Study objectives: Pentoxifylline (POF) has been shown to suppress the cytokine production from lipopolysaccharide (LPS)-stimulated monocytes/alveolar macrophages (AMs). Sarcoidosis is a granulomatous disease that is driven by the action of tumor necrosis factor (TNF)-[alpha] and other proinflammatory cytokines. In this study, we aimed to investigate the effects of POF on the production of TNF-[alpha], interleukin (IL)-1[beta], IL-6, IL-8, IL-10, and the soluble TNF receptors (sTNFRs) 1 and 2 from AMs in sarcoidosis, and we also compared them with those of dexamethasone (DEX).
Methods: AMs from 14 patients with sarcoidosis were cultured for 24 h with RPMI medium alone or with LPS (100 ng/mL), and with POF at concentrations of 0.01, 0.1, and 1 mmol/L, or with 0.1 mmol/L DEX. Cytokines in the culture supernatants were analyzed by enzyme-linked immunosorbent assay.
Results: The results showed that POF induced a dose-dependent suppression of the spontaneous TNF-[alpha] release from AMs in sarcoidosis (p < 0.001), and that the spontaneous release of the other cytokines was unaffected by POF at all tested concentrations, but a trend for the inhibition of IL-10 production was found (p = 0.092). DEX inhibited the spontaneous release of TNF-[alpha] (p < 0.001), sTNFR2 (p < 0.05), IL-1[beta] (p < 0.05), and IL-10 (p < 0.01). POF also suppressed the LPS-stimulated production of these cytokines except for that of sTNFR1. Similar to POF, DEX inhibited the LPS-stimulated production of these cytokines, but not that of sTNFR1 and IL-1[beta].
Conclusions: Compared with DEX, POF may improve therapeutic regimens in patients with sarcoidosis either by sparing or by replacing corticosteroids. However, the precise clinical value of POF in the treatment of sarcoidosis and other lung diseases will have to be determined in further clinical trials.
Key words: alveolar macrophages; cytokine production; pentoxifylline; sarcoidosis
Abbreviations: AM = alveolar macrophage: DEX = dexamethasone; IL = interleukin; LPS = lipopolysaccharide; PBMC = peripheral blood mononuclear cell; PDE = phosphodiesterase: POF = pentoxifylline; sTNFR = soluble tumor necrosis factor receptor; Th = T helper; TNF = tumor necrosis factor
**********
Pentoxifylline (POF) is a methylxanthine that was used initially in therapy for peripheral vascular disease. (1) It has become evident that this drug has important effects on immune cells and immune-mediated phenomena. It is able to inhibit cytokine production by macrophages/monocytes and whole blood cells. Among its immunologic effects, the inhibition of POF on tumor necrosis factor (TNF) production is of great importance. (2-6) POF also suppresses the production of other cytokines from peripheral blood mononuclear calls (PBMCs) or whole-blood cells. (4,6-9) In contrast to the well-documented and commonly accepted anti-TNF-[alpha] activity of POF, its role in the inhibition of the production of other cytokines is still unclear and is sometimes controversial, with divergent effects observed depending on the experimental conditions. (4-8)
Sarcoidosis is a multiorgan disorder of unknown origin that is characterized in the affected organs by a T-lymphocyte-mononuclear phagocyte infiltration, granuloma formation, and distortion of the normal microarchitecture. (10) In the course of the sarcoid alveolitis, an abundance of cytokines, soluble cytokine receptors, and soluble adhesion molecules that are capable of attracting and activating immune cells, and of inducing and maintaining granulomas are released by alveolar macrophages (AMs), T cells, and epithelial cells. AMs behave as versatile secretary cells, which release a great variety of cytokines in sarcoidosis patients, including TNF-[alpha], interleukin (IL)-1, IL-6, IL-8, IL-10, IL-12, IL-15, granulocyte-macrophage colony-stimulating factor, and transforming growth factor-[beta]. [11-17]
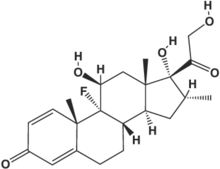
So far, there are no data regarding the effects of POF on the production of these cytokines from AMs in sarcoidosis, except for our previous report, which showed that POF inhibits the spontaneous production of TNF-[alpha] from AMs in sarcoidosis. (3) In this study, we were interested in investigating further the effects of POF on the soluble TNF receptors (sTNFRs) 1 mid 2, on the production of other cytokines, such as 1L-1[beta], IL-6, IL-8, and IL-10, from AMs in sarcoidosis, and in comparison with the effects of dexamethasone (DEX), which is a member of the glucocorticoid group of potent immunosuppressive and anti-inflammatory agents.
MATERIALS AND METHODS
Subjects
Fourteen consecutive patients with active pulmonary sarcoidosis (six women and eight men; age range, 32 to 58 years; all nonsmokers) were investigated. The diagnosis was established on the basis of compatible clinical and radiographic features, histologic evidence of noncaseating granulomata on transbronchial biopsy specimens, or an increased CD4/CD8 ratio in BAL fluid, and the exclusion of other granulomatous lung diseases. (18) The criteria of disease activity were as follows: (1) recently developed symptoms or increasing symptoms such as cough, dyspnea, weakness, fever, and arthralgia; and/or (2) chest radiographic evidence of progressive disease; and/or (3) deterioration of findings of lung function tests. According to chest roentgenographic staging, four patients had stage I disease, nine patients had stage II disease, and one patient had stage III disease. No patient was receiving treatment with steroids. Written informed consent was obtained according to institutional guidelines.
BAL Procedure
BAL was performed via a fiberoptic bronchoscope. Sterile isotonic saline solution was instilled into the right middle or left linguist lobe in 10 20-mL aliquots to a total volume of 200 mL, with immediate aspiration by gentle suction after the instillation of each aliquot. A volume of > 50% was retrieved. The recovered BAL fluid was filtered through two layers of sterile gauze and subsequently was centrifuged at 500g for 10 min at 4[degrees]C. The cells were counted in a hemocytometer. Cell viability was assessed by Trypan blue exclusion. Cell differentials were made on smears stained with May-Grunwald-Giemsa by counting 600 cells. Immunocytochemical staining was performed to obtain a CD4/CD8 count.
Cell Culture
AM cell cultures were performed as previously described. (14) After three washings with phosphate-buffered saline solution, the BAL cells were resuspended to a final concentration of 1 x [10.sup.6] cells/mL in RPMI 1640 medium supplemented with 10% heat-inactivated fetal calf serum, 2 mmol/L L-glutamine, 200 U/mL penicillin, and 200 [micro]g/mL streptomycin (Seromed; Biochrom KG; Berlin, Germany). The cell suspension was added at 1 x [10.sup.6] cells per well to a 24-well plastic tissue culture plate (Falkon; Becton Dickinson; Franklin Lakes, NJ) and was incubated at 37[degrees]C in a 5% C[O.sub.2] humidified atmosphere fur 1 h to permit the adherence of AMs. The nonadherent cells were removed by three washes with culture medium. The purity of the adherent AMs was identified to be > 95% by morphology and nonspecific esterase staining. The purified AMs were incubated for an additional 24 h with 1 mL RPMI 1640 medium alone, with 1 mL RPMI 1640 medium and lipopolysaccharide (LPS) [100 ng/mL; Sigma Chemical Co; St. Louis, MO], with 1 mL RPMI 1640 in the absence and presence of LPS (100 ng/mL) together with POF (Sigma) at concentrations of 0.01, 0.1, and 1 mmol/L, or with 0.1 mmol/L DEX (Sigma). The culture supernatants of the AMs were harvested and centrifuged, then were stored in fractions at -80[degrees]C until analysis.
Assay for TNF-[alpha], sTNFR1, sTNFR2, IL-1[beta], IL-6, IL-8, and IL-10
The concentrations of TNF-[alpha], sTNFR1, sTNFR2, IL-1[beta], IL-6, IL-8, and IL-10 in culture supernatants were quantified using commercially available human enzyme-linked immunosorbent assay kits (Endogen, Inc, Woburn, MA; sTNFR1 and sTNFR2, HyCult Biotechnology, Uden, the Netherlands) with sensitivity of 5, 25, 25, 1, 1, 2, and 3 pg/mL, respectively. The concentrations of above-measured TNF-[alpha], sTNFR1, sTNFR2, IL-1[beta], IL-6, IL-8, and IL-10 were expressed as picograms per milliliters per [10.sup.6] AMs after correction for the proportion of AMs.
Statistical Analysis
Data are expressed as the mean [plus or minus] SEM. The figures show the median and the 25th to 75th percentiles as box-plot diagrams. Within each group, the data were analyzed using Kruskal-Wallis one-way analysis of variance on ranks. A p value of < 0.05 was accepted as statistically significant.
RESULTS
Effects of POF and DEX on Spontaneous Cytokine Production From AMs in Sarcoidosis
As shown in Table 1, POF induced a dose-dependent suppression of TNF-[alpha] release. At a POF concentration of 0.1 mmol/L, the TNF-[alpha] release was 37% of the spontaneous production (p < 0.001), and a concentration of 1 mmol/L showed almost complete inhibition (Fig 1, top, A; p < 0.001). The spontaneous production of the other cytokines was not significantly inhibited by POF at all tested concentrations, but a trend for the inhibition of IL-10 production was found (Fig 2, top, A; p = 0.092). Similar to POF, DEX suppressed the spontaneous release of TNF-[alpha] (p < 0.001). In contrast to POF, DEX also reduced the spontaneous production of sTNFR2, IL-1[beta], and IL-10 to 78%, 48%, and 54%, respectively, of the spontaneous production (Fig 3, top, A; p < 0.05). No inhibitory effect of DEX on sTNFR1, IL-6, and IL-8 was seen.
[FIGURES 1-2 OMITTED]
Effects of POF and DEX on LPS-Stimulated Cytokine Production From AMs in Sarcoidosis
As shown in Table 2, the LPS-stimulated production of all cytokines was significantly higher than with spontaneous cytokine production (p < 0.05 and p < 0.001, respectively). POF suppressed the release of LPS-stimulated TNF-[alpha], sTNFR2, IL-1[beta], IL-6, and IL-8 production in a dose-dependent fashion (Fig 1, bottom, B, and Fig 3, bottom, B) [p < 0.05 or p < 0.001, respectively]. The LPS-stimulated release of IL-10 was inhibited by POF only at the highest dose (ie, 1 mmol/L) [Fig 2, bottom, B; p < 0.001]. Similar to POF, DEX also reduced the production of LPS-stimulated cytokines except for that of IL-1[beta](p < 0.001). POF and DEX showed no inhibition of LPS-stimulated sTNFR1 production.
[FIGURE 3 OMITTED]
DISCUSSION
The present study showed that POF induced a dose-dependent suppression of spontaneous TNF-[alpha] release from AMs in sarcoidosis, and that there was a trend for the inhibition of IL-10. DEX suppressed the spontaneous release of TNF-[alpha] sTNFR2, IL-1[beta], and IL-10 from AMs in sarcoidosis.
The rather selective inhibitory effect of POF on spontaneous TNF-[alpha] production from AMs in vitro in sarcoidosis, as shown in this study, is supported by the results of similar studies in vitro and in vivo. Previous studies (4,5) have demonstrated that the production of IL-1[beta], IL-6 and granulocyte-macrophage colony-stimulating factor from human monocytes/ AMs was unaffected by POF, whereas TNF-[alpha] production was markedly suppressed by POF. A study of POF on endotoxemia in human volunteers or in OKT3-treated renal transplant recipients had shown an inhibitory effect of POF on TNF-[alpha] levels, whereas IL-6 and IL-8 were not affected. (19) Bernard et al (20) reported a selective inhibition of POF oil TNF-[alpha] production by endothelial cells under LPS stimulation compared to that on IL-6. An in vivo study (21) on the effects of continuous IV infusion of POF on serum levels of TNF-[alpha], IL-6, and IL-8 in patients with septic shock showed a selective decrease of TNF-[alpha], whereas the levels of the other two cytokines remained unaffected. The lowest effective concentration of POF in our in vitro study (0.01 mmol/L) is comparable to peak therapeutic plasma concentrations of 0.1 to 0.01 mmol/L. (1) Other studies that investigated a comparable POF effect used higher concentrations than those required in vivo. (5)
A trend for the inhibition of spontaneous IL-10 production was seen in AMs from our results. Other studies also have demonstrated that the modulation of cytokine release induced by POF is not solely restricted to TNF. Bienvenu et al (8) also reported that IL-10 was significantly inhibited by POF at a concentration of 0.1 mmol/L. Benbernou et al (7) found that POF at appropriate concentrations induced a selective suppression of IL-2 and interferon-[gamma], whereas at high concentrations (ie, 0.5 mmol/L) this drug could act as a suppressive agent of both T helper (Th) type 1-derived and Th2-derived cytokines. D'Hellencourt et al (6) demonstrated that POF at a concentration of 1 mmol/L inhibited IL-10 production by LPS-stimulated whole-blood cell and PBMC culture, and also that POF induced a dose-dependent decrease in the TNF-[alpha], TNF-[beta], and IL-10 messenger RNA levels expressed by LPS-stimulated PBMCs. These findings are in disagreement with those of Rott et al(22) who considered POF to be a selective suppressor of Th1-associated lymphokine production but not of Th2-associated lymphokine production.
The mechanism of action of POF on cytokine inhibition is rather complex. The classic inhibition of phosphodiesterase (PDE) that is induced by POF is probably a major explanation, but is not the only one. The PDE inhibition is responsible for an elevation of the intracellular cyclic adenosine monophosphate level, which has a key role in controlling the activation and proliferation of monocytes/macrophages and of T and B lymphocytes. (23) Other mechanisms like modulation of calcium mobilization or interaction with adenosine receptors may be involved in the effects of POF and xanthine derivatives. (24,25) Another study (26) showed that the inhibitory effect of rolipram, a specific inhibitor of PDE IV, on TNF production is at least partially mediated by the endogenous production of IL-10. The presence of rolipram accelerated the IL-10 release by LPS-stimulated cells. Thus, different mediators secreted by the same cells are regulated by POF, probably using a distinct mechanism.
DEX, which is known for its multiple immunosuppressive and anti-inflammatory activities, has been widely used in the treatment of allergic and inflammatory granulomatous diseases, it has been shown to inhibit the production and gene expression of many cytokines, which are known to induce inflammatory or immunologic responses. (9,27-33) The molecular mechanism of the action of DEX is comparatively well-understood through its effect on the transcription factor nuclear factor-[kappa]B, which has been implicated in the activation of multiple cytokine genes. It has been demonstrated that DEX and POF inhibit TNF-[alpha] production at both the transcriptional and translational levels, with the effect of DEX being more pronounced at the translational level, but with POF inhibiting predominantly the transcription of the TNF-[alpha] gene. (2,4,34) Although POF and DEX inhibit TNF-[alpha] production by distinctly different mechanism, our results indicate that these drugs inhibit the production of the spontaneous TNF-[alpha] and other cytokines to a similar extent.
Shown by our in vitro studies of the LPS-stimulated cells and in line with those studies reported in the literature, POF not only inhibits TNF-[alpha] production, but also down-regulates other cytokines. (4-9,22) Based on these results, POF has complex effects on the cytokine network. The cellular environment and the mechanisms that trigger cytokine production seem to greatly influence these effects.
In sarcoidosis, AMs, AM-derived TNF-[alpha], and other cytokines play a crucial role in orchestrating inflammatory cell accumulation, granuloma formation, and the fibrogenesis of sarcoidosis. Accordingly, the results of our in vitro study may have important implications for the potential use of POF in the treatment of sarcoidosis, and also may explain in part the beneficial effect of POF on sarcoidosis patients what was observed in a 1997 open trial. (35) Compared with DEX, POF has no severe side effects and, thus, has a broader therapeutic window. (1) However, the lull details of the mechanism of how POF may be a promising immunosuppressive agent for the treatment of sarcoidosis have not yet been elaborated.
In conclusion, the results of this in vitro study show that POF not only inhibits the spontaneous production of TNF-[alpha] from AMs, but also suppresses the LPS-stimulated production of TNF-[alpha] and other cytokines from AMs. Compared with DEX, POF shows similar effects in regard to the inhibition of spontaneous and LPS-stimulated cytokine production. POF may improve the therapeutic regimens for sarcoidosis either by sparing or by replacing corticosteroids. However, the precise clinical value of POF in the treatment of sarcoidosis and other lung diseases will have to be determined in further clinical trials.
REFERENCES
(1) Ward A, Clissold SP. Pentoxifylline: a review of its pharmacodynamic and pharmacokinetic properties and its therapeutic efficacy. Drugs 1987; 34:40-97
(2) Han J, Thompson P, Beutler B. Dexamethasone and pentoxifylline inhibit endotoxin-induced cachectin/tumor necrosis factor synthesis at separate point in the signaling pathway. J Exp Med 1990; 172:391-394
(3) Marques LJ, Zheng L, Poulakis N, et al. Pentoxifylline inhibits TNF[alpha] production from human alveolar macrophages. Am J Respir Crit Care Med 1999; 159:508-511
(4) Neuner P, Klosner M, Schauer M, et al. Pentoxifylline in vivo down-regulates the release of IL-1, IL-6, IL-8, and tumor necrosis factor-[alpha] by human peripheral blood mononuclear cells. Immunology 1994; 83:262-267
(5) Poulakis N, Androutsos G, Kazi D, et al. The differential effect of pentoxifylline on cytokine production by alveolar macrophages and its clinical implication. Respir Med 1999; 93:52-57
(6) D'Hellencourt CL, Diaw L, Cornillet P, et al. Differential regulation of TNF[alpha], IL-1[beta], IL-6, IL-8, TNF[beta], and IL-10 by pentoxifylline. Int J Immunopharmacol 1996; 18:739-748
(7) Benbernou N, Esnault S, Potron G, et al. Regulatory effects of pentoxifylline on T-helper cell-derived cytokine production in human blood cells. J Cardiovasc Pharmacol 1995; 25(supp1):S75-S79
(8) Bienvenu J, Doche C, Gutowski MC, et al. Production of proinflammatory cytokines and cytokines involved in the TH1/TH2 balance is modulated by pentoxifylline. J Cardiovasc Pharmacol 1995; 25(suppl):S80-S84
(9) Moller DR, Wysocka M, Greenlee BM, et al. Inhibition of human interleuk-12 production by pentoxifylline. Immunology 1997; 91:197-203
(10) Costabel U. Sarcoidosis: clinical update. Eur Respir J 2001; 18(suppl):56s-68s
(11) Baughman RP, Strohofer SA, Buchsbaum J, et al. Release of tumor necrosis factor by alveolar macrophages of patients with sarcoidosis. J Lab Clin Med 1990; 115:36-42
(12) Minshall EM, Tsicopoulos A, Yasruel Z, et al. Cytokine mRNA gene expression in active and nonactive pulmonary sarcoidosis. Eur Respir J 1997; 10:2034-2039
(13) Prior C, Knight RA, Herold M, et al. Pulmonary sarcoidosis: patterns of cytokine release in vitro. Eur Respir J 1996; 9:47-53
(14) Zheng L, Teschler H, Guzman J, et al. Alveolar macrophage TNF-alpha release and BAL cell phenotypes in sarvoidosis. Am J Respir Crit Care Med 1995; 152:1061-1066
(15) Girgis RE, Basha MA, Maliarik M, et al. Cytokines in the bronchoalveolar lavage fluid of patients with active pulmonary sarcoidosis. Am J Respir Crit Care Med 1995; 152:71-75
(16) Moller DR, Forman JD, Liu MC, et al. Enhanced expression of IL-12 associated with Thl cytokine profiles in active pulmonary sarcoidosis. J Immunol 1996; 156:4952-4960
(17) Agostini C, Trentin L, Faced M, et al. Role of IL-15, IL-2, and their receptors in the development of T cell alveolitis in pulmonary sarcoidosis. J Immunol 1996; 157:910-918
(18) Hunninghake GW, Costabel U, Ando M, et al. ATS/ERS/ WASOG statement on sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis 1999; 16:149-173
(19) Zabel P, Schade U, Schlaak M. Inhibition of endogenous TNF formation by pentoxifylline. Immunobiology 1993; 187: 447-463
(20) Bernard C, Barnier P, Merval R, et al. Pentoxifylline selectivity inhibits tumor necrosis factor synthesis in the arterial wall. J Cardiovasc Pharmacol 1995; 25(suppl):S30-S33
(21) Zeni F, Pain P, Vindimian M, et al. Effects of pentoxifylline on circulating cytokine concentrations and hemodynamics in patients with septic shock: results from a double-blind, randomized, placebo-controlled study. Crit Care Med 1996; 24:207-214
(22) Rott O, Cash E, Fleischer B. Phosphodiesterasc inhibitor pentoxifylline, a selective suppressor of T-helper type 1, but not type 2, associated lymphokine production, prevents induction of experimental auto-immune encephalitis in Lewis rats. Eur J Immunol 1993; 23:1745-1751
(23) Rosenthal LA, Taub DL, Moors MA, et al. Methylxanthine induced inhibition of the antigen and the superantigen specific activation of T and B lymphocytes. Immunopharmacology 1992; 24:203-217
(24) Yang KD, Chuen HL, Shaio MF. Pentoxifylline augments but does not antagonize TNF[alpha]-mediated neuroblastoma cell differentiation: modulation of calcium mobilization but not cAMP. Biochem Biophys Res Commun 1995; 211:1006-1014
(25) Wells JN, Kramer GL. Phosphodiesterase inhibitors as tools in cyclic nucleotide research: a precautionary comment. Mol Cell Endocrinol 1981; 23:1-3
(26) Kambayashi T, Jacob CO, Zhou D, et al. Cyclic nucleotide phosphodiesterase type IV participates in the regulation of IL-10 and in the subsequent inhibition of TNF[alpha] and IL-6 by endotoxin-stimulated macrophages. J Immunol 1995; 155: 4909-4916
(27) Lew W, Oppenheim JJ, Matsushima K. Analysis of the suppression of IL-1[alpha] and IL-1[beta] production in human peripheral blood mononuclear adherent cells by a glucocorticoid hormone. J Immunol 1988; 140:1895-1902
(28) Wu CY, Fargeas C, Nakajima T, et al. Glucocorticoids suppress the production of interleukin 4 by human lymphocytes. Eur J Immunol 1991; 21:2645-2647
(29) Williams CMM, Coleman JW. Induced expression of mRNA for IL-5, IL-6, TNF, MIP-2 and IFN immunologically activated rat peritoneal mast cells: inhibition by dexamethasone and cyclosporin A. Immunology 1995; 86:244-249
(30) Tobler A, Meier R, Seitz M, et al. Glucocorticoids downregulate gene expression of GM-CSF, NAP/IL-8 and IL-6, but not of M-CSF, in human fibroblasts. Blood 1992; 79:45-51
(31) Fushimi T, Okayama H, Seki T, et al. Dexamethasone suppressed gene expression and production of interleukin-10 by human peripheral blood mononuclear cells and monocytes. Int Arch Allergy Immunol 1997; 112:13-18
(32) Waage A, Bakke O. Glucocorticoids suppress the production of tumour necrosis factor by lipopolysaccharide-stimulated human monocytes. Immunology 1988; 63:299-302
(33) Arya SK, Wong-Staal F, Gallo RC. Dexamethasone-mediated inhibition of human T cell growth factor and gamma-interferon messenger RNA. J Immunol 1984; 133:273-276
(34) Schmidt-Choudhury A, Furuta GT, Lavigne JA, et al. The regulation of tumor necrosis factor-[alpha] production in murine mast cells: pentoxifylline or dexamethasone inhibits IgE-dependent production of TNF-[alpha] by distinct mechanisms. Cell Immunol 1996; 171:140-146
(35) Zabel P, Entzian P, Dalhoff K, et al. Pentoxifylline in treatment of sarcoidosis. Am J Respir Crit Care Med 1997; 155:1665-1669
* From the Department of Pneumology and Allergy (Drs. Tong, Dai, Chen, Costabel, and Abdoh), Ruhrlandklinik, Medical Faculty, University of Essen, Essen, Germany; and General and Experimental Pathology (Dr. Guzman), Ruhr University, Bochum, Germany.
This work was supported by Arbeitsgemeinschaft zur Forderung der Pneumologie an der Ruhrlandklinik and by FORUM (University of Bochum).
Manuscript received December 18, 2002; revision accepted Marcia 18, 2003.
Correspondence to: Ulrich Costabel, MD, FCCP, Ruhrlandklinik, Tuschener Weg 40, 45239 Esse, Germany; e-mail: erj.costabel@t-online.de
COPYRIGHT 2003 American College of Chest Physicians
COPYRIGHT 2003 Gale Group