Study objectives: Benzodiazepines are commonly administered to medical ICU (MICU) patients. Propylene glycol (1,2-propanediol) is the solvent used to deliver lorazepam and diazepam IV. Although propylene glycol toxicity is increasingly recognized and reported, its incidence is unknown. Herein, we describe five MICU patients who acquired severe propylene glycol toxicity due to IV lorazepam or diazepam administration. Additionally, we evaluate the incidence of propylene glycol toxicity in MICU patients receiving 1V lorazepam or diazepam.
Design: Case series and prospective, observational study.
Setting: Eighteen-bed MICU in a 550-bed urban academic hospital.
Patients and methods: MICU patients administered IV benzodiazepines during a 3-month period were enrolled. Patients were categorized according to the IV benzodiazepine that they received. Laboratory data and highlights of their clinical course were recorded daily. The incidence of propylene glycol toxicity was determined and the groups compared.
Results: Forty-four patients were enrolled. Twenty-one patients received a benzodiazepine delivered in propylene glycol (lorazepam or diazepam), and 23 patients received a benzodiazepine delivered in an alternative solvent (midazolam). We found that four patients (19%) who received IV lorazepam or diazepam had metabolic evidence of propylene glycol toxicity. None of the patients had clinical deterioration. Neither metabolic abnormality nor clinical deterioration suggestive of propylene glycol toxicity were identified in subjects receiving IV midazolam.
Conclusion: Propylene glycol toxicity is a potentially life-threatening iatrogenic complication that is common and preventable. It should be considered whenever a patient has an unexplained anion gap, unexplained metabolic acidosis, hyperosmolality, and/or clinical deterioration. Close monitoring of all patients receiving IV lorazepam or diazepam for early evidence of propylene glycol toxicity is warranted.
Key words: anion gap; benzodiazepine; diazepam; hyperosmolality; lactic acidosis; lorazepam; metabolic acidosis; osmolar gap; propylene glycol; sedation
Abbreviation: MICU = medical intensive care unit
**********
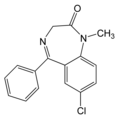
In the medical ICU (MICU), benzodiazepines are routinely administered IV to sedate patients receiving mechanical ventilation or to treat alcohol withdrawal, nausea, and anxiety. Propylene glycol (1,2-propanediol) is the vehicle used to deliver diazepam and lorazepam IV. It is considered safe for use as a vehicle for IV medications by the US Food and Drug Administration. (1-3)
Despite the reputation of propylene glycol for safety, propylene glycol toxicity has been reported. Adverse effects from propylene glycol have occurred when used to deliver topical sulfadiazine silver cream, (3-5) IV nitroglycerine, (6) etomidate, (7) enoximone, (8) multivitamins, (9-10) and phenytoin. (11) The adverse effects attributed to propylene glycol include hyperosmolality, (1,3-13) hemolysis, (4,14) cardiac arrhythmia, (3,11) seizure and coma, (3,9-10,15) and agitation. (16) Additionally, propylene glycol toxicity can mimic sepsis or systemic inflammatory response syndrome presenting with lactic acidosis, (1,3-12) hypotension, (12) and multisystem organ dysfunction. (12)
Propylene glycol toxicity due to administration of IV lorazepam or diazepam is being increasingly recognized and reported, (11,12,17-21) We previously reported a case of acute, life-threatening multisystem organ dysfunction due to propylene glycol toxicity during treatment of alcohol withdrawal with high-dose IV diazepam. (12) Since our case report, (12) we have observed five cases of severe propylene glycol toxicity in our MICU. Additionally, three cases have been reported by other groups. (17-19)
Our additional cases, the growing number of case reports, and reports of similar cases that we received from other physicians prompted us to perform a prospective, observational study to determine the incidence of propylene glycol toxicity in MICU patients receiving IV benzodiazepines. In this report, we describe the five additional cases and the observational study. Surprisingly, we found that propylene glycol toxicity is a common cause of metabolic abnormalities in the MICU patient population and can be life threatening.
MATERIALS AND METHODS
Design
The study was a prospective, observational study performed in the MICU of a large urban hospital.
Subject Enrollment
All patients admitted to the MICU during a 3-month period were screened for inclusion in our study. This was the anticipated duration necessary to enroll 25 patients per group, the number required to achieve a statistical power of 80%. Eligible patients met one of the following criteria: (1) continuous IV benzodiazepine for > 24 h; or (2) IV benzodiazepine by bolus injection totaling [greater than or equal to] 500 mg of diazepam over the previous 24 h, [greater than or equal to] 50 mg of lorazepam over the previous 24 h, or [greater than or equal to] 50 mg of midazolam over the previous 24 h. There were no exclusion criteria.
Data Collection
Data were acquired by chart and computer database review. Age, gender, admitting diagnosis, comorbidities, alcohol history, electrolytes, BUN, creatinine, albumin level, liver function, and toxicology results were recorded at the time of enrollment. Thereafter, electrolytes, BUN, creatinine, anion gap, arterial blood gas, benzodiazepine dose over the previous 24 h, and cumulative benzodiazepine dose were recorded daily.
Increase of the anion gap and decrease of serum bicarbonate are early signs of lactic acid accumulation, a byproduct of propylene glycol. Therefore, if a patient's anion gap has increased or serum bicarbonate has decreased without an obvious cause, the lactic acid level and osmolality were measured per MICU standard of care. The former confirms lactic acid accumulation, and the latter can determine whether accumulation of propylene glycol is a possible etiology. Abnormality of either could be followed by measurement of the propylene glycol level. The diagnostic approach could be altered at the discretion of the attending physician. An increase in anion gap was defined as an increase of [greater than or equal to] 4 mmol/L, and a decrease in serum bicarbonate was defined as a decrease of [greater than or equal to] 4 mmol/L. Once a subject was enrolled, data collection continued until the IV benzodiazepine was discontinued.
Data Analysis
Patients receiving diazepam and/or lorazepam were assigned to the experimental, propylene glycol-containing group. Patients receiving midazolam were assigned to the control, propylene glycol-free group. No other benzodiazepines were used.
Prior to comparing means of the two groups, an F test of equal variances was performed. If the variances were determined to be equal, a two-sample independent-group t test was performed with significance defined as p < 0.05. If the variances were determined to be unequal, a Wilcoxon rank-sum test was performed instead. [chi square] analysis was performed to compare two independent proportions, again defining significance as p < 0.05.
We defined metabolic evidence of propylene glycol toxicity if the patient had an increase in anion gap or a decrease in serum bicarbonate that reversed after discontinuation of the IV benzodiazepine and that could not be explained by an alternative etiology. An elevated osmolar gap that could not be explained by a preadmission ingestion or infusion of other medications was also considered sufficient to define the patient as having metabolic evidence of propylene glycol toxicity. If a subject had metabolic evidence of propylene glycol toxicity and shock, acidemia, or organ system failure, the subject was defined as having clinical deterioration due to propylene glycol toxicity or severe propylene glycol toxicity. The study protocol was reviewed and approved by the Institutional Review Board of Boston Medical Center.
RESULTS
Five Cases of Propylene Glycol Toxicity
Five additional cases of propylene glycol toxicity were identified in our MICU over a 2-year period. During this period, there were approximately 1,460 hospital admissions. Each case was confirmed by interviewing the attending physician, examining the written medical record, and reviewing the computer database. We estimate that 30% of our patients (438 patients) received IV benzodiazepines during their MICU stay.
Case 1: A 48-year-old man with a history of alcohol abuse was admitted for respiratory failure due to aspiration pneumonia. He was intubated and rapidly progressed to ARDS. Continuous infusion of lorazepam was administered for sedation during mechanical ventilation and for control of alcohol withdrawal. During the initial 7 days of hospitalization, the patient received 1,070 mg of lorazepam (ie, 444 g of propylene glycol). During hospital days 6 and 7, the anion gap increased to 19, serum bicarbonate decreased to 13 mmol/L, pH decreased to 7.16, and creatinine increased to 2.2 mg/dL. All values were initially normal. Sepsis was initially considered as the cause of these abnormalities; however, despite antibiotics, the anion gap increased to 22, serum bicarbonate fell to 10 mmol/L, and pH decreased to 7.11. M1 culture results were negative, and serum osmolality was 405 mOsm/kg. The lorazepam was discontinued, and midazolam was substituted. All other infusions were unchanged. Within 24 h, all metabolic abnormalities resolved. A propylene glycol level was 144 mg/dL.
Case 2: A 61-year-old man with a history of alcohol abuse was admitted in status epilepticus. He was intubated, and his seizures were controlled with IV diazepam and phenytoin. Signs of alcohol withdrawal subsequently developed, including agitation, fever, tachycardia, hypertension, and tremulousness, and the patient was maintained on IV diazepam. Over the initial 5 days, he received 4,850 mg of diazepam (ie, 970 g of propylene glycol). On the sixth hospital day, the anion gap increased to 21, serum bicarbonate decreased to 15 mmol/L, and pH decreased to 7.17. Creatinine remained unchanged. Serum osmolality was 386 mOsm/kg. Phenytoin was continued, and diazepam was changed to midazolam. Within 24 h, the metabolic abnormalities resolved. A propylene glycol level was 108 mg/dL.
Case 3: A 41-year-old man with HIV was admitted with fever and cough due to Pneumocystis carinii pneumonia. He was treated with trimethoprim/sulfamethoxazole and prednisone; despite therapy, he progressed to ARDS. Continuous infusion of lorazepam was administered for sedation during mechanical ventilation. On the twenty-third day of IV lorazepam infusion, the anion gap increased from 10 to 19, creatinine increased from 0.8 to 1.4 mg/dL, and the patient became profoundly hypotensive, requiring two vasopressors. During the next 2 days, the anion gap increased to 24, serum bicarbonate fell from 27 to 21 mmol/L, and creatinine increased to 1.9 mg/dL. Sepsis was considered; however, all cultures results were negative and the patient failed to respond to broad-spectrum antibiotics. Serum lactate was 11 mEq/dL, and serum osmolality was 380 mOsm/kg. The patient had received 11 g of IV lorazepam (ie, 4,565 g of propylene glycol) over the previous 25 days. Lorazepam was discontinued, and midazolam was substituted. All other infusions were unchanged. Within 24 h, the vasopressors were discontinued, the anion gap decreased to 18, serum bicarbonate increased to 28 mmol/L, serum creatinine decreased to 1.0 mg/dL, and serum osmolality fell to 326 mOsm/kg. A propylene glycol level was not measured.
Case 4: A 30-year-old woman with a history of IV drug abuse was admitted with infectious endocarditis due to methicillin-sensitive Staphylococcus aureus. She was treated with nafcillin and gentamicin and improved over the initial 5 days of her hospitalization. On the sixth hospital day, the midazolam infusion used for sedation during mechanical ventilation was changed to a lorazepam infusion. Over the following 3 days, she received 1,540 mg of lorazepam (ie, 639 g of propylene glycol) with simultaneous increase in the anion gap from 10 to 18 and progressive oliguric acute renal failure (creatinine increased from 0.7 to 4.6 mg/dL). The abnormalities were initially attributed to gentamicin toxicity. All blood culture results were negative. Despite initiation of hemodialysis and broad-spectrum antibiotics, the anion gap increased to 27 and the creatinine increased to 5.6 mg/dL over the next 6 days. Serum osmolality was 384 mOsm/kg, and the lactate level was 3.8 mEq/dL. The patient had received 3,068 mg of lorazepam (ie, 1,273 g of propylene glycol) during this period. The lorazepam was discontinued, and all other infusions were continued. Within 24 h, the anion gap had corrected to 12, serum osmolality decreased to 299 mOsm/kg, and creatinine decreased to 3.3 mg/dL. A propylene glycol level was not measured.
Case 5: A 53-year-old man was admitted with diffuse interstitial reticular nodular pulmonary infiltrates and a 3-week history of cough, fever, and sweats. Respiratory failure rapidly developed, and the patient was placed on mechanical ventilation, broad-spectrum antibiotics, and systemic glucocorticoids. Initially sedated with propofol and midazolam, sedation was changed to lorazepam on the fifth hospital day. From the fifth through the twelfth hospital days, the patient received 2,166 mg of lorazepam (ie, 899 g of propylene glycol). During this time, the serum bicarbonate fell from 22 to 14 mmol/L and creatinine increased from 0.6 to 3.2 mg/dL with a progressive decrease in urine output. Sepsis was considered; however, all culture results were negative and the patient failed to respond to broad-spectrum antibiotics. Serum osmolality was 408 mOsm/kg. Lorazepam was discontinued, and midazolam was substituted. All other infusions were continued. Within 72 h, the serum bicarbonate, serum creatinine, and urine output normalized. A propylene glycol level was not measured.
Observational Study
During the study period, 290 patients were admitted to the MICU and 44 patients were enrolled. Twenty-one patients were included in the propylene glycol-containing group; the propylene glycol-free group included 23 patients.
Patients who received propylene glycol-containing preparations were more likely to have a history of heavy ethanol intake (Table 1). There was no difference in age, gender, or admitting diagnosis. Electrolytes, glucose, renal function, acid-base status, nutritional status, and toxicology results were similar in both groups. There were no differences in underlying comorbid conditions (data not shown).
Many of the patients admitted to the MICU received sedatives other than benzodiazepines, most commonly propofol or fentanyl. These medications were chosen if rapid arousal or coexisting painful conditions were considered paramount. Sedative selection was at the discretion of the attending physician.
Among the 21 patients who received propylene glycol-containing benzodiazepine preparations, 4 patients (19%) had metabolic evidence of propylene glycol toxicity. All four patients had either an unexplained elevation in anion gap or an unexplained decrease in serum bicarbonate that resolved after cessation or substitution of the propylene glycol-containing benzodiazepine; one patient had both. Three of the patients had serum osmolality levels measured, and all were elevated. Only one subject had serum lactic acid measured, and it was elevated. Two subjects had propylene glycol levels measured. One subject had a serum propylene glycol level of 175 mg/dL and a urine propylene glycol level of 1,445 mg/dL; the other subject had a serum propylene glycol level of 58 mg/dL. Clinical deterioration was not observed among any subject with propylene glycol toxicity (Table 2). All of the subjects survived their MICU admission and were discharged to a medical ward in stable condition. None of the subjects who received propylene glycol-free benzodiazepine preparations had similar metabolic changes. Brief synopses of the cases of propylene glycol toxicity identified during the observational study are summarized below and in Table 3.
Case 1: A 34-year-old man with a history of alcohol abuse was admitted following a seizure. Results of a toxicology screen, including alcohol, were negative. Over the initial 2 days, he received 20 mg of diazepam by IV boluses and 730 mg of lorazepam by continuous infusion (ie, 306 g of propylene glycol). On the third hospital day, it was noted that his serum bicarbonate had progressively decreased from 26 to 15 mmol/L. Creatinine was normal. Serum osmolality was 336 mOsm/kg, serum propylene glycol was 175 mg/dL, and urine propylene glycol was 1,445 mg/dL. Both the diazepam and lorazepam were changed to midazolam. Within 24 h, the metabolic abnormalities resolved.
Case 2: A 60-year-old woman with a history of alcohol abuse was admitted following a seizure. Results of a toxicology screen, including alcohol, were negative. Over the initial 3 days, she received 290 mg of diazepam by IV boluses and 1,092 mg of lorazepam by continuous infusion (ie, 511 g of propylene glycol). On the fourth hospital day, her serum bicarbonate had decreased from 27 to 21 mmol/L. Creatinine was normal. Serum osmolality was 318 mOsm/kg (osmolar gap, 41 mOsm/kg), serum lactate was 2.3 mEq/dL, and the propylene glycol was 588 mg/dL. Both the diazepam and lorazepam were changed to midazolam. Within 48 h, the metabolic abnormalities resolved.
Case 3: A 35-year-old woman with a history of alcohol abuse was admitted with aspiration pneumonitis and a heroin overdose. During her first two hospital days, she received 68 mg of lorazepam by continuous infusion (it, 28 g of propylene glycol). On the third hospital day, her anion gap had increased from 7 to 13. The lorazepam was changed to midazolam. Within 24 h, the metabolic abnormalities resolved.
Case 4: A 35-year-old man with a history of alcohol abuse was admitted with supraventricular tachycardia. During his first hospital day, signs of alcohol withdrawal developed, including tremulousness, tachycardia, and flushing. The patient was managed with diazepam by IV boluses; over the initial 2 days, he received 2,450 mg of diazepam (ie, 490 g of propylene glycol). On the third hospital day, the serum bicarbonate had progressively decreased from 25 to 21 mmol/L and the anion gap had increased from 8 to 12. Serum osmolality was 326 mOsm/kg (osmolar gap, 35 mOsm/kg). The diazepam was changed to midazolam. Within 24 h, the metabolic abnormalities resolved.
DISCUSSION
Propylene glycol toxicity is a potentially life-threatening iatrogenic condition that is both avoidable and treatable. Therefore, a better understanding of the incidence, prevalence, clinical signs, and predisposing factors may help prevent iatrogenic morbidity and mortality. To our knowledge, the current study is the largest case series and first prospective analysis of the incidence of propylene glycol toxicity in MICU patients administered IV benzodiazepines.
In the MICU, benzodiazepines are commonly administered IV to sedate patients receiving mechanical ventilation. Clinical guidelines (22) suggest that lorazepam is the benzodiazepine of choice for continuous sedation.
While many sedatives exist, benzodiazepines are frequently chosen because of their reputation for safety and their anxiolytic and antiemetic effects. Moreover, because benzodiazepines are the preferred medication to treat or prevent alcohol withdrawal, (23) they are frequently chosen for continuous sedation when alcohol abuse is known or suspected.
Studies highlight a growing interest in propylene glycol toxicity. Yaucher and coworkers (20) reported a retrospective evaluation of eight ICU patients who had elevated serum creatinine levels while receiving lorazepam infusions. They found a positive correlation between creatinine levels and propylene glycol levels, lorazepam dose, and duration of lorazepam infusion. Yahwak and colleagues (21) prospectively evaluated 14 ICU patients receiving high-dose lorazepam and found a positive correlation between the osmolar gap and propylene glycol concentration. More recently, Arroliga and coworkers (24) prospectively evaluated nine ICU patients receiving high-dose IV lorazepam. They reported propylene glycol accumulation in six of nine patients, defined as coexistence of both an increased anion gap ([greater than or equal to] 15) and an osmolar gap ([greater than or equal to] 10 mOsm/L) in the presence of a positive propylene glycol level. Notably, they detected a positive correlation between infusion rate and propylene glycol concentration and found that the osmolar gap was the strongest predictor of propylene glycol concentration. (24) None of these studies addressed the clinical significance of the laboratory findings.
We hypothesized that the incidence of propylene glycol toxicity would be insignificant, defined as < 5%. Our belief was based on the frequency with which we had identified clinical deterioration due to propylene glycol toxicity in our MICU. Instead, we found that 4 of 21 subjects (19%) who had received propylene glycol-containing benzodiazepines had metabolic evidence of propylene glycol toxicity. The high incidence of metabolic abnormalities due to propylene glycol is consistent with the findings of Arroliga and colleagues (24): six of nine patients who received high-dose IV lorazepam had similar metabolic abnormalities consistent with propylene glycol toxicity. The data suggest that propylene glycol toxicity has a spectrum of severity ranging from common metabolic abnormalities to infrequent clinical deterioration.
A normal or acceptable level of propylene glycol has not been defined. Therefore, the clinical implication of propylene glycol levels is unclear. Although studies suggest that serum propylene glycol concentration positively correlates with the duration (20) or rate (21) of lorazepam infusion and that the osmolar gap is a reasonable surrogate for propylene glycol accumulation, (21,24) the threshold level beyond which propylene glycol accumulation is detrimental is unknown. In subjects with clinical deterioration due to propylene glycol toxicity, we found propylene glycol levels ranging from 104 to 144 mg/dL. In contrast, in subjects with only metabolic abnormalities due to propylene glycol toxicity, we found serum propylene glycol levels ranging from 58 to 127 mg/dL. This suggests that higher concentrations of propylene glycol are more likely to be associated with clinical deterioration, although overlap exists.
We sought parameters that predict susceptibility to propylene glycol toxicity. Although it is of interest that six of the nine cases of propylene glycol toxicity occurred in subjects with a history of alcohol abuse, this association could not be confirmed statistically because individuals with a history of ethanol abuse were more likely to receive propylene glycol-containing benzodiazepines in our study. It is plausible, however, that individuals with a history of ethanol abuse are more susceptible to propylene glycol toxicity since both ethanol and propylene glycol are metabolized by similar mechanisms. We hypothesize that long-standing ethanol abuse alters the usual metabolic pathways leading to the accumulation of serum osmoles and favors lactic acid production causing an anion gap and metabolic acidosis. Additional investigation is necessary to define the relationship between alcohol abuse and the risk of propylene glycol toxicity.
The mechanism of propylene glycol toxicity is unknown. Approximately 55 to 75% of propylene glycol is metabolized to pyruvate, acetate, and lactate, (3,25,26) while 25 to 45% remains unchanged. There is no evidence that the metabolic byproducts are causative. Rather, in vitro studies (27) suggest that propylene glycol itself is cytotoxic. Accumulation of lactic acid is the reason that propylene glycol toxicity commonly presents with an anion gap metabolic acidosis. If the correct diagnosis is not made, the patient can progress to hypotension, acidemia, and multisystem organ dysfunction. It can be difficult to distinguish propylene glycol toxicity from sepsis and systemic inflammatory response syndrome. Measurement of serum osmolality and/or a propylene glycol level can help distinguish the two entities; however, the diagnosis must first be considered.
The doses chosen as enrollment criteria for subjects receiving intermittent boluses of IV benzodiazepines were selected randomly. Surprisingly, one of the subjects had metabolic evidence of propylene glycol toxicity after receiving only 68 mg of IV lorazepam by continuous infusion. This raises the possibility that additional cases may have been missed because they were not enrolled in the study, as the cumulative dose they received was less than that chosen as entry criteria.
Propylene glycol is considered safe for use as a vehicle provided that dosage guidelines are not surpassed. Present guidelines suggest that IV lorazepam be used at 0.01 to 0.1 mg/kg/h, (22,24) and IV diazepam be administered at 5 to 10 mg every 3 to 4 h as needed. (28) Our calculations indicate, then, that propylene glycol should be safe for use up to nearly 1 g/kg/d. Most of our research subjects received doses of propylene glycol in excess of these guidelines. This is explained by the common belief that the lone risk of high-dose benzodiazepines is respiratory suppression and, if the patient is intubated, then little risk exists. Our study shows that propylene glycol toxicity is an additional risk that should be considered.
Clinical deterioration was not seen in the patients with propylene glycol toxicity in our prospective study. There are two possible explanations for this. It is possible that only a small subset of patients who have metabolic abnormalities from propylene glycol will progress to clinical deterioration; and a greater number of subjects are, therefore, necessary to detect clinical deterioration. Alternatively, the explanation could be institutional bias. The case that prompted the initiation of this study was widely discussed at conferences attended by the attending physicians, pulmonary/critical care fellows, and housestaff responsible for directing clinical care in our MICU. As such, metabolic abnormalities consistent with propylene glycol toxicity were more readily sought, detected, and corrected prior to the development of severe clinical deterioration in these patients. Thus, morbidity and mortality associated with propylene glycol toxicity in a MICU setting may be markedly underestimated by this study.
We acknowledge that limits in our study design exist. It would be ideal, for example, to measure serum osmolality, lactic acid, and propylene glycol levels serially in both our control and experimental groups. However, the purpose of this study was to determine whether propylene glycol toxicity is sufficiently common to warrant more rigorous clinical investigation. We believe further study is worthwhile and suggest that efforts focus on investigation of dose response, risk factors, and diagnostic markers.
This study demonstrates that metabolic abnormalities due to propylene glycol occur during routine MICU care. Moreover, propylene glycol toxicity is an iatrogenic complication that can be life threatening. From our observations, we believe that many episodes of hypotension and metabolic acidosis observed in MICU patients and attributed to a systemic inflammatory response or culture-negative sepsis are due to unrecognized propylene glycol toxicity. Propylene glycol toxicity should be considered whenever a patient has an unexplained anion gap, metabolic acidosis, hyperosmolality, and/or clinical deterioration. Close monitoring of all patients receiving IV benzodiazepines for early evidence of propylene glycol toxicity is warranted.
ACKNOWLEDGMENT: We thank John Marshall, PharmD, for assistance with the calculation of propylene glycol amounts.
REFERENCES
(1) Cate JC, Hedrick R. Propylene glycol intoxication and lactic acidosis [letter]. N Engl J Med 1980; 303:1237
(2) Food and Drug Administration. GRAS status of propylene glycol and propylene glycol monostearate. Fed Regist 1982; 47:27810
(3) Fligner CL, Jack R, Twiggs GA, et al. Hyperosmolality induced by propylene glycol: a complication of silver sulfadiazine therapy. JAMA 1985; 253:1606-1609
(4) Bekeris L, Baker C, Fenton J, et al. Propylene glycol as a cause of elevated serum osmolality. Am J Clin Path 1979; 72:633-636
(5) Commens CA. Topical propylene glycol and hyperosmolality. Br J Dermatol 1990; 122:77-80
(6) Demey HE, Daelemans RA, Verpooten GA, et al. Propylene glycol-induced side effects during intravenous nitroglycerine therapy. Intensive Care Med 1988; 14:221-226
(7) Bedichek E, Kirschbaum B. A case of propylene glycol toxic reaction associated with etomidate infusion. Arch Intern Med 1991; 151:2297-2298
(8) Huggon I, James I, Macrae D. Hyperosmolality related to propylene glycol in an infant treated with enoximone infusion. BMJ 1990; 301:19-20
(9) Arulanantham K, Genel M. Central nervous system toxicity associated with ingestion of propylene glycol. J Pediatr 1978; 93:515-516
(10) Martin G, Finberg L. Propylene glycol: a potentially toxic vehicle in liquid dosing form. J Pediatr 1970; 77:877-878
(11) Tozer TN, Winter ME. Phenytoin. In: Evans WE, Schentag JJ, Jusko WJ, eds. Applied pharmacokinetics: principles of therapeutic drug monitoring. San Francisco, CA: Applied Therapeutics, 1980; 294
(12) Wilson KC, Reardon C, Father HW. Propylene glycol toxicity [letter]. N Engl J Med 2000; 343:815
(13) Parker MG, Fraser GL, Watson DM, et al. Removal of propylene glycol and correction of increased osmolar gap by hemodialysis in a patient on high dose lorazepam infusion therapy. Intensive Care Med 2002; 28:81-84
(14) Doenicke A, Roizen MF, Hoernecke R, et al. Hemolysis after etomidate: comparison of propylene glycol and lipid formulations. Br J Anaesth 1997; 79:386-388
(15) Lolin Y, Francis DA, Flanagan RJ, et al. Cerebral depression due to propylene glycol in a patient with chronic epilepsy: the value of the plasma osmolal gap in diagnosis. Postgrad Med J 1988; 64:610-613
(16) Tuohy KA, Nicholson WJ, Schiffman F. Agitation by sedation. Lancet 2003; 361:308
(17) Cawley M. Short-term lorazepam infusion and concern for propylene glycol toxicity: case report and review. Pharmacotherapy 2001; 21:1140-1144
(18) Arbour R, Esparis B. Osmolar gap metabolic acidosis in a 60-year-old man treated for hypoxemic respiratory failure. Chest 2000; 118:545-546
(19) Al-Khafaji AH, Dewhirst WE, Manning HL. Propylene glycol toxicity associated with lorazepam infusion in a patient receiving continuous veno-venous hemofiltration with dialysis. Anesth Analg 2002; 94:1583-1585
(20) Yaucher NE, Fish JT, Smith HW, et al. Propylene glycol-associated renal toxicity from lorazepam infusion. Pharmacotherapy 2003; 23:1094-1099
(21) Yahwak JA, Biker RR, Fraser GL, et al. An observational pilot study of osmolar gap monitoring to detect propylene glycol toxicity in adult ICU patients receiving high-dose lorazepam [abstract]. Chest 2003; 124(Suppl):178S
(22) Jacobi J, Fraser GL, Coursin DB, et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med 2002; 30:119-141
(23) Mayo-Smith MF. Pharmacological management of alcohol withdrawal: a meta-analysis and evidence-based practice guideline; American Society of Addiction Medicine Working Group on Pharmacological Management of Alcohol Withdrawal. JAMA 1997; 278:144-151
(24) Arroliga AC, Shehab N, McCarthy K, et al. Relationship of continuous infusion lorazepam to serum propylene glycol concentration in critically ill adults. Crit Care Med. 2004; 32:1709-1714
(25) Christopher MM, Eckfeldt JH, Eaton JW. Propylene glycol ingestion causes D-Lactic Acidosis. Lab Invest 1990; 62:114-118
(26) Ruddick JA. Toxicology, metabolism, and biochemistry of 1,2-propanediol. Toxicol Appl Pharmacol 1972; 21:102-111
(27) Morshed KM, Jain SK, McMartin KE. Propylene glycol-mediated cell injury in a primary culture of human proximal tubule cells. Toxicol Sci 1998; 46:410-417
(28) Valium injection (package insert). Nutley, NJ: Roche Pharmaceutical, March 1999
* From The Pulmonary Center, Boston University School of Medicine, Boston MA.
Manuscript received July 12, 2004; revision accepted March 16, 2005.
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal.org/misc/reprints.shtml).
Correspondence to: Kevin Wilson, MD, The Pulmonary Center, R-304, Boston University School of Medicine, 715 Albany St, Boston, MA 02118; e-mail: kwilson@lung.bumc.bu.edu
COPYRIGHT 2005 American College of Chest Physicians
COPYRIGHT 2005 Gale Group