Family physicians frequently care for patients who have migraine and other primary headache disorders. In recent years, the number of headache-related consultations has doubled, and the number continues to increase. (1) Although most headaches are episodic, an estimated 4 to 5 percent of adults have chronic daily headaches (CDH). (2,3) Patients with CDH have a poorer quality of life than patients with episodic migraine headaches. (4) CDH is the cause for most referrals to specialist headache clinics. (5)
Patients with CDH most commonly have a history of episodic migraine that has evolved to a daily headache (chronic migraine). Regardless of the original headache syndrome, overuse of medication occurs in approximately one third of patients who develop daily headaches. Medication-induced headache, or drug rebound headache, has been described as an "unrecognized epidemic." (6) In tertiary headache treatment centers, 50 to 82 percent of patients who have CDH have medication overuse. (7)
Patients with daily headaches are categorized as having primary or secondary headaches. The primary headaches are further divided into those lasting less than or longer than four hours (8,9) (Table 1). (9)
Patient Assessment
In a systematic approach to the patient with CDH, the physician evaluates the patient for potential ominous pathology, determines the primary headache type, and assesses underlying physical contributors to headache, triggering factors, comorbidities, and the patient's medication history (Table 2). (10) The elements of the clinical history, physical examination, and laboratory tests that are suggestive of specific diagnoses causing CDH are summarized in Table 3.
Potentially Significant Pathology
All patients with daily headache require a careful evaluation to exclude secondary causes. Although they may not specifically express it, most patients with CDH are concerned about serious pathology. (11) Potential indicators of intracranial pathology in patients with sudden-onset acute headache are occipitonuchal location, age greater than 40 years, and an abnormal neurologic examination. Symptoms of particular concern in patients with nonacute headache include increasing headache frequency or progressive symptoms, neurologic signs or symptoms (including lack of coordination, subjective numbness and tingling), or headache awakening the patient from sleep (not explained by cluster headache or typical migraine). (12)
In the absence of neurologic findings, episodic migraine does not require imaging studies (12,13); the evidence is less clear for chronic migraine and chronic non-migraine headaches. Based on the low rate of detection of significant pathology, a work group of the American Academy of Neurology (AAN) came to this conclusion: "At this time, there is insufficient evidence to define the role of CT [computed tomography] and MRI [magnetic resonance imaging] in the evaluation of patients with headaches that are not consistent with migraine." (13) A more recent guideline (12) from the AAN recommends that neuroimaging be considered in patients with unexplained abnormal findings on the neurologic examination, but states that there is no clear evidence to recommend MRI or CT as the initial examination.
Table 2 (10) lists significant features that raise the index of suspicion for a pathologic cause in patients with chronic or recurrent headaches. Patients who have had a stable headache pattern for at least six months rarely have significant intracranial pathology. In the absence of worrisome features, these patients do not require imaging. (12) An imaging study for the sake of reassurance is occasionally warranted, but a thorough clinical evaluation usually obviates the need.
Isolated headache without neurologic symptoms is an unusual presentation of brain tumor that occurs in only 8 percent of cases. (14) Although a classic profile of a brain tumor headache has been described (severe headache that is worse in the morning and associated with nausea or vomiting), the pattern is not commonly encountered. (15)
In adults, it is unusual for headache to be the presenting symptom of an underlying systemic disease in the absence of other symptoms. Clinical suspicion should guide testing for anemia, thyroid disease, liver disease, connective tissue disorders, and infectious diseases (i.e., human immunodeficiency virus antibody and Lyme serology) in patients who have risks or features raising the likelihood of these conditions. Diagnostic testing for a systemic cause may have a greater yield in patients with recent onset of daily headache syndromes. Patients often attribute headache to elevated blood pressure, but only sudden or extreme elevations of blood pressure cause headache. (16)
Identifying the Primary Headache
Episodic headaches are usually diagnosed on the basis of the signs and symptoms of the individual headache attack. In patients with CDH, diagnosis is best reached by examining the history of the original headache pattern and its evolution over time.
MIGRAINE
Most patients with CDH who present to physicians with headache have chronic (transformed) migraine. (17) These patients have a history of episodic migraine that has evolved (transformed) over time into a pattern of almost daily headaches. These daily headaches may be mild, but migraine flares may continue to be superimposed on the daily headache symptoms. The most common causes of migraine transformation are frequent headaches at baseline and obesity. (18) Other modifiable risk factors for transformation include medication overuse, snoring, and stressful life events. Risk factors that cannot be modified are female gender, low education/socioeconomic status, and head injury. Sudden transformation may be associated with trauma to the head or neck, medical illness, surgery, or psychologic trauma. (7)
Interestingly, chronic tension-type headaches and other daily headaches (such as post-traumatic headache) may evolve into a pattern of chronic migraine. (19) Chronic migraine may represent a final pathway for several different primary headache types.
TENSION-TYPE HEADACHE
Patients with chronic tension-type headache have daily or near-daily headaches that typically are occipital or diffuse and pressure-like. It is unclear whether psychologic or muscle tension is actually present and, if present, whether these are primary events or epiphenomena. Psychologic and muscle tension also are present with migraine. (20) The role of cervical pathology in chronic tension-type headache continues to be defined. Limited evidence from a single small case series shows that selective blocks of the C1-C2 lateral joint completely relieve headache in two thirds of a highly selected group of patients with occipital headaches. (21)
NEW DAILY PERSISTENT HEADACHE
This type of headache develops "out of the blue" and persists. Patients with new daily persistent headache have no history of headache; if headaches did pre-exist, there is a sudden change to daily headache. A precipitating event is noted in over one half of patients. The most common events are a febrile or viral illness, general surgery, or a stressful life event. (22) These headaches are often refractory to therapy and may persist indefinitely. New daily persistent headache may occur with or without features of migraine.
HEMICRANIA CONTINUA
Although rare, hemicrania continua is an important disorder to consider because it responds consistently to therapy with indomethacin (Indocin). The headache is constant, with exacerbations of pain, strictly unilateral, and often associated with autonomic symptoms of tearing and rhinorrhea.
BRIEF AND UNILATERAL SYNDROMES
Cluster headache is commonly misdiagnosed as migraine, and migraine is occasionally mislabeled as cluster headache. Cluster headache is readily recognized as a daily or near-daily headache, strictly unilateral, of excruciating severity, and associated with tearing, rhinitis, or other facial autonomic symptoms on the side of the headache. The key feature distinguishing this condition from migraine is that cluster headache has a briefer duration, usually 30 minutes to three hours. Other diagnostic clues to cluster headache are clock-like regularity of headache recurrence and reliable triggering by alcohol consumption. Cluster headache is usually episodic, persisting for weeks to months at a time and remitting for months or years between episodes. Approximately 10 percent of cases, however, are reported to be chronic, with continuous daily episodes. Clinical features and therapies for cluster headache have recently been reviewed. (23)
Other brief headache syndromes are uncommon but merit recognition. Brief headache syndromes that are strictly unilateral usually are associated with autonomic features such as tearing and rhinitis. Other than cluster headache, these headaches are consistently responsive to indomethacin therapy, to the extent that a positive response to this agent is a diagnostic feature.
Drug Rebound and Medication Overuse
Patients who do not stop analgesic overuse fail to improve despite use of preventive therapy. (24,25) Conversely, patients who stop taking analgesics on a daily basis have a marked reduction in frequency of headache. Drug rebound headache is a common treatable cause of transformed migraine, and some experts believe it is important in other daily headache syndromes, including post-concussive headache. (26) Patients who have drug rebound headache are typically refractory to usual acute and prophylactic interventions. The patient who repeatedly presents to the emergency department requesting narcotics for headache relief most commonly has drug rebound headache. (27)
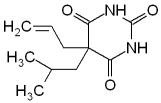
There is no established threshold for the quantity, frequency, or duration of medication use required for the development of drug rebound headache. Affected patients typically take headache-relieving medication daily or near daily, but the sustained use of these medications more than three days per week is probably sufficient to develop drug rebound headache. All symptomatic headache medications, including triptans, (28) have the potential to cause drug rebound headache. The agents most commonly reported to cause drug rebound headache are narcotics, butalbital products, and combination products containing caffeine. (25)
Physicians should remain alert to signs of secondary headache in patients who are self-medicating frequently. Only after a careful evaluation for secondary headache should drug rebound headache be suspected in patients with medication overuse.
Headache History
An initial, open-ended question, such as "Tell me about your headaches," will yield valuable information that may not be acquired by a relentless pursuit using closed-ended questions. Patients may report having several different types of headache and give each one a label, such as "migraine," "tension headache," or "sinus headache." The patient should be allowed to describe each of these headache types, even though they may all represent different manifestations of the spectrum of a migraine headache. (29)
Particular attention should be given to the patient's age at onset, the circumstances of headache onset, the time when headaches worsened or began occurring daily, and associated life events. Medical or surgical illnesses, trauma involving the head or neck, and life stressors commonly are identified with the onset of headaches or the transformation of headaches from episodic and/or manageable to CDH.
Physical Examination
The neurologic examination is crucial to exclude even subtle signs of cerebral dysfunction. The patient's ability to communicate the history is a valuable measure of mental status. The funduscopic examination must be documented. Subtle signs of frontal lobe dysfunction may be demonstrated by testing stereognosis (such as the ability to identify an object placed in the patient's palm). A thorough examination also will reassure the patient and may obviate the need for imaging studies when there are no historical features of concern.
A myofascial evaluation should include cervical range-of-motion, trigger points of the upper back, and temporomandibular motion and tenderness. However, positive physical findings are common and do not necessarily indicate the cause of the headache. Seventy-five percent of patients with migraine complain of associated neck pain; triptan therapy resolves both neck pain and headache. (30)
The question of sinus abnormalities as a cause of headache remains controversial (31,32) Nearly 90 percent of patients with frequent episodes of "sinus" headache fulfill criteria for migraine headache. (33) CT imaging or nasal endoscopy may occasionally identify a treatable cause of headache in a patient with sinus symptoms.
Assessing Psychiatric Comorbidity
Anxiety and depression are highly prevalent in patients who have CDH (7) and, when present, may negatively influence prognosis. All patients who have CDH should be screened for psychiatric comorbidity. Direct questioning (such as, "Are you depressed?"), indirect questioning, and screening instruments (such as the Beck Depression Inventory) may be used. The Primary Care Evaluation of Mental Disorders (PRIME-MD), a multidimensional psychiatric screening tool that also identifies other somatic complaints, (34) may be particularly useful for screening patients with headache.
Treatment
The appropriate treatment of patients with CDH emphasizes the reduction of headache triggers and the use of preventive therapy (Tables 4 and 5), The goals of migraine preventive therapy are to (1) reduce attack frequency, severity, and duration; (2) improve responsiveness to treatment of acute attacks; and (3) improve function and reduce disability. (13) Many tricyclic antidepressants and certain anticonvulsants appear to be effective treatments, with amitriptyline (Elavil) having the best documented efficacy. (35,36) Beta blockers are commonly used if there is a migraine component. Patients with refractory headaches often require therapy with several agents such as a tricyclic antidepressant plus an anticonvulsant and a beta blocker. Selective serotonin reuptake inhibitors appear to be most useful in patients with psychiatric comorbidity.
If the patient is overusing medications, the overuse must be managed before prophylactic agents will be effective (Table 6). The treatment of drug rebound headache involves (1) withdrawal from all symptomatic agents, including caffeine; (2) a transition therapy to support the patient during detoxification; and (3) initiation or adjustment of headache prophylaxis. The literature is insufficient to recommend any one treatment over another (37) Patients often have exacerbation of headache in the first two weeks following withdrawal from analgesics and may require four to 12 weeks after withdrawal (occasionally, even longer) to show improvement.
Once the patient has completed an adequate period of medication withdrawal, the use of symptomatic medications again may be allowed, but on a limited basis--no more than two days per week. Nonsteroidal anti-inflammatory drugs and triptans are most commonly used in patients with occasional migraine flares. The use of medications that are highly prone to drug rebound, such as narcotics and combination products containing butalbital or caffeine, should be avoided. Dihydroergotamine (DHE)ay be used safely over an extended period.
The primary care physician can provide behavioral support by helping the patient identify lifestyle triggers and psychosocial stressors. Behaviors that help to prevent headache flares include establishing a habit of regular meal times, sleep and awake times, and exercise. It is useful to help the patient to identify any connection between psychosocial stressors and headache flares. Most headache patients can benefit from basic stress-reduction techniques such as yoga and meditation. There is compelling evidence for the efficacy of biofeedback, relaxation techniques, and cognitive-behavior therapy for headache prophylaxis. (38) Referral to a medical psychologist or a pain psychologist should be considered for patients with significant psychosocial stressors or refractory headache.
Referral
Patients who do not respond to appropriate prophylaxis or who frequently use narcotics or butalbital products should be referred to a headache specialist. Patients with significant psychiatric comorbidity, associated chronic pain, and/or chemical dependency may require the services of a multidisciplinary pain clinic. Tertiary headache centers that provide inpatient care should be considered for patients who have not responded to aggressive outpatient therapy.
The author thanks Anne Walling, M.D., for suggesting the topic for this manuscript.
REFERENCES
(1.) Gibbs TS, Fleischer AB Jr, Feldman SR, Sam MC, O'Donovan CA. Health care utilization in patients with migraine: demographics and patterns of care in the ambulatory setting. Headache 2003;43:330-5.
(2.) Scher AI, Stewart WF, Liberman J, Lipton RB. Prevalence of frequent headache in a population sample. Headache 1998;38:497-506.
(3.) Castillo J, Munoz P, Guitera V, Pascual J. Epidemiology of chronic daily headache in the general population. Headache 1999;39:190-6.
(4.) Monzon MJ, Lainez MJ. Quality of life in migraine and chronic daily headache patients. Cephalalgia 1998;18:638-43.
(5.) Mathew NT, Reuveni U, Perez F. Transformed or evolutive migraine. Headache 1987;27:102-6.
(6.) Edmeads J. Analgesic-induced headaches: an unrecognized epidemic. Headache 1990;30:614-5.
(7.) Mathew NT. Transformed migraine, analgesic rebound, and other chronic daily headaches. Neurol Clin 1997;15:167-86.
(8.) Silberstein SD, Lipton RB, Solomon S, Mathew NT. Classification of daily and near-daily headaches: proposed revisions to the IHS criteria. Headache 1994;34:1-7.
(9.) Chronic daily headache: diagnosis and treatment. In: Silberstein SD, Lipton RB, Goadsby PJ. Headache in clinical practice. 2d ed. London: Martin Dunitz, 2002.
(10.) Dodick DW. Clinical clues and clinical rules: primary vs secondary headache. Adv Stud Med 2003;3:S550-S5.
(11.) Walling AD. Headache. Home Study Self-Assessment Monograph No. 265. Leawood, Kan.: American Academy of Family Physicians, 2001.
(12.) Silberstein SD. Practice parameter: evidence-based guidelines for migraine headache (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2000;55:754-62.
(13.) Frishberg BM. The utility of neuroimaging in the evaluation of headache in patients with normal neurologic examinations. Neurology 1994;44:1191-7.
(14.) Vasquez-Barquero A, Ibanez FJ, Herrera S, Izquierdo JM, Berciano J, Pascual J. Isolated headache as the presenting clinical manifestation of intracranial tumors: a prospective study. Cephalalgia 1994;14:270-2.
(15.) Forsyth PA, Posner JB. Headaches in patients with brain tumors: a study of 111 patients. Neurology 1993;43:1678-83.
(16.) Strandgaard S, Henry P. Arterial hypertension. In: Olesen J, Tfelt-Hansen P, Welch KM. The headaches. Philadelphia: Lippincott Williams & Wilkins, 2000:819-22.
(17.) Headache Classification Subcommittee of the International Headache Society. The international classification of headache disorders. 2d ed. Cephalalgia 2004;24(suppl 1):9-160.
(18.) Scher AI, Stewart WF, Ricci JA, Lipton RB. Factors associated with the onset and remission of chronic daily headache in a population-based study. Pain 2003;106:81-9.
(19.) Spierings EL, Schroevers M, Honkoop PC, Sorbi M. Presentation of chronic daily headache: a clinical study. Headache 1998;38:191-6.
(20.) Solomon S. Diagnosis of primary headache disorders. Validity of the International Headache Society criteria in clinical practice. Neurol Clin 1997;15:15-26.
(21.) Aprill C, Axinn M J, Bogduk N. Occipital headaches stemming from the lateral atlanto-axial (C1-2)joint. Cephalalgia 2002;22:15-22.
(22.) Li D, Rozen TD. The clinical characteristics of new daily persistent headache. Cephalalgia 2002;22:66-9.
(23.) Bahra A, May A, Goadsby PJ. Cluster headache: a prospective clinical study with diagnostic implications. Neurology 2002;58:354-61.
(24.) Kudrow L. Paradoxical effects of frequent analgesic use. Adv Neurol 1982;33:335-41.
(25.) Mathew NT, Kurman R, Perez F. Drug induced refractory headache-clinical features and management. Headache 1990;30:634-8.
(26.) Warner JS. The outcome of treating patients with suspected rebound headache. Headache 2001;41:685-92.
(27.) Maizels M. Health resource utilization of the emergency department headache "repeater." Headache 2002;42:747-53.
(28.) Limmroth V, Katsarava Z, Fritsche G, Przywara S, Diener HC. Features of medication overuse headache following overuse of different acute headache drugs. Neurology 2002;59:1011-4.
(29.) Cady R, Schreiber C, Farmer K, Sheftell F. Primary headaches: a convergence hypothesis. Headache 2002;42:204-16.
(30.) Kaniecki RG. Migraine and tension-type headache: an assessment of challenges in diagnosis. Neurology 2002;58(suppl 6):S15-20.
(31.) Blumenthal HJ. Headaches and sinus disease. Headache 2001;41:883-8.
(32.) Cady RK, Schreiber CP. Sinus headache or migraine? Considerations in making a differential diagnosis. Neurology 2002;58(9 suppl 6):S10-4.
(33.) Schreiber CP, Hutchinson S, Webster CJ, Ames M, Richardson MS, Powers C. Prevalence of migraine in patients with a history of self-reported or physician-diagnosed "sinus" headache. Arch Intern Med 2004;164:1769-72.
(34.) Spitzer RL, Williams JB, Kroenke K, Linzer M, deGruy FV 3d, Hahn SR, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1000 study. JAMA 1994;272:1749-56.
(35.) Holroyd KA, O'Donnell FJ, Stensland M, Lipchik GL, Cordingley GE, Carlson BW. Management of chronic tension-type headache with tricyclic antidepressant medication, stress management therapy, and their combination: a randomized controlled trial. JAMA 2001;285:2208-15.
(36.) Redillas C, Solomon S. Prophylactic phamacological treatment of chronic daily headache. Headache 2000;40:83-102.
(37.) Zed PJ, Loewen PS, Robinson G. Medication-induced headache: overview and systematic review of therapeutic approaches. Ann Pharmacother 1999;33:61-72.
(38.) Penzien DB, Rains JC, Andrasik F. Behavioral management of recurrent headache: three decades of experience and empiricism. Appl Psychophysiol Biofeedback 2002;27:163-81.
MORRIS MAIZELS, M.D., Kaiser Permanente, Woodland Hills, California
MORRIS MAIZELS, M.D., is a member of the Department of Family Practice at Kaiser Permanente, Woodland Hills, Calif. In addition, he is founder and director of the Woodland Hills Headache Clinic for Kaiser Permanente. Dr. Maizels received his medical degree from the University of Washington School of Medicine, Seattle. He is a member of the Board of Directors of the American Headache Society and an associate editor of Headache: The Journal of Head and Face Pain.
Address correspondence to Morris Maizels, M.D., Department of Family Practice, Woodland Hills Headache Clinic, Kaiser Permanente, Woodland Hills, CA 91365 (e-mail: Morris. Maizels@kp.org). Reprints are not available from the author.
The author indicates that he does not have any conflicts of interest. Sources of funding: Dr. Maizels has been a speaker for Merck & Co., Inc.; Pfizer Inc.; and Novartis Inc.; and is or has been a consultant for Merck & Co., Inc.; GlaxoSmithKline, Inc.; Pharmacia; and Ortho-McNeil, Inc. In addition, he has received research grants from Merck & Co, Inc.; Novartis Inc.; and the Natural Science Corporation of America. He solicits funding from all major pharmaceutical companies to support continuing medical eduction-approved migraine symposia.
COPYRIGHT 2004 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group