The Art of Prescribing
Because of the importance of maintaining current knowledge of technological advances involving genetics, neuroscience, and their impact on psychopharmacology, we have created a new column for advanced practice psychiatric nurses.
This new column offers a question-and-answer forum that can help nurses maintain their knowledge of advances in prescribing and psychopharmacology, and implications for safe psychiatric care. Deborah Antai-Otong has a wealth of knowl- edge and expertise with prescriptive authority and as a psychotherapist. She currently manages the care of patients with various psychiatric disorders including mood disorders, schizophrenia, dual diagnosis, and anxiety disorders. She is the author of numerous refereed journal articles and book chapters that focus on psychopharmacology and is a guest lecturer at a local university on this topic. She is also the author of several books, including Psychiatric Nursing: Biological and Behavioral Concepts (Clifton Park, NY: Delmar & Thompson Learning, 2003) and Psychiatric Emergencies (Eau Claire, WI, PESI, 2001).
Historically, psychopharmacology has been an integral aspect of psychiatric care. The dawning of this century has generated an explosion of scientific studies that enhance positive patient responses to various psychopharmacological agents with fewer adverse side effects. Likewise, contemporary advances in brain imaging, genetics, neuroscience, neuroendocrinology, and molecular sciences provide a plethora of data that enhance the understanding of the complexity of pharmacological effects and specific cellular activities associated with mental disorders. These data offer opportunities for advanced practice psychiatric nurses to implement integrated models of mental health care using pharmacological and psychotherapeutic interventions.
The rapid technological advances of psychopharmacology require a thorough understanding of these complexities and their impact on safe medication and symptom management. Issues such as culture, ethnopharmacology, gender, age, cultural practices, stigma, and patient preferences also play significant roles in patient responses to pharmacological interventions. Finally, advances in molecular biology indicate a number of genetic polymorphisms exist in some enzyme systems (e.g., P450) and lead to alterations in drug metabolism.
Question: How do you manage medications for clients who take multiple medications for multiple problems?
Answer: It is difficult to predict drug-to-drug interactions that are inherent in multiple medical conditions; however, understanding complex processes is essential to the nurse who administers or prescribes medications. A brief review of pharmacokinetics and pharmacodynamics is crucial to understanding the patient's response to pharmacotherapy. Drug interactions are often characterized as either pharmacokinetic or pharmacodynamic.
Pharmacokinetic interactions are those in which one drug alters the rate or degree of absorption, distribution, or elimination (metabolism or excretion) of another drug that may result in an increase or decrease in the concentration of the drug at the site of action. Key parameters include maximum serum concentration, half-life, total amount of drug excreted by the kidneys.
Pharmacodynamic interactions are those in which one drug induces change in a patient's response to the drug without altering the drug's pharmacokinetic properties. For example, an increase of toxicity (doubled level) of lamotrigine (Lamictel) resulting from an interaction with valproic add (Depakene).
Knowledge about the effect of various drugs on the cytochrome P450 enzymes is imperative, and enables the nurse to identify potentially serious or fatal drug-to-drug interactions. The metabolic conversion of drugs is normally enzymatic in nature. Most drug enzyme systems responsible for biotransformation of drugs occur in the liver, although every tissue has some metabolic potential.
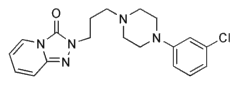
The cytochrome P450 isoenzyme system located in the endothelium of liver cells (hepatic microsomal enzymes) is involved in the metabolism of diverse compounds, including drugs (Hardeman, Limbird, & Gilman, 2001). The relevance of this enzyme system is its potential for various drugs to act as P450 inhibitors or inducers. A result of P450 inhibition, such as the effects of fluoxetine (Prozac) on trazodone (Desyrel), is an increase in the plasma concentration and prolonged pharmacological effects and likelihood of fluoxetine-induced toxicity of trazodone. A clinical implication of this situation is for the nurse to lower the dose of trazodone to reduce sedation, anticholinergic, and other potential drug-to-drug side effects. In contrast, P450 induction actions result in lower plasma levels and efficacy of one of the drugs. An example of induction of drug metabolism is carbamazepine (Tegretol), a P450 inducer, and birth control pills. The interaction between these two drugs results in an increased metabolism of BCPs caused by carbamazepine, resulting in lower plasma levels and efficacy in preventing pregnancy. A clinical implication from this situation is for the patient to use another form of birth control. In other cases, it may indicate a need to increase the dose of the second drug to maintain therapeutic serum levels.
The following considerations may also be helpful in handling potential drug-to-drug interactions:
1. Analyze data from a comprehensive database concerning the patient's physical and mental status that include pathophysiology of major organs such as the kidney and liver, genetic factors, drug allergies, developmental stage, and pregnancy.
2. Ask yourself the following questions:
a. What are the direct and physical interactions of each drug?
b. How does GI absorption affect each drug?
c. How does protein binding affect the drug concentration?
d. Which specific receptor sites will the drugs affect? Normally, the displacement of drugs from their receptor sites leads to a pharmacologic effect rather than drug interaction. For instance, a beta blocker, like propanolol (Inderal), may displace a beta agonist, such as albuterol (Proventil), from beta^sup 2^ receptors and increase the risk of bronchospasm or asthma attack (Hardeman et al., 2001; Hartshorn & Tatro, 1999).
3. Consult with the patients other healthcare providers and develop an integrated plan of care that addresses the management of both medical and psychiatric conditions.
As an advanced practice psychiatric nurse, you need to gather these data to use as a guide in the administration and prescription of multiple medications for co-- morbid medical and psychiatric conditions.
References
Hardeman, J.G., Limbird, L.E., & Gilman, A.G. (2001). Goodman & Gilman's The pharmacological basis of therapeutics (10th ed.). New York McGraw-Hill.
Tatro, D.S. (1999). Drug interactikon facts. St. Louis, MO: Facts and Comparisons.
Search terms: Drug interactions, cytochrome, P450, enzymes
Deborah Antai-Otong, MS, RN, CNS, NP, FAAN
Deborah Antai-Otong, MS, RN, CNS, NP, CS, FAAN
Mental Health Provider and Program Specialist Employee Support Program
VA North Texas Health Care System
Dallas, TX
Author contact: Deborah.Antai-otong@med.va.gov, with a copy to the Editor: mary@artwindows.com
Copyright Nursecom, Inc. Jan-Mar 2003
Provided by ProQuest Information and Learning Company. All rights Reserved