Pain is a phenomenon that has been experienced for ages with various severities, durations, and etiologies. Several mechanisms for pain have been postulated, as have mechanisms for the relief of pain. Recently discovered information on pain perception and amplification has pointed out the possible role of N-methyl-D-aspartate (NMDA) receptors in some types of pain and the potential efficacy of NMDA receptor antagonists in relieving this pain. This article examines the mechanisms of chronic pain, the functions of the NMDA receptor, and the actions of several known NMDA receptor antagonists; this information may shed light on future therapy for those who do not obtain pain relief and/or have intolerable side effects from standard treatment. A discussion of pharmacokinetic parameters and other studies provides a rationale for NMDA antagonist use in the treatment of pain. The importance of compounding in obtaining the full benefits of these agents and the potential for future therapies also are elucidated.
Mechanisms of Chronic Pain
Millions of individuals suffer from various chronic nonmalignant pain states. Standard therapy for these pain syndromes is burdensome and exposes patients to numerous side effects. Compounded NMDA antagonists such as dextromethorphan may alleviate pain with fewer side effects in some of these cases. To learn more, I conducted a literature search to identify papers discussing the use of NMDA receptor antagonists to treat pain in animal and/or human models. Articles related to chronic nonmalignant pain states were selected and reviewed. These articles revealed that NMDA antagonists are effective in chronic pain when used appropriately, tailored specifically for each patient, and their effects carefully monitored.
The pharmacology of pain relief is rather complex. It is easiest to understand if pain is viewed as a sensory process that involves a balance of inhibition and excitation. Lack of inhibition alone or excitation of neuronal sensory systems can lead to pain. Excitation sets up the framework for chronic pain as repeated excitation lowers the threshold for further stimulus by noxious stimuli. This theory, sometimes called "wind-up," holds that persons with a chronic nonmalignant pain state are predisposed to abnormally increased pain sensations in response to relatively mild stimuli. Although wind-up requires a certain, frequency of stimulation to produce its effects, once achieved responses are augmented 20-fold in amplitude and continue despite cessation of peripheral input.1 Maintenance of these excitatory states is enhanced in inflammatory conditions. The sensory system comprises two fibers to conduct afferent impulses to the spinal cord: A-delta fibers and C fibers, which are myelinated and unmyelinated sensory fibers, respectively. A-delta fibers are responsible for fast pain and C fibers for slow pain, with differences in transmission becoming apparent only when the stimulus originates far from the central nervous system (CNS), as in stubbing of a toe. The quick stabbing sensation when a toe is stubbed is fast pain, while the dull throbbing that ensues is slow pain. It is important to note that C fibers contain glutamate, whose significance is discussed in the next paragraph.
The spinal cord has the capability to alter its own circuitry and continuously modify stimulus and response, making it moldable or plastic. Several neurotransmitters are involved in this process, carrying excitatory and inhibitory signals through afferent transmission, but most interesting are the excitatory amino acids (EAA). There is considerable evidence that EAA (i.e., glutamate and aspartate) play a major role in the transmission and maintenance of noxious stimuli. There are three receptors for glutamate: AMPA, NMDA, and metabotropic receptors. The role of the metabotropic receptors is unknown. AMPA receptors play important roles throughout the CNS, and thus their antagonism would most likely produce extensive side effects. Research in mechanisms and control of chronic nonmalignant pain, therefore, has focused on the NMDA receptor.
Under normal circumstances, ion-mediated NMDA receptors are plugged with magnesium so that an acute noxious stimulus produces no response. If acute noxious stimulation continues, glutamate binds to the NMDA receptor and depolarization moves the magnesium out of its designated space, allowing calcium ions to flood into the cell. When this happens, the NMDA receptor has moved from a lower state of excitation to a higher state, and is "wound up." Repeated C-fiber stimulation is what induces the wound-up state. Only C-fiber stimulus that is maintained with adequate frequency and intensity is sufficient to activate the receptor. It has been shown that chronic pain phases that are a result of prolonged peripheral inflammation are sensitive to NMDA antagonism, whereas initial acute pain phases are not. It is for this reason that the NMDA receptor is thought to be involved in chronic pain states and maintenance of pain rather than the AMPA receptor, which maintains baseline levels of sensation. It stands to reason that, if NMDA is involved in inflammatory, neuropathic, and ischemic pain, then an NMDA antagonist may alleviate this pain.2
NMDA receptors are known to be involved in opioid sensitivity. NMDA receptor activation leads to excitation and increase in pain transmission. For analgesia to occur, this excitation must be balanced by inhibition. The buildup of intracellular calcium during wind-up contributes to opioid tolerance. Voltage-gated calcium channel blockade by NMDA antagonists reduces this buildup, reducing opioid tolerance. Neurons that are exposed to minimal amounts of morphine have high amounts of extracellular calcium, while repeated exposure to morphine causes buildup of calcium within these neurons. NMDA antagonism blocks this process. So NMDA not only can reduce opioid tolerance but prevent it. The addition of an NMDA antagonist to a pain therapy regimen can restore opioid efficacy and decrease necessary opioid doses for patients already on opioids.2'3
While many pharmacological treatments have been thought to be effective in chronic nonmalignant pain, their practical use is limited by fear of tolerance/addiction, intolerable anticholinergic side effects, or electrocardiographic changes. The nonopioid agents, commonly called adjuncts or adjuvants, have efficacy in certain pain syndromes and, despite their name, can actually be used as first-line therapy. Commonly used adjuncts for chronic pain syndromes include drugs used primarily as anticonvulsants, such as carbamazepine and gabapentin (although gabapentin has been used for many other illnesses, such as migraine headaches). Use of carbamazepine in treatment of chronic pain raises concerns because of the potential for drug interactions and need to monitor drag levels. Although it has been suggested that monitoring levels should be voluntary, since most patients show no signs or symptoms of toxicity, drug interactions byway of the cytochrome P-450 hepatic enzymes are inevitable. Gabapentin's usefulness is restricted in many pain states because of the high incidence of weight gain and somnolence in patients taking this drug.
Other adjuncts used in the treatment of chronic nonmalignant pain include tricyclic antidepressants (TCAs), selective serotoninreuptake inhibitors (SSRIs), monoamine oxidase inhibitors (AIAOIs), nonsteroidal anti-inflammatory drugs (NSAIDs), sedative/hypnotics, and muscle relaxants. In many cases, these are impractical because of food restrictions, need for blood level monitoring and dose adjustments, excessive cost, addiction potential, or severe toxicity. These limitations make NMDA receptor antagonists very attractive in the treatment of chronic pain syndromes.
Chronic Nonmalignant Pain Syndromes
One of the most common types of chronic nonmalignant pain is peripheral diabetic neuropathy (PDN). An estimated 6% of the US population suffers from diabetes, and it is estimated that anywhere from 30% to 50% of these individuals suffer from some form of neuropathy. Painful diabetic neuropathy is very troubling and disabling; even though the common misconception of PDN is numbness, PDN in most cases is actually an unusual burning and tingling sensation that can interrupt daily activities. The pain can be severe, and patients who do not receive adequate treatment have poorer quality of life, including sleep and mood disturbances. Painful diabetic neuropathy usually affects the feet and ankles (lower extremities); it affects the fingers and hands to a lesser degree.
Postherpetic neuralgia (PHN) is another type of neuropathic pain. This condition is a complication of infection with the Varicella zoster virus (VZV), or chicken pox. The virus remains latent in sensory nerve endings, often for many years; if it is reactivated, the person develops herpes zoster (HZ), or shingles, which occurs most often as a painful skin rash. While chicken pox typically is an infection of children, HZ occurs mostly in adults.4 A key factor in reactivation of VZV is immune system function; patients in immunocompromised states such as malignancy, HIV infection, use of immunosuppressant drugs (e.g., steroids), or diabetes are more subject to development of HZ and complications than immunocompetent individuals. Persons aged 50 years or older have a 20% chance of continuing to have pain 6 months after the onset of original HZ symptoms. Patients with HZ typically are treated with an antiviral agent to reduce the severity and duration of disease, along with a steroid and adjunctive analgesics (such as amitriptyline and gabapentin) to relieve the pain. This regimen does not afford complete pain relief in many patients, however, and these individuals may require opioids to provide adequate pain control, which often entails uncomfortable side effects.4
Fibromyalgia (FM; also called fibromyalgia syndrome) affects predominantly middle-aged women. The syndrome is characterized by musculoskeletal pain and often fatigue, disturbed sleep, and restless legs. An assortment of other syndromes occur frequently with FM. A cure for FM has not been found and treatment is largely symptomatic, including pain and sleep medications. Adjunctive medications such as TCAs, SSRIs, MAOIs, NSAIDs, anticonvulsants, sedatives/hypnotics, and muscle relaxants, as well as opioids, all have been tried in the treatment of this syndrome. In many cases, one or more of these agents is effective in relieving one symptom of FM while aggravating other symptoms or causing intolerable side effects (e.g., TCAs). Fibromyalgia may respond to treatment with an NMDA antagonist. In FM, central nociception in the dorsal horn of the spinal cord is due mainly to NMDA activation, and therefore NMDA antagonists are a logical treatment choice.5 NMDA receptor antagonists can improve pain symptoms in FM, and low-affinity compounds in high doses can create high-level NMDA receptor blockade.
Clinical Studies
Sindrup et al evaluated data to determine the number of patients who need to be treated to get 50% relief from chronic pain syndromes.6 Numbers needed to treat (NNT) studies have shown that there are generally three categories of therapy in pain management: therapies with NNTs of 2 to 3, which include TCAs, anticonvulsant drugs with sodium and calcium channel blocking properties, tramadol, levodopa, and dextromethorphan; therapies with NNTs of around 6, which include SSRIs and topical capsaicin; and therapies with much higher NNTs, such as mexiletine, which has an estimated NNT of 38. An analysis of dextromethorphan revealed an NNT of 1.9, although it should be noted that this was just one study with a small number of patients/' This value is comparable to results seen with TCAs, which are well known for their efficacy in neuropathies of different origins.6 Ketamine, a noncompetitive NMDA antagonist, is available only in intravenous form, and is associated with dissociative side effects.7 Of the NMDA antagonists, therefore, only dextromethorphan has practical value in the treatment of chronic nonmalignant pain.
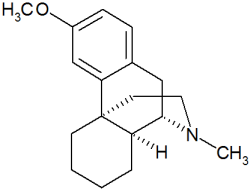
Even though dextromethorphan is the D-isomer of levorphanol (a codeine analog), it has no clinically significant effect on the opioid receptors and thus lacks morphine-like properties. Dextromethorphan acts on the cough center in the medulla oblongata, which raises the threshold for the cough reflex. It is well absorbed from the gastrointestinal tract, metabolized in the liver (first-pass effect), and excreted in the urine either unchanged or as dextrorphan, which also has cough-suppressing activity. Dextromethorphan has an established safety record as an antitussive in doses up to 400 mg/day with no respiratory or hemodynamic side effects.8,9 It does not exhibit euphoric properties, although it dilates pupils and increases blood pressure. Jasinski investigated its use with opioids such as morphine to assess whether dextromethorphan could increase morphine's abuse potential, but the results of this study were negative. He concluded that dextromethorphan does not potentiate the euphoric effects of morphine, that morphine suppresses the dysphoric effects of dextromethorphan, and that morphine suppresses the increases in pupil size, pulse, and blood pressure that are caused by dextromethorphan. Therefore, dextromethorphan does not enhance or reduce the euphoric action exhibited by morphine and its derivatives.10 Moreover, dextromethorphan does not affect the physical dependence or respiratory depression that accompany opioid use.10 In one study, patients reported better pain relief with dextromethorphan/morphine combinations than with much higher doses of morphine alone."These patients required no increase in dose over the 10-month treatment period, indicating that dextromethorphan prevents opioid tolerance and lowers required doses of morphine.11,12
Nelson et al studied the use of high-dose dextromethorphan in PDN and PHN in 26 patients, and found statistically significant pain reduction, as measured by a validated 13-word descriptor scale, by 24% in patients with PDN (P = 0.014).13 Average daily doses in these patients were 152 mg, 236 mg, 322 mg, 382 mg, 392 mg, and 381 mg for weeks 1 to 6, respectively. No differences were reported in duration of disease or concomitant medications between good and poor responders. This study did not, however, find any significant pain reduction in patients with PHN, even though these patients received higher mean daily doses of dextromethorphan than the patients with PDN. At the end of the 6-week trial, the average dose in patients with PHN was 439 mg. Only at the very end of the treatment period did these patients report pain relief, which was very slight. No period effect or period-treatment interaction ("carryover effect") was eminent (P = 0.74 and P = 0.27). Four patients who were taking regularly prescribed opioids did not prefer dextromethorphan. Adverse effects, dizziness and light-headedness, occurred most often during the titration phase; only two patients experienced such effects during the maintenance phase. Dextromethorphan caused no hyperglycemic or hypoglycemic reactions as confirmed by blood glucose and glycosylated hemoglobin measurements.
Subjects who continued treatment in the open-label portion of the study remained at the same dextromethorphan maintenance dose that they had received during the blinded part of the study, and no side effects were reported. Two patients who continued treatment in the open-label follow-up experienced what appeared to be a mild withdrawal phenomenon, which can be avoided by tapering the dextromethorphan dose over 1 week. In their discussion, the authors of this study report proposed a hypothesis that the difference in results of patients with PDN and PHN could be attributed to mixed central and peripheral neuropathic pain mechanisms in PHN. They also theorized that the NMDA channel blockers are effective in preventing noxious input that occurs in diabetics but not in patients with PHN. Pain relief from dextromethorphan was equivalent to that from TCAs (amitriptyline and desipramine) in previous studies of patients with PDN. The authors concluded by saying that they could not recommend high-dose dextromethorphan for treatment of chronic pain because it is available only in combination forms that can be problematic if taken at doses of greater than 120 mg/day.
In another study, Sang et al evaluated dextromethorphan and memantine, another low-affinity NMDA receptor antagonist, versus active placebo (lorazepam)." Median doses of dextromethorphan, memantine, and lorazepam for patients with PDN or PHN were 400 mg/day, 55 and 35 mg/day, and 1.8 and 2.2 mg/day, respectively. All three drugs were dispensed as externally identical capsules. Efficacy data showed that, in patients with PDN, dextromethorphan reduced pain intensity by a mean of 3 3 % from baseline, while memantine and lorazepam reduced pain intensity only 17% and 16%. Pain intensity was reduced by much less in patients with PHN, and the highest efficacy in these patients was that of dextromethorphan (6%). Interestingly, subjects who responded to dextromethorphan had a significant dose-response effect in terms of pain relief (P = 0.035). Maximally targeted doses (MTDs) of dextromethorphan, memantine, and lorazepam were 960, 58, and 2 mg, respectively. In patients who received dextromethorphan, only the MTD yielded a significant reduction in mean pain intensity (primary end point; P = 0.035 and r^sup 2^ = 0.93); doses equivalent to 25%, 50%, or 75% of the MTD did not yield significant relief. Dextromethorphan seemed to play a significant role in the emotional well-being of patients with PDN (P = 0.01) as demonstrated by quality of life (SF-36) data; patients who received dextromethorphan had a dramatic improvement from baseline, whereas all other groups showed only slight change. Unblinding of active placebo (lorazepam) in this study had no effect on response rates. The most common adverse events in the study were sedation, dry mouth, and gastrointestinal distress, which all appeared in the titration phase; no new events emerged during the maintenance phase. In their discussion, the authors reasoned that patients with PDN might have gotten better pain relief because these patients received higher mean doses of dextromethorphan. Even the MTD of memantine and lorazepam were unsuccessful in both treatment groups. The NNT for dextromethorphan was 3.2, making it comparable to opioids and traditional adjuncts such as gabapentin, TCAs, and tramadol. This study concludes that PDN patients achieved pain relief from high-dose dextromethorphan because the neuropathy is caused primarily by axonal degeneration, whereas patients with PHN are in an axonal degeneration stage only in the first few months after the acute episode, making NMDA receptor blockade ineffective later in the disorder. Both Nelson et al and Sang et al did mention that their study populations were not large enough for adequate power analyses, making the results of secondary endpoints difficult to evaluate.
Two NMDA antagonists have been reviewed for their use in FM. Ketamine has been given intravenously and orally in several small studies varying from 5 to 29 subjects. Although there is a certain usefulness to ketamine, cognitive side effects, especially from intravenous preparations, limit its applicability.14 Oral ketamine's safety and efficacy make it a more promising choice. Dextromethorphan is an alternative in FM patients; side effects are dose related and so optimal dosing is key.
Dextromethorphan has also been considered in the treatment of phantom pain. Phantom limb pain was initially described as a sensation of pain in a body part that has been amputated; while first associated with missing limbs, it has more recently been associated with other body parts such as the breast and penis. It has been reported that as many as 66% of patients who undergo amputation will experience phantom limb pain within the first 6 months after their surgery and, of these patients, 5% to 10% will continue to have severe, persistent, and disabling pain that is resistant to conventional therapy. Phantom pain has been given various explanations and, even though peripheral and central mechanisms have been postulated, the underlying mechanisms are still obscure. Some evidence has pointed to NMDA receptor involvement and so the efficacy of ketamine and dextromethorphan have been studied. Ketamine has not gained as much popularity because of its patenterai route of administration and dissociative side effects.
Ben Abraham et al conducted a study in patients with phantom pain in which subjects were evaluated psychologically, neurologically, and metabolically because of the sensitive nature of their pain.15 Single doses of dextromethorphan greater than 100 ing were not allowed in the study, since previous trials had found that doses greater than 100 mg cause substantial side effects. For ethical reasons, the drugs the patients were taking for pain before the study (acetaminophen, NSAIDs, morphine and derivatives, anticonvulsants, TCAs, and others) were not discontinued unless the subjects themselves discontinued them. Patients received dextromethorphan 60 or 90 mg twice daily or placebo, and patients who received dextromethorphan experienced reduction in pain by at least 50%, better mood, and less sedation. One patient who received dextromethorphan 90 mg twice daily reported exacerbation of pain, but the reasons for this were unclear. Doses of 120 mg to 270 mg per day were effective in relieving pain without adverse side effects or excessive sedation for almost 4 months. Because of the small number of patients and psychosocial factors, the study could not conclude whether pain intensity was confounded by other obscure causes.
Metabolism of Adjunctive Pain Medications
Phenotypic differences in cytochrome P-450 2D6 (CYP 450) metabolism complicate treatment with dextromethorphan. In the white European population, 81% are extensive metabolizers (EM), 13% are poor metabolizers (PM), and the remaining 6% are intermediates, falling in between. The PM phenotype is an inherited autosomal recessive trait that has pharmacokinetic consequences on many drugs, including beta-blockers, TCAs, neuroleptics, codeine, and a few other opioids.16 In humans, dextromethorphan is metabolized to dextrorphan by the polymorphic CYP 2D6. Desmeules et al showed that PM have significant increases in objective and subjective pain thresholds (45% and 35%, respectively) if 50 mg of quinidine sulfate, a selective inhibitor of CYP 2D6 (which blocks the O-demethylation of dextromethorphan to dextrorphan in humans) is administered along with 50 mg of dextromethorphan. These authors concluded that phenotypic differences in this polymorphic enzyme have major impacts on antinociceptive and neuromodulatory effects of dextromethorphan."
Related to the issue of CYP 2D6 enzyme is the potential for serotonin (indolamine) syndrome. Although not easily diagnosed or attributable to specific causes, serotonin syndrome typically occurs in a few specific scenarios. The list of signs and symptoms observable in a patient with serotonin syndrome is extensive, ranging from mental status and behavior changes (agitation, confusion, disorientation) to musculoskeletal consequences (myoclonus, rigidity, ankle clonus, incoordination) to autonomie instability (fever, nausea, diarrhea, diaphoresis, tachycardia, tachypnea, pupillary dilation) and positive Babinski sign, just to name a few. The three main scenarios in which a patient may develop the syndrome are enhanced serotonin availability (e.g., in a patient taking trazodone), decreased serotonin reuptake (e.g., in a patient taking an SSRI or trazodone), and decreased serotonin breakdown (e.g., in a patient taking an MAOI). Serotonin syndrome usually occurs after initiation or escalation of a serotomimetic agent alone or in combination with an MAOI. The MAOIs inhibit an enzyme that increases levels of serotonin, used commonly in the treatment of resistant depression. case reports of increased serotonin levels and serotonin syndrome in settings of treatment with SSRIs, trazodone, dextromethorphan, and many other agents have been reported, usually with concomitant use of an MAOI, although not always. Even though the syndrome usually resolves without any specific treatment, it can be fatal. Treatment of the syndrome includes withdrawal of offending agents, supportive measures (fluids, antipyretics), benzodiazepines if indicated for muscle rigidity, propranolol if indicated for heart rate control, and a serotonin receptor antagonist to shorten the syndrome's duration. One patient who received dextromethorphan while on phenelzine (an MAOI) developed high fever and fatal coma; the literature reports that the cause of death was unclear. Most significantly, MAOIs are irreversible, so replacement of depleted enzyme can take up to 2 weeks. In some cases, as with fiuoxetine, a 4- to 6-week washout period is recommended because of the long half-lives of either the parent drug or its metabolite. FIuoxetine's metabolite, norfluoxetine, has a half-life of 19 days, and long-term high-dose fluoxetine requires a 3-month washout period. Despite the countless uses of fluoxetine and the other SSRIs (obsessive-compulsive disorder, eating disorders, posttraumatic stress disorder, anxiety and panic disorders), caution should be used when combining amphetamines and/or SSRIs and/or dextromethorphan with an MAOI.17
Compounding of Dextromethorphan
Since dextromethorphan capsules are not commercially available, many compounding pharmacies have formulated 15-, 27-, 30-, and 60-mg capsules with lactose as fillers. Proposed dosing regimens are 15 to 30 mg every 6 hours or 10 to 30 mg six times daily, which can be modified to a three times daily regimen once the patient has been initiated on dextromethorphan therapy and is ready to move to maintenance dosing. Maximum doses of 240 mg/day have been compounded and are considered safe. Furthermore, when topical compounds are applied to the site of pain every 1 to 2 hours as needed, even as little as three times a day on a regular basis, the results are encouraging. Topically administered medication is usually formulated in either Pluronic lecithin organogel (PLO) or a vanishing-penetrating base; PLO is predominant.
As its name implies, PLO is an emulsion of Pluronic gel and lecithin.18 The most common form of Pluronic gel used in the compounding market today is Pluronic F-127 (PF-127). PF-127 has unique physiologic characteristics: as it warms it becomes a semisolid (gel), and as it cools it becomes a liquid (i.e., thermoreversible gelation). Apparently thermoreversible gelation is best achieved only at concentrations of 20% and greater. Pluronic concentrations of 30% and 35% are used in some compounding pharmacies, and these thicker gels have been successful. Viscosity is increased as proportionately more Pluronic is present than water; the higher the concentration, the more viscous the gel Pluronic is a permeation enhancer; it is a very stable compound that does not irritate the skin even when left on for extended periods. PF-127 has been found to have zero-order kinetics, meaning that the delivery of drug is constant.
Lecithin is derived from the soy plant. It enhances the gel and makes it more suitable and consistent for topical drug delivery. The lecithin does not seem to alter the gel in any other ways that detract from its primary purpose.18
The PLO can be made before any drug is added and is very simple to make. Shear forces combine Pluronic and lecithin to produce micelles, phospholipid bilayers that are small and uniform in size. Many drugs can be administered topically in PLO to avoid first-pass metabolism or side effects from oral administration. Pain medications such as gabapentin, amitriptyline, carbamazepine, and lidocaine formulated in PLO are very useful. The PLO gel has the property of allowing administration of highly polar drugs; its ability to form micelles around the drug allows the drug to permeate through the skin. Although little has been published on PLO, it has been used for many years in compounding, as a vehicle for hydrophilic and lipophilic compounds to be delivered transdermally.18 The Professional Compounding Center of America (PCCA) and other pharmacy compounding support organizations and companies have several formulas and recipes that the compounding pharmacist can use to make PLO as a topical vehicle for delivery of drugs. Formulations are also available in other pharmacy journals, including the International Journal ofPhamiMceutical Compounding, Major advantages of PLO gels over other topical gels are compatibility with many systems, low toxicity, no need for any neutralizer, and surfactant properties that enhance permeation.
It is important to note that topical dextromethorphan 5% to 10% in a gel is effective without concern for side effects and/or possible interactions with concomitant medications." Ketamine in a topical gel formulation also has been studied, with notable results. Topical application of ketamine has the benefit of preventing most if not all of the cognitive side effects that result from intravenous administration. In a small study by Crowley et al, five subjects who had spent years trying to achieve pain relief through numerous physician visits and pain medications became pain free with varying doses of ketamine PLO.20 The list of procedures, surgeries, and medications that these subjects endured is massive. Ketamine PLO not only controlled pain 100% in all patients but presented no side effects, even with high doses (700 mg/day). Ketamine 5% and 10% have been compounded in PLO, and these formulations are stable, consistent, and effective.7,20 These compounded topical preparations are given 6-month beyond-use dates to ensure the quality of the final product.
Compounds of dextromethorphan alone and in combination with morphine have been prepared and have shown excellent results, especially in patients whose pain is refractory to standard treatment and/or those with opioid tolerance. The dextromethorphan and morphine dosages can be adjusted to meet the individual needs of the patient. This has shown to not only prevent opioid tolerance but reverse tolerance in patients who require high dosages of morphine for acceptable pain control."
Other NMDA antagonists, including memantine and amantidine, need further investigation to determine whether they offer applicability, efficacy, and practicality for patients with chronic pain. One study consisting of 24 patients found that memantine (average daily dose, 20 mg) was no more effective than placebo in PHN.8 Only several small studies have been conducted and the results are conflicting; the reason for this is unknown. Although theoretically the mechanisms of these agents are similar or identical to that of dextromethorphan, a well-designed, large study would shed light on the matter, potentially justifying their use.
Conclusion
Both animal and clinical research indicates that there is a place for dextromethorphan and other NMDA receptor antagonists in control of chronic nonmalignant pain. For patients with chronic pain, a single daily dose of 30 to 90 mg seems to be effective in managing pain symptoms and reducing analgesic requirements. Compounding pharmacists can tailor the therapy to the individual needs of patients, as there is much room for improvement in the available dosage forms. Further clinical trials are needed to determine optimal dosage regimens to minimize untoward effects and length of treatment necessary in chronic pain conditions to prevent relapse of symptoms.
Acknowledgment
The author would like to thank Cheslav Berg, PharmD, MS, and the staff of Compounding Pharmacy of Beverly Hills for their editorial contributions to this article.
References
1. Dickenson AH. Spinal cord pharmacology of pain. Br J Anaesth1325; 75(2): 193-200.
2. Dickenson AH, Chapman V, Green GM. The pharmacology of excitatory and inhibitory amino acid-mediated events in the transmission and modulation of pain in the spinal cord. Gen Pharmacol 1997; 28(5): 633-638.
3. Kane DL, Glasnapp A. Dextromethorphan hydrobromide and opioid tolerance: A compounding opportunity for pharmacists with chronic pain patients. IJPC 1998; 2(2): 118-119.
4. Johnson RW, Dworkin RH. Treatment of herpes zoster and postherpetic neuralgia. BMJ 2003; 326(7392): 748-750.
5. Henriksson KG, Sorensen J. The promise of N-methyl-D-aspartate receptor antagonists in fibromyalgia. Rheum Dis Clin North Am 2002; 28(2):343-351.
6. Sindrup SH, Jensen TS. Efficacy of pharmacological treatments of neuropathic pain: An update and effect related to mechanism of drug action. Pain 1999; 83(3): 389-400.
7. Wood RM. Ketamine for pain in hospice patients. IJPC 2000; 4(4): 253-254.
8. Weinbroum AA, Rudick V, Paret G et al. The role of dextromethorphan in pain control. Can J Anaesth 2000; 47(6): 585-596.
9. Sang CN, Booher S, Gilron I et al. Dextromethorphan and memantine in painful diabetic neuropathy and postherpetic neuralgia: Efficacy and dose-response trials. Anesthesiology2002; 96(5): 1053-1061.
10. Jasinski DR. Abuse potential of morphine/dextromethorphan combinations. J Pain Symptom Manage 2000; 19(1 Suppl): S26-S30.
11. Chevlen E. Morphine with dextromethorphan: Conversion from other opioid analgesics. J Pain Symptom Manage 2000; 19(1 Suppl): S42-S49.
12.HeiskanenT, Hartel B, Dahl ML et al. Analgesic effects of dextromethorphan and morphine in patients with chronic pain. Pain 2002; 96(3): 261-267.
13.Nelson KA, Park KM, Robinovitz E et al. Highdose oral dextromethorphan versus placebo in painful diabetic neuropathy and postherpetic neuralgia. Neurology 1997; 48(5): 1212-1218.
14. Bern J, Peck R. Dextromethorphan: An overview of safety issues. Drug Sat 1992; 7(3): 190-199.
15. Ben Abraham R, Marouani N, Weinbroum AA. Dextromethorphan mitigates phantom pain in cancer amputees. Ann Surg Oncol 2003; 10(3): 268-274.
16.Desmeules JA, Oestreicher MK, Piguet V et al. Contribution of cytochrome P-4502D6 phenotype to the neuromodulatory effects of dextromethorphan. J Pharmacol Exp Ther 1999; 288(2):607-612.
17.Bodner RA, Lynch T, Lewis L et al. Serotonin syndrome. Neurology 1995; 45(2): 219-223.
18. [No author listed.] The history of Pluronic lecithin organogel: An interview with Marty Jones, BSPharm, FACA, FIACP. IJPC 2003; 7(3): 180-183.
19. Jones M. Clinical nuggets and pearls: Chronic neuropathic pain and opioid tolerance. IJPC 2002; 6(1): 4-6.
20. Crowley KL, Flores JA, Hughes CN et al. Clinical application of ketamine ointment in the treatment of sympathetically maintained pain. IJPC 1998; 2(2): 122-127.
Emilyn S. Mishkan, PharmD
Ralphs Pharmacy
West Los Angeles, California
Address correspondence to Emilyn S. Mishkan, PharmD, Ralphs Pharmacy, 12331 Gorham Ave., Los Angeles, CA 90049. E-mail: ejmishkan@yahoo.com
Copyright International Journal of Pharmaceutical Compounding Sep/Oct 2005
Provided by ProQuest Information and Learning Company. All rights Reserved