TEST YOUR KNOWLEDGE OF GLANDULAR PROBLEMS AND APPROPRIATE NURSING INTERVENTIONS.
1. All of the following are appropriate for a patient with nephrogenic diabetes insipidus (DI) except
a. thiazide diuretics.
b. a low-sodium diet.
c. a low-protein diet.
d. desmopressin.
Rationale: d. Desmopressin is used to treat patients with central DI. For patients with nephrogenic DI, treatment typically includes a lowsodium, low-protein diet and thiazide diuretics to IN induce volume depletion and improve sodium, chloride and water reabsorption in the proximal tubules. This resuits in less volume delivered to the collecting ducts, which are lacking in antidiuretic hormone (ADH).
2. A diabetic patient should be closely monitored for the Somogyi effect. Which of the following statements is incorrect?
a. The Somogyi effect is associated with undetected episodes of hypoglycemia during sleep.
b. The Somogyi effect causes low early-morning blood glucose levels and high postprandial blood glucose levels.
c. The Somogyi effect can be treated by increasing the insulin dosage.
d. The Somogyi effect can be treated by decreasing the insulin dosage.
Rationale: c. Increasing the insulin dosage would women the Somogyi effect, which is associated with undetected episodes of hypoglycemia during sleep. A low early-morning blood glucose level and a high postprandial blood glucose level result from excess insulin and rebound hyperglycemia. The treatment of choice to counteract the Somogyi effect is to reduce the insulin dosage.
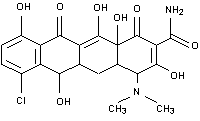
3. The physician prescribes demeclocycline for a patient with syndrome of inappropriate antidiuretic hormone (SL4,DH). This drug is given to
a. prevent seizure activity associated with hyponatremia.
b. inhibit the release of ADH.
c. prevent supraventricular arrhythmias.
d. interfere with the action of ADH at the renal tubules.
Rationale: d. Demeclocycline, a tetracycline, causes nephrogenic DI by interfering with the action of ADH at the renal tubules, allowing diuresis to occur. The drug has no effect on seizure activity or myocardial conduction, nor does it inhibit the release of ADH.
4. During fluid resuscitation and electrolyte replacement for a patient with diabetic ketoacidosis (DKA), the serum potassium level is a primary concern. Which of the following statements about potassium is incorrect?
a. Potassium returns to the intracellular compartment via glucose.
b. Potassium moves into the extracellular space in metabolic acidosis.
c. Potassium loss in the renal tubules results from hyperglycemia, which promotes osmotic diuresis.
d. Potassium-phosphorus supplements can be used to restore potassium and phosphate losses.
Rationale: a. In a patient with DKA., the serum potassium level initially is elevated because of dehydration and metabolic acidosis. However, once fluids and insulin are administered, potassium begins moving into the intracellular compartments. This shifting is directly related to the administration of insulin, not glucose. The diuresis associated with hyperglycemia causes a profound loss of electrolytes, so carefully assess for signs of hypokalemia as the glucose level is corrected. Although phosphorus replacement is controversial, simultaneous replacement of phosphorus and potassium can be accomplished with potassium-phosphorus supplements.
5. Your patient, a 64-year-old woman with DI resulting from a pituitary tumor, is lethargic and weak. On admission, she was hypernatremic, with a serum sodium level of 152 mEq/liter. Her vital signs are: temperature, 101.6 F (38.7 deg.C); pulse, 124 beats/minute with sinus tachycardia; respirations, 22; and BP, 102/68. Given the patient's mental status, the physician orders intravenous (LV ) fluids to correct the water deficit. Which statement about volume replacement in a patient with DI is true?
a. The water deficit should be corrected quickly to prevent intravascular collapse and shock.
b. The water deficit should be corrected gradually over 48 hours to prevent cerebral edema, seizures, and death.
c. The water deficit should be corrected using a hypertonic saline solution to increase tubular water resorption.
d. The water deficit should be replaced over 24 hours to support normal cardiac output.
Rationale: b. If water is replaced too quickly, fluid can shift from the intravascular space into the brain cells, resulting in cerebral edema, seizures, and possibly death. The type of fluid used to correct a deficit depends on the patient's condition; however, oral or LV DSW is a common option. An isotonic saline solution may be used initially to stabilize the patient's hemodynamic status. 6. In the case study above, the patient's DI results from a lack of which hormone?
a. ADH
b. corticotropin
c. glucocorticoid hormones
d. gonadotropin hormones
Rationale: a. DI related to a pituitary dysfunction, such as a pituitary tumor, is caused by a deficiency of ADH. A lack of ADH in central DI also can be caused by head trauma, neurosurgery, cerebrat injury, or infection. The other hormones listed aren't associated with DI.
7. All of the following are signs and symptoms of hyperosmolar nonketotic syndrome (FINKS) except
a. intracellular dehydration.
b. osmotic diuresis.
c. hyperglycemia.
d. fatty acid release.
Rationale: d. For reasons not clearly understood, fatty acid release doesn't occur in HNKS. Patients with this condition probably have enough insulin to avoid lipolysis but not enough to prevent hyperglycemia. Intracellular dehydration and osmotic diuresis are other signs of HNKS.
8. All of the following stimulate the posterior pituitary gland to release ADH except
a. hypercapnia via chemoreceptor stimulation.
b. hypovolemia via pressurereceptor stimulation.
c. hypotension via baroceptor stimulation.
d. hypothalamic osmoreceptor stimulation.
Rationale: a. Hypercapnia doesn't trigger the release of ADH. Antidiuretic hormone is released in response to plasma osmolarity. Hypovolemia and hypotension also stimulate the release of ADH, which results in antidiuresis.
9. Which fluid and electrolyte changes are common in a patient with SIADH?
a. decreased serum sodium, decreased plasma osmolarity, and increased urine sodium
b. decreased urine volume, increased serum sodium, and increased urine sodium
c. increased weight, increased serum sodium, and increased plasma osmolarity
d. decreased weight, decreased serum sodium, and decreased plasma osmolarity
Rationale: a. Diagnostic test results in a patient with SIADH would include a decreased serum sodium level, decreased plasma osmolarity, increased urine osmolarity, and increased urine sodium level. Weight gain also occurs.
Source: Springhouse Certification Review: Critical Care Nursing, Springhouse Corp., 1997.
Copyright Springhouse Corporation Aug 2000
Provided by ProQuest Information and Learning Company. All rights Reserved