and recent history of abuse of alcohol, sedatives, and opioids.
When we first saw the patient, he was receiving morphine sulfate (MS) 3.6 mg IV q 2 h. We first assessed whether the patient was physically dependent on opioids. If he was not dependent, then he could immediately be switched to buprenorphine. The patient consented to a single-blind naloxone challenge test which is typically used to assess physical dependence [8]. Injections of saline, then 0.2 mg and 0.6 mg naloxone were given IV. With 0.6 mg of naloxone, lacrimation, rhinorrhea, perspiration, piloerection, yawning, and restlessness were observed.
At this point the patient agreed to a single-blind attempt to switch him to buprenorphine. The patient's physician had decreased his morphine to 9 mg IV q 6 h. A 3-day baseline period then occurred in which 9 mg morphine was administered IV at 0300, 0900, 1500, and 2100. Each morning of this period, heart rate, respiratory rate, sitting blood pressure, and temperature were taken and the signs of opioid withdrawal [9] were rated. The patient also completed visual-analogue scales of pain, strength of medication, and good and bad effects, as well as a 20-item opioid withdrawal scale [7]. During this baseline the patient's vital signs and self-ratings were stable, plus observer and self-reported ratings of withdrawal were minimal (Fig. 1).
Next we substituted saline for his 0300 dose of MS. The next morning his vital signs, observer signs of withdrawal, and self-ratings of withdrawal and pain were unchanged. We then began buprenorphine 0.6 mg IV 6 h. Measures at 0.5 h after this first dose showed a possible slight increase in observer and self-rated withdrawal. Repeat measures immediately before and 0.5 h after the next dose of buprenorphine and aily thereafter showed no indication of precipitated withdrawal or increased pain. Analgesia was not interrupted with this protocol.
DISCUSSION
Buprenorphine was used in this patient for two reasons. First, the patient had a history of drug dependence. Buprenorphine appears to produce less physical dependence [1-5] than typical [mu]-agonist opioid analgesics. Second, the patient had a history of impulsive behavior and intoxication. Buprenorphone produces less respiratory depression than typical [mu]-agonist [3]. In the past, certain opioids have been suggested to have less dependence potential and abuse liability tahn [mu]-agonist (e.g., pentazocine). However, these opioids require cessation of [mu]-analgesics for 24-48 h, appear to produce more respiratory depression than buprenorphine, and, unlike buprenorphine, appear to be less acceptable analgesics due to their psychotomimetic effects [8].
Several regimens have been used to transfer daily heroin users into buprenorphine (see Johnston et al. for a review) [8]. The duration between last use of a [mu]-opioid and administration of buprenorphine with these regimens has not been well-specified, but appears to be in the rnage of 12 to 24 h. In the present study we induced 12 h of abstinence by simply omitting the evenign dose of a q 6 h schedule. This protocol allowed us to transfer a patient to buprenorphine without precipitating withdrawal and, importantly, without interrupting analgesia.
References
[1] Portenoy, R. K., and Foley, K. M., Chronic use of opioid analgecis in non-malignant pain: Report of 38 cases, Pain 25:171-186 (1978).
[2] Jasinski, D. R. Pevnick, J. S., and Griffith, J. D., Human pharmacology and abuse potential of the analgesic buprenorphine, Arch. Gen. Psychiatry 35:601-616 (1978).
[3] Lewis, J., Rance, M. J., and Sanger, D. J., The pharmacology and abuse potential of buprenorphine, a new antagonist analgesic, in Advances in Substance Abuse, Behavioral and Biological Research, Vol. 3 (N. K. Mello, ed.), JAI Press, Greenwich, Connecticut, 1982.
[4] Lukas, S. E., Jasinski, D. R., and Johnson, R. E., Electroencephalographic and behavioral correlates of buprenorphine and administration, Clin. Pharmacol. Ther. 36:127-132 (1984).
[5] Mello, N. K., Mendelson, J. H., and Kuehnle, J. C., Buprenorphine's effects on human heroin self-administration, an operant analysis, J. Pharmacol. Exp. Ther. 36:127-132 (1984).
[6] Bickel, W. K., Stitzer, M. L., Bigelow, G. E., Liebson, I. A., Jasinski, D. R., and Johnson, R. E., Buprenorphine: Dose-related blockade of opioid challenge effects in opioid dependent humans, J. Pharmacol. Exp. Tehr. 247:47-53 (1988).
[7] Aceto, M. D., Characterization of prototypical opioid antagonists agonists/antagonist, and agonists in the morphine dependent rhesus monkey, Neuropeptides 5:15-18 (1984).
[8] Johnson, R. E., Cone, E. J., Henningfield, J. E., and Fudals, P. J., Use of buprenorphine in the treatment of opiate addiction. I. Physiologic and behavioral effects during a rapid dose induction, Clin. Pharmacol. Ther. 46:335-343 (1989).
[9] Jaffe, J. H., and Martin, W. R., Opioid analgesics and antagonists, in The Pharmacological Basis of Therapeutics (A. S. Gilman, L. S. Goodman, T. W. Rall, and F. Murad, eds.), Macmillan, New York, 1985.
COPYRIGHT 1991 Taylor & Francis Ltd.
COPYRIGHT 2004 Gale Group