Definition
Antibiotics may be informally defined as the subgroup of anti-infectives that are derived from bacterial sources and are used to treat bacterial infections. Other classes of drugs, most notably the sulfonamides, may be effective antibacterials. Similarly, some antibiotics may have secondary uses, such as the use of demeclocycline (Declomycin, a tetracycline derivative) to treat the syndrome of inappropriate antidiuretic hormone (SIADH) secretion. Other antibiotics may be useful in treating protozoal infections.
Purpose
Antibiotics are used for treatment or prevention of bacterial infection.
Description
Although there are several classification schemes for antibiotics, based on bacterial spectrum (broad versus narrow) or route of administration (injectable versus oral versus topical), or type of activity (bactericidal vs. bacteriostatic), the most useful is based on chemical structure. Antibiotics within a structural class will generally show similar patterns of effectiveness, toxicity, and allergic potential.
Penicillins
The penicillins are the oldest class of antibiotics, and have a common chemical structure which they share with the cephalopsorins. The two groups are classed as the beta-lactam antibiotics, and are generally bacteriocidal-that is, they kill bacteria rather than inhibiting growth. The penicillins can be further subdivided. The natural pencillins are based on the original penicillin G structure; penicillinase-resistant penicillins, notably methicillin and oxacillin, are active even in the presence of the bacterial enzyme that inactivates most natural penicillins. Aminopenicillins such as ampicillin and amoxicillin have an extended spectrum of action compared with the natural penicillins; extended spectrum penicillins are effective against a wider range of bacteria. These generally include coverage for Pseudomonas aeruginosa and may provide the penicillin in combination with a penicillinase inhibitor.
Cephalosporins
Cephalosporins and the closely related cephamycins and carbapenems, like the pencillins, contain a beta-lactam chemical structure. Consequently, there are patterns of cross-resistance and cross-allergenicity among the drugs in these classes. The "cepha" drugs are among the most diverse classes of antibiotics, and are themselves subgrouped into 1st, 2nd and 3rd generations. Each generation has a broader spectrum of activity than the one before. In addition, cefoxitin, a cephamycin, is highly active against anaerobic bacteria, which offers utility in treatment of abdominal infections. The 3rd generation drugs, cefotaxime, ceftizoxime, ceftriaxone and others, cross the blood-brain barrier and may be used to treat meningitis and encephalitis. Cephalopsorins are the usually preferred agents for surgical prophylaxis.
Fluroquinolones
The fluroquinolones are synthetic antibacterial agents, and not derived from bacteria. They are included here because they can be readily interchanged with traditional antibiotics. An earlier, related class of antibacterial agents, the quinolones, were not well absorbed, and could be used only to treat urinary tract infections. The fluroquinolones, which are based on the older group, are broad-spectrum bacteriocidal drugs that are chemically unrelated to the penicillins or the cephaloprosins. They are well distributed into bone tissue, and so well absorbed that in general they are as effective by the oral route as by intravenous infusion.
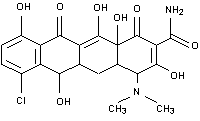
Tetracyclines
Tetracyclines got their name because they share a chemical structure which has four rings. They are derived from a species of Streptomyces bacteria. Broad-spectrum bacteriostatic agents, the tetracyclines may be effective against a wide variety of microorganisms, including rickettsia and amebic parasites.
Macrolides
The macrolide antibiotics are derived from Streptomyces bacteria, and got their name because they all have a macrocyclic lactone chemical structure. Erythromycin, the prototype of this class, has a spectrum and use similar to penicillin. Newer members of the group, azithromycin and clarithyromycin, are particularly useful for their high level of lung penetration. Clarithromycin has been widely used to treat Helicobacter pylori infections, the cause of stomach ulcers.
Others
Other classes of antibiotics include the aminoglycosides, which are particularly useful for their effectiveness in treating Pseudomonas aeruginosa infections; the lincosamindes, clindamycin and lincomycin, which are highly active against anaerobic pathogens. There are other, individual drugs which may have utility in specific infections.
Recommended dosage
Dosage varies with drug, route of administration, pathogen, site of infection, and severity. Additional considerations include renal function, age of patient, and other factors. Consult manufacturers' recommendations for dose and route.
Side effects
All antibiotics cause risk of overgrowth by non-susceptible bacteria. Manufacturers list other major hazards by class; however, the health care provider should review each drug individually to assess the degree of risk. Generally, breastfeeding is not recommended while taking antibiotics because of risk of alteration to infant's intestinal flora, and risk of masking infection in the infant. Excessive or inappropriate use may promote growth of resistant pathogens.
Penicillins. Hypersensitivity may be common, and cross allergenicity with cephalosporins has been reported. Penicillins are classed as category B during pregnancy.
Cephalopsorins. Several cephalopsorins and related compounds have been associated with seizures. Cefmetazole, cefoperazone, cefotetan and ceftriaxone may be associated with a fall in prothrombin activity and coagulation abnormalities. Pseudomembranous colitis has been reported with cephalosporins and other broad spectrum antibiotics. Some drugs in this class may cause renal toxicity. Pregnancy category B.
Fluroquinolones. Lomefloxacin has been associated with increased photosensitivity. All drugs in this class have been associated with convulsions. Pregnancy category C.
Tetracyclines. Demeclocycline may cause increased photosensitivity. Minocycline may cause dizziness. Do not use tetracyclines in children under the age of eight, and specifically avoid during periods of tooth development. Oral tetracyclines bind to anions such as calcium and iron. Although doxycycline and minocycline may be taken with meals, patients must be advised to take other tetracycline antibiotics on an empty stomach, and not to take the drugs with milk or other calcium-rich foods. Expired tetracycline should never be administered. Pregnancy category D. Use during pregnancy may cause alterations in bone development.
Macrolides: Erythromycin may aggravate the weakness of patients with myasthenia gravis. Azithromycin has, rarely, been associated with allergic reactions, including angioedema, anaphylaxis, and dermatologic reactions, including Stevens-Johnson syndrome and toxic epidermal necrolysis. Oral erythromycin may be highly irritating to the stomach and when given by injection may cause severe phlebitis. These drugs should be used with caution in patients with liver dysfunction. Pregnancy category B: Azithromycin, erythromycin. Pregnancy category C: Clarithromycin, dirithromycin, troleandomycin.
Aminoglycosides: This class of drugs causes kidney and ototoxicity. These problems can occur even with normal doses. Dosing should be based on renal function, with periodic testing of both kidney function and hearing. Pregnancy category D.
Interactions
Consult specialized references.
Recommended usage
To minimize risk of adverse reactions and development of resistant strains of bacteria, antibiotics should be restricted to use in cases where there is either known or a reasonable presumption of bacterial infection. The use of antibiotics in viral infections is to be avoided. Avoid use of fluroquinolones for trivial infections.
In severe infections, presumptive therapy with a broad-spectrum antibiotic such as a third generation cephalosporin may be appropriate. Treatment should be changed to a narrow spectrum agent as soon as the pathogen has been identified. After 48 hours of treatment, if there is clinical improvement, an oral antibiotic should be considered.
When the pathogen is known or suspected to be Pseudomonas, use a suitable beta-lactam drug in combination with an aminoglycoside. Do not rely on a single agent for treatment of Pseudomonas. When the patient has renal insufficiency, consider azactam in place of the aminoglycoside.
In treatment of children with antibiotic suspensions, caregivers should be instructed in use of oral syringes or measuring teaspoons. Household teaspoons are not standardized and will give unreliable doses.
Key Terms
- Bacteria
- Tiny, one-celled forms of life that cause many diseases and infections.
- Inflammation
- Pain, redness, swelling, and heat that usually develop in response to injury or illness.
- Meningitis
- Inflammation of tissues that surround the brain and spinal cord.
- Microorganism
- An organism that is too small to be seen with the naked eye.
- Organism
- A single, independent unit of life, such as a bacterium, a plant or an animal.
- Pregnancy category
- A system of classifying drugs according to their established risks for use during pregnancy. Category A: Controlled human studies have demonstrated no fetal risk. Category B: Animal studies indicate no fetal risk, but no human studies; or adverse effects in animals, but not in well-controlled human studies. Category C: No adequate human or animal studies; or adverse fetal effects in animal studies, but no available human data. Category D: Evidence of fetal risk, but benefits outweigh risks. Category X: Evidence of fetal risk. Risks outweigh any benefits.