More than 150 years ago William Morton successfully used diethyl ether as general anaesthesia. Advances in anaesthesia have made many new surgical techniques possible, and mortality directly attributable to anaesthesia is now rare. Most recent advances have contributed to an important decrease in morbidity from anaesthesia and to an increase in quality of perioperative management.
Methods
Although anaesthesia encompasses intensive care medicine and chronic pain management, our review is limited to advances in anaesthesia for surgery and obstetrics. We discuss topics that we believe, after canvassing our colleagues, to be the most topical in recent international literature on anaesthesia. Although some of the developments have a long history, they are all recent additions to clinical practice.
Inhalational anaesthesia
Volatile anaesthetics remain the commonest agents for maintenance of anaesthesia but since the introduction of sodium thiopentone, intravenous agents have been used for induction. Induction with volatile agents is often slow, stormy, and unpleasant for the patient Volatile agents that possessed acceptable induction characteristics lost favour because of their side effects, but the new agent sevoflurane has, to a great extent, improved their popularity.[1]
Sevoflurane
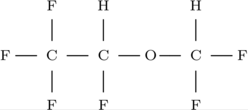
Although first synthesised in the late 1960s, sevoflurane has only recently been available for general use. Sevoflurane is a methylpropyl ether which, because of its high insolubility--it is more than three times less soluble in blood than halothane--produces both rapid induction and recovery characteristics and easy control of anaesthetic depth.[2] Sevoflurane's low solubility enables a faster onset of anaesthesia because the partial pressure of the gas in the brain increases more rapidly than it does with the older agents. Similarly, when administration of sevoflurane ceases, the fall in partial pressure of the gas in the brain is equally rapid, and therefore recovery from anaesthesia is also faster than with the older agents. Importantly, sevoflurane does not irritate the airways and is therefore associated with a rapid and pleasant induction. Induction with sevoflurane is becoming extremely popular, especially in children, but maintenance with sevoflurane is less popular owing to its expense and a potentially nephrotoxic metabolite, compound A, which may accumulate during closed circuit anaesthesia with low gas flows. Considerable debate about the significance of sevoflurane in maintenance is ongoing, but its use in low flow circuits has been restricted in the United States.[3]
Desflurane
Desflurane was also developed in the 1960s and has been only recently introduced into clinical practice.[4] Although desflurane has similar physical properties to sevoflurane it is irritant to the airway and, when used in children, 50% may develop signs of laryngospasm.[5] When used for maintenance, however, desflurane allows precise control of depth of anaesthesia[6] and very rapid recovery.[7] As desflurane can be used safely at low gas flows, thus allowing costs to be kept down,[8] these characteristics can be exploited.
Xenon
Xenon is an inert gas with anaesthetic properties but until recently its cost has been prohibitive. It is extremely insoluble in plasma and thus exhibits an even faster onset of action and recovery than any volatile agent.[9] It is not sufficiently potent to be used alone in most patients, however, but may replace nitrous oxide as a supplement to general anaesthesia in the future; it has analgesic properties, is less soluble, and is not a greenhouse gas (unlike nitrous oxide).[10]
Intravenous anaesthesia
Total intravenous anaesthesia
Propofol
Since the introduction of propofol in 1984 no new intravenous anaesthetic agents have been introduced. Significant advances have been made, however, in the methods of administration of propofol for induction and maintenance of anaesthesia without the use of volatile agents, termed total intravenous anaesthesia. Exponents of this technique claim excellent recovery characteristics and a low incidence of postoperative nausea and vomiting, with the avoidance of potentially harmful pollution of the surgical environment.[11] A major disadvantage of propofol has been the difficulty of achieving the desired plasma concentration by manual control of the infusion rate since to maintain this concentration accurately the infusion rate must be adjusted frequently. In practice the resulting plasma concentration can vary erratically causing haemodynamic instability or light anaesthesia.
Target controlled infusion
Target controlled infusion systems allow the anaesthetist to set a desired plasma concentration, which the software inside the pump produces rapidly but safely by controlling the infusion rate according to complex but standard pharmacokinetic equations.[12 13] Changes may still be required according to clinical signs, but the technique enables changes in rate to reflect factors such as patient characteristics, previous administration of propofol, and duration of infusion (fig 1).
[Fig 1 ILLUSTRATION OMITTED]
If a reliable monitor of anaesthetic depth becomes available it will be possible to "dose the loop" and provide virtually automatic anaesthesia by feedback control of a target controlled infusion system. Much research has focused on this, with the aim of producing a machine that will reliably indicate whether a paralysed patient is anaesthetised. Unfortunately, autonomic clinical signs do not always detect an aware patient especially in the presence of drugs that affect these signs, such as [Beta] blockers. Recent work has concentrated on measurements derived from an electroencephalogram, but most of these are unreliable or too complex for practical use. The auditory evoked potential index--a single numerical variable derived from the auditory evoked potential--was found to show consistent changes that may reliably detect awareness.[15 16] Prototype closed loop systems, using the auditory evoked potential index to control propofol given by target controlled infusion, have been described.[17]
Remifentanil
Remifentanil is a new potent synthetic opioid ideally suited for infusion (often with a target controlled infusion system) during anaesthesia. Unlike other opioids, remifentanil contains a methyl ester in its structure, which allows rapid extrahepatic non-saturable metabolism by non-specific esterases in blood and tissues.[18] Most significantly, the terminal half life of remifentanil is less than 10 minutes and, unlike all other opioids, this is not affected by duration of infusion (fig 2).[19] Remifentanil's place in anaesthesia has yet to be fully determined. Critics point out the lack of postoperative analgesia with remifentanil, but it is already widely used during neuroanaesthesia and is likely to represent a significant advance in several other areas such as cardiac and cardiovascular anaesthesia.
[Fig 2 ILLUSTRATION OMITTED]
Local anaesthetics
Bupivacaine
Bupivacaine is the most frequently used local anaesthetic for perioperative and postoperative pain relief in many countries. Onset of anaesthesia is rapid (within minutes), but the duration of action is comparatively long, sometimes lasting for several hours depending on the dose given and route of administration. In common with all local anaesthetics, bupivacaine can cause severe central nervous system and cardiovascular toxicity if given intravenously by mistake or if used in excessive doses by other routes.[20 21]
The bupivacaine molecule exhibits stereoisomerism, and recent studies comparing the two enantiomers have shown that R(+)-bupivacaine is 3-4 times more likely to cause cardiovascular toxicity than S(-)-bupivacaine in rabbit hearts.[22] Studies in sheep have shown a higher threshold for convulsions with the S(-) form.[23] Less cardiovascular disturbance has also been shown in humans with the S(-) form.[24] This improved safety profile is not at the expense of efficacy as S(-)-bupivacaine has been shown to be at least as good as racemic RS-bupivacaine when used either extradurally or for brachial plexus block.[25 26] Bupivacaine is likely to be generally available shortly and probably represents a significant advance in safety.
Ropivacaine
Ropivacaine is a new local anaesthetic with a structure similar to bupivacaine, but prepared only as the pure S(-) isomer.[27] The sensory anaesthesia produced is similar to that of bupivacaine but its central nervous system and cardiovascular toxicity profile in humans is superior to that of RS-bupivacaine.[28] During the course of clinical trials some patients have received accidental large intravenous doses of ropivacaine, but none has suffered harmful systemic toxicity.[29] In addition, it has been claimed that ropivacaine produces greater sensory motor separation when used by the epidural route,[30] allowing good analgesia with less intense motor block than bupivacaine.
Mobile epidurals
A recent advance in obstetric anaesthesia has been the introduction of mobile epidurals.[31] To produce adequate analgesia, traditional epidurals require the use of local anesthetics in concentrations that may produce significant motor neuronal blockade and consequent immobility. In contrast, mobile techniques usually depend on the epidural administration of a mixture of very low concentration local anaesthetic together with an opioid such as fentanyl. The lower concentration of local anaesthetic minimises motor block, whereas the opioid acts at opiate receptors in the central nervous system to enhance analgesia. The preserved mobility is often sufficient to allow walking, free of pain, which is popular with women in labour. [32] It has been suggested that the immobility and loss of muscle tone produced by traditional epidurals may delay progress in labour and cause increased rates of instrumental delivery and caesarian sections, a view supported by a recent comprehensive systematic review.[33] Large randomised multicentre studies are in progress to compare mobile epidurals with conventional epidurals in this respect. Mobile epidurals are currently rarely available outside large centres, partly because medical and midwifery staff require training. If beneficial effects on the numbers of normal deliveries are shown, however, we can expect mobile epidurals to become quickly more common.
Similar low concentration local anaesthetic-opioid mixtures have recently been used in epidurals for postoperative pain management, allowing improved and earlier mobilisation and greater patient satisfaction. Despite these benefits, the use of this technique is also limited because provision of an epidural service on general surgical wards requires support from an acute pain team.
Postoperative emesis
Postoperative nausea and vomiting remains a significant morbidity problem after general anaesthesia and the [5-HT.sub.3] antagonists have been shown to be at least as effective as standard antiemetics but with an improved side effect profile. [34 35] Postoperative nausea and vomiting remains a problem, however, and ongoing studies are investigating the efficacy of combination therapy (antagonising more than one receptor type) and the activity of the new neurokinin type 1 receptor antagonists. Preliminary studies of neurokinin type 1 receptor antagonists show promise. [36]
Equipment
Laryngeal mask airway
One of the most significant advances in anaesthesia in recent years has been the laryngeal mask airway. This device can be inserted blindly (without a laryngoscope), leaves the anaesthetist's hands free, and produces a close enough seal around the laryngeal inlet to allow spontaneous or, with certain provisos, positive pressure ventilation. Because of its simplicity of use, it is rare not to anaesthetise at least one patient on an operating list with a laryngeal mask airway. Since its introduction, anaesthetists have devised ways of using the laryngeal mask airway to facilitate tracheal intubation, either by passing an endotracheal tube blindly down the lumen of a correctly positioned layrngeal mask airway or by first using it as a guide for the passage of a fibreoptic laryngoscope.[37] Such techniques are invaluable in the management of patients who are difficult to intubate using direct laryngoscopy (an important cause of morbidity and mortality in anaesthesia), as studies have shown that the success rate for placement of the laryngeal mask airway in the abnormal airway is at least 97%. [38] These methods are, however, cumbersome, and only narrow endotracheal tubes can be inserted in this way. Recently a purpose designed intubating laryngeal mask airway has been described, which allows blind successful placement of endotracheal tubes up to 8.0 mm in diameter, a normal sized tube for use in adults. [39] This device should prevent many cases of failed intubation and, in any case, creates a safety margin by allowing oxygenation to continue while intubation is attempted.
McCoy laryngoscope
The McCoy laryngoscope is a recent aid for difficult intubations.[40] It is shaped like a standard Macintosh laryngoscope but has a hinged tip to its blade, which can be activated by a lever on the handle. Use of this hinged tip has been shown to improve the view of the larynx in a substantial proportion of difficult laryngoscopies,[41] and as a result the McCoy laryngoscope has become popular.
Competing interests: DJR has been reimbursed for attending several conferences and has received lecture fees from GlaxoWellcome (manufacturer of remifentanil).
Recent advances
New inhalational anaesthetics allow rapid, pleasant gaseous induction of anaesthesia and rapid recovery with a minimal "hangover" effect
Target controlled infusion techniques have improved the accuracy of total intravenous anaesthesia and pave the way for "dosed loop" automatic anaesthesia
A unique opioid, remifentanil, allows fine control of intraoperative analgesia but its effects wear off within minutes of stopping infusion
Separation of stereoisomers has allowed the development of improved safer local anaesthetics
Mobile epidurals are rapidly gaining popularity in labour wards because they allow normal mobility with high quality pain relief
Neurokinin type I receptor antagonists promise to further improve management of postoperative nausea and vomiting
Recent developments in equipment have helped to minimise the problems of anaesthetising patients with "difficult" airways
[1] Paris ST, Cafferkey M, Tarling M, Hancock P, Yate PM, Flynn PJ. Comparison of sevoflurane and halothane for outpatient dental anaesthesia in children. Br J Anaesth 1997;79:280-4.
[2] Biebyck JF, Eger EI. New inhaled anaesthetics. Anesthesiology 1994;80: 906-22.
[3] Smith I, Nathanson M, White PF. Sevoflurane--a long-awaited volatile anaesthetic. Br J Anaesth 1996;76:435-45.
[4] Jones RM, Cashman JN, Mant TGK. Clinical impressions and cardiorespiratory effects of a new fluorinated inhalational anaesthetic, desflurane(I-653), in volunteers. Br J Anaesth 1990;64:3-6.
[5] Zwass MS, Fisher DM, Wellborn LG, Cot CJ, Davis PJ, Dinner M, et al. Induction and maintenance characteristics of anaesthesia with desflurane and nitrous oxide in infants and children. Anesthesiology 1992;76:373-8.
[6] Patel SS, Goa KL. Desflurane--a review of its pharmacodynamic and pharmacokinetic properties and its efficacy in general anaesthesia. Drugs 1995;50:742-67.
[7] Ghouri AF, Bodner M, White PF. Recovery profile after desfluranenitrous oxide versus isoflurane-nitrous oxide in outpatients. Anesthesiology 1991;74:419-24.
[8] Lee DJH, Robinson DL, Soni N. Efficiency of a circle system for short surgical cases: comparison of desflurane with isoflurane. Br J Anaesth 1996;76:780-2.
[9] Goto T, Saito H, Shinkai M, Nakata Y, Ichinose F, Morita S. Xenon provides faster emergence from anaesthesia than does nitrous oxide-sevoflurane or nitrous oxide-isoflurane. Anesthesiology 1997;86:1273-8.
[10] Petersen-Felix S, Luginbohl M, Schnider TW, Curatolo M, Arendt-Nielsen L, Zbinden AM. Comparison of the analgesic potency of xenon and nitrous oxide in humans evaluated by experimental pain. Br J Anaesth 1998;81:742-7.
[11] Mirakhur RK, Morgan M. Intravenous anaesthesia: a step forward. Anaesthesia 1998;53(suppl 1):1-3.
[12] Gray JM, Kenny GNC. Development of the technology for `Diprifusor' TCI systems. Anaesthesia 1998;53(suppl 1):22-7.
[13] Russell D, Wilkes MP, Hunter SC, Glen JB, Hutton P, Kenny GNC. Manual compared with target controlled infusion of propofol. Br J Anaesth 1995;75:562-6.
[14] Gepts E. Pharmacokinetic concepts. Anaesthesia 1998;53(suppl 1):4-12.
[15] Mantzaridis H, Kenny GNC. Auditory evoked potential index: a quantitative measure of changes in auditory evoked potentials during general anaesthesia. Anaesthesia 1997;52:1030-6.
[16] Doi M, Gajraj RJ, Mantzaridis H, Kenny GNC. Relationship between calculated blood concentration of propofol and electrophysiological variables during emergence from anaesthesia: comparison of bispectral index, spectral edge frequency, median frequency and auditory evoked potential index. Br J Anaesth 1997;78:180-4.
[17] Kenny GNC, McFadzean W, Mantzaridis H, Fisher AC. Closed-loop control of anaesthesia. Anesthesiology 1992;77:A328.
[18] Egan TD. Remifentanil pharmacokinetics and pharmacodynamics. A preliminary appraisal. Clin Pharmacokinet 1995;29:80-92.
[19] Thompson JP, Rowbotham DJ. Remifentanil--an opioid for the 21st century. Br J Anaesth 1996;76:341-3.
[20] Albright GA. Cardiac arrest following regional anaesthesia with etidocaine or bupivacaine. Anesthesiology 1979;51:285-7.
[21] Rosenberg PH, Katso EA, Tuominen MK, Linden HB. Acute bupivacaine toxicity as a result of venous leakage under the tourniquet cuff during a Bier block. Anesthesiology 1983;58:95-8.
[22] Mazoit JX, Boico O, Samii K. Myocardial uptake of bupivacaine: pharmacokinetics and pharmacodynamics of bupivacaine enantiomers in the isolated perfused rabbit heart. Anesth Analg 1993;77:477-82.
[23] Mather LE, Huang YF, Veering BT, Pryor M. Comparative toxicity of bupivacaine and S(-)-bupivacaine in sheep: clinical implications, 11th World Congress abstract book. Anesthesiology 1996;137:F135.
[24] Gristwood R, Bardsley H, Dickens J. Reduced cardiotoxicity of S(-)-bupivacaine compared with racemic bupivacaine (marcaine): new clinical evidence. Expert Opinion Invest Drugs 1994;3:1209-12.
[25] Cox CR, Faccenda KA, Gilhooly C, Bannister J, Scott NB, Morrison LMM. Extradural S(-)-bupivacaine: comparison with racemic RS-bupivacaine. Br J Anaesth 1998;80:289-93.
[26] Cox CR, Checketts MR, Mackenzie N, Scott NB, Bannister J. Comparison of S(-)-bupivacaine with racemic (RS)-bupivacaine in supraclavicular brachial plexus block. Br J Anaesth 1998;80:594-8.
[27] McClure JH. Ropivacaine. A review article. Br J Anaesth 1996;76:300-7.
[28] Knudsen K, Beckman Suurkola M, Bloomberg S, Sjovall J, Edvardsson N. Central nervous and cardiovascular effects of intravenous infusion of ropivacaine, bupivacaine and placebo in healthy volunteers. Br J Anaesth 1997;78:507-14.
[29] Morton CP, Bloomfield S, Magnusson A, Jozwiak H, McClure JH. Ropivacaine 0.75% for extradural anaesthesia in elective caesarean section: an open clinical and pharmacokinetic study in mother and neonate. Br J Anaesth 1997;79:3-8.
[30] Brockway MS, Bannister J, McClure JH, McKeown DH, Wildsmith JAW. Comparison of extradural ropivacaine and bupivacaine. Br J Anaesth 1991;66:31-7.
[31] Elton CD, Ali P, Mushambi MC. "Walking extradurals" in labour: a step forward? Br J Anaesth 1997;79:551-4.
[32] Collis RE, Davies DWL, Aveling W. Randomised comparison of combined spinal-epidural and standard epidural analgesia in labour. Lancet 1995;345:1413-6.
[33] Howell CJ. Epidural versus non-epidural analgesia for pain relief in labour. Cochrane Database of Systematic Reviews. In: Cochrane Library. Cochrane Collaboration; Issue 1. Oxford: Update Software, 1999.
[34] Shende D, Mandal NG. Efficacy of ondansetron and metoclopramide for preventing postoperative emesis following strabismus surgery in children. Anaesthesia 1997;52:489-500.
[35] Capouet V, De Pauw C, Vernet B, Ivens D, Derijcke V, Versichelen L, et al. Single dose i.v. tropisetron in the prevention of postoperative nausea and vomiting after gynaecological surgery. Br J Anaesth 1996;76:54-60.
[36] Diemunsch P, Schoeffler P, Bryssine B, Cheli-Muller LE, Lees J, McQuade BA, et al. Antiemetic activity of the [NK.sub.1] receptor antagonist GR205171 in the treatment of established postoperative nausea and vomiting after major gynaecological surgery. Br J Anaesth 1999;82:274-6.
[37] Benumof JL. Use of the LMA to facilitate fiberscope-aided tracheal intubation. Anesth Analg 1992;74:313-4.
[38] Silk JM, Hill HM, Calder I. Difficult intubation and the laryngeal mask. Eur J Anaesthesiol 1991 ;4:47-51.
[39] Brain AIJ, Verghese C, Addy EV, Kapila A. The intubating laryngeal mask. I: development of a new device for intubation of the trachea. Br J Anaesth 1997;79:699-703.
[40] McCoy EP, Mirakhur RK. The levering laryngoscope. Anaesthesia 1993;48:516-9.
[41] Tuckey JP, Cook TM, Render CA. An evaluation of the levering laryngoscope. Anaesthesia 1996;51:71-3.
University Department of Anaesthesia, University of Leicester, Leicester Royal Infirmary, Leicester LEI 5WW Andrew J Fox lecturer David J Rowbotham professor
Correspondence to: DJ Rowbotham David. Rowbotham@leicester.ac.uk
BMJ 1999;319:557-60
COPYRIGHT 1999 British Medical Association
COPYRIGHT 2000 Gale Group