Economic analysis of the revised strategy to control lymphatic filariasis with mass annual single dose diethylcarbamazine (DEC) at 6 mg/kg body weight launched in one of the districts of Tamil Nadu in 1996 was carried out. This exploratory study, proposed for five years in 13 districts under 7 states on a pilot scale through the Department of Public Health is an additional input of the existing National Filaria Control Programme in India. A retrospective costing exercise was undertaken systematically from the provider's perspective following the completion of the first round of drug distribution. The major activities and cost components were identified and itemized cost menu was prepared to estimate the direct (financial) and indirect (opportunity) cost related to the implementation of the Programme. The total financial cost of this Programme to cover 22.7 lakh population in the district was Rs. 22.05 lakhs. The opportunity cost of labour and capital investment was calculated to be Rs. 7.98 lakhs. The total per capita cost was Rs.1.32, with Rs. 0.97 and Rs. 0.35 as financial and opportunity cost respectively. Based on these estimates, the implementation cost of the Programme at Primary Health Centre (PHC) level was calculated and projected for five years. The additional financial cost for the existing health care system is estimated to be Rs.27,800 per PHC every year. DEC tablets (50 mg) was the major cost component and sensitivity analysis showed that the cost of the Programme could be minimized by 20 per cent by switching over to 100 mg tablets. The analysis indicates that this Programme is a low-cost option and the results are discussed in view of its operational feasibility and epidemiological impact.
Key words Costing - financial and opportunity costs - lymphatic filariasis - mass annual single dose DEC - PHC
It is essential to consider both operational and economic feasibility of any intervention to control parasitic diseases apart from its effectiveness so as to make decisions more rationally. Health care sector in developing countries is constrained by limited resources and it is difficult to implement all possible worthwhile interventions. Still, considerable resources are allocated towards prevention and control of diseases in many developing countries in view of their significant contribution to disease burden'. Economic evaluation techniques to assess health care interventions have been standardized in recent years and are used to identify cost-effective options to control parasitic diseases2-4. However, their application in lymphatic filariasis is limited and consequently information on the costs of control strategies under operational settings are scanty5-7.
Lymphatic filariasis is considered as the second leading cause of permanent and long-term disability world-wide. India alone contributes about 40 per cent of the global disease burden due to filariasisy9,10' and the National Filaria Control Programme (NFCP) initiated in 1955, covers only 46 million people essentially in urban areas". Antilarval measures and case detection cum treatment of microfilaria carriers are the two methods adopted to control filariasis in these areas. A revised strategy using mass annual single dose diethylcarbamazine DEC) distribution'2 had been launched on a pilot scale by the NFCP in 1996 -as National Filariasis Day (NFD) programme. As an exploratory approach, the operational feasibility of this Programme through the existing health care system is being assessed in 13 identified districts in 7 states following its implementation. However, the extension of this Programme requires information on not only operational feasibility but also its cost and effectiveness. In an effort to provide information on cost-effectiveness, we determined the cost of the Programme by examining retrospectively the financial and opportunity costs from Cuddalore district in Tamil Nadu following the completion of the first round of drug distribution. Cost projections were also made for the implementation of the Programme at Primary Health Centre (PHC) level. The results of sensitivity analysis were used to provide guidelines for cost saving in programme implementation. `
Material & Methods
Mass annual single dose DEC distribution; integrated with the existing primary health care system was initiated in 1996 in selected endemic districts. The National Institute of Communicable Diseases (NICD), Delhi and National Malaria Eradication Programme (NMEP) are the nodal agencies responsible for procurement of drugs and developing strategy for information, education and communication (IEC) including arrangements of necessary funds for the same. The Directorate of Public Health and Preventive Medicine, Government of Tamil Nadu and Vector Control Research Centre, Pondicherry are the state level nodal agencies of the programme in Tamil Nadu. The Deputy Director of Health Services is looking after the Programme at the district level. Medical Officers of the PHCs through their public health staff are involved in actual implementation of NFD programme. A committee of independent experts has been identified for monitoring and evaluation of the programme. Planning, preparation and implementation are the different phases of .this programme. The key activities encompassed by this intervention included planning, sensitization, family enumeration, drug distribution and supervision. An age related dosage schedule is followed with 50mg for age class 1-2 yr, 100 mg for 2+ to 4, 150 mg for 4+ to 8, 200 mg for 8+ to 11, 250 mg for 11+ to 14 and 300 mg for more than 14 yr of age. Pregnant women, infants and chronically sick individuals are exempted.
Study area : Among the 13 districts selected, this pilot programme could be launched only in Cuddalore district in Tamil Nadu during the first year. All data related to costing were from Cuddalore district following the first round of drug distribution which was carried out between August 4-7, 1996. The population of this district is 22,69,477 (as per family enumeration prior to drug distribution). Male to female ratio is 1:0.98. Only about half of the. population had formal education. The total surface area is about 4,283 kM2 with a population density of 530/kml. About 5.3 lakhs population is living in urban areas, which include five municipalities and 16 town panchayats. There are 1,518 villages governed by 13 administrative blocks with a rural population of 17.4 lakhs. Health care facilities are extended to the 'urban and semi-urban population through 27 Government Hospitals and 16 dispensaries. A network of 51 PHCs with 319 Health Subcentres (HSCs) is pro viding health care to the rural population. Delimitation surveys conducted during 1955-59 under the NFCP had shown that the prevalence of microfilaraemia ranged from 3.0 to 15.7 per cent in different localities of this district (erstwhile Southarcot district) 13. It was relatively higher in urban areas (12.9 %) than in rural areas (5.4%). The overall microfilaria (mf) and disease rates were 8.38 and 2.62 per cent respectively". Subsequent surveys during 1988-89 (NFCP unpublished data) showed the persistence of filariasis with mf prevalence ranging from 2.50 to 10.06 in different areas of this district.
Assessment of cost: Functional organization of the NFD programme was used as the basis for identification and distribution of cost components. The present costing exercise 15.16 considers the resource inputs from provider's perspective only. District was the level of costing as the entire district was covered under this Programme and all activities as well as resources were channeled vertically from the district headquarters. Itemized cost menu" was used to determine direct (financial) and indirect (opportunity) costs. Identification of component items, recognition of the units of each item and derivation of a cost profile in relation to various input and activity categories were the main approaches followed. Actual cost incurred under different inputs of the Programme was used to determine unit cost. Actual number of vehicles used and the distance covered were used to assess the cost on transport. A unit cost of Rs. 1.95/km, including Rs.l .15 for fuel and Rs.0.80 for maintenance, was used to calculate running cost on transport.
The opportunity cost of the diverted services of personnel was calculated using official wage rates. The time allocated by different personnel for programme implementation was used to assess the total cost on labour. Vehicle was the only capital item used for this programme, the economic cost of which was calculated by annualization factor18 using current market rate. Annual economic cost of the vehicle was converted into cost per kilometer run, considering the life span of the vehicle in terms of fixed target distance to cover (2 lakhs km).
Evaluation of mass DEC programme is being carried out in this district both for its process and impact. Process indicators such as coverage, compliance, side reactions and record keeping are being monitored. Ef fectiveness indicators such as microfilaria prevalence and intensity are also monitored for impact assessment. Present analysis on impact assessment for effectiveness was restricted to data from 28 villages, 3 town panchayats and 2 municipal town's for want of parallel data from the rest of the areas.
Based on district level costing, cost at PHC level was estimated and presented in 1996 price. Estimates were made by assuming a population of 25,000 covered by 5 HSCs, eligible population of 97 per cent and total coverage of eligible population. The time allocation for drug distribution was assumed to be five days while for the rest of activities one day each. As all the PHC staff will be engaged in actual drug distribution only the Medical Officer will be left for supervision.
Market rate of Rs.0.20/50mg DEC tablet was used as unit cost on drug. Actual requirement of drug was calculated separately for 50 and 100 mg and combination using the general distribution pattern of different age classes from the census record with additional 10 per cent on wastage and overhead expenditure. The average distance of HSC from the PHC was assumed to be 10 km.
Sensitivity analysis was carried out for cost minimization. Drug price was the. only parameter with uncertainty in relation to the strength of the drug (50 mg/ 100 mg) and a unit cost of Rs.0.31 per 100 mg DEC tablet was used for comparison. Cost saving by switching over from 50 to 100 ing was determined by using sensitivity analysis. Cost projection for five years was also done using present value calculation on future cost for subsequent rounds of mass drug distribution at annual discount rate of 5 per cent'. The per capita cost derived from this analysis was used to estimate total cost of this Programme at the national level to cover the entire population at risk. The per capita cost reported from earlier studies was converted into present value (1996) and the cost per I per cent reduction of microfilaraemia was used as,cost-effectiveness ratio for comparison.
Results
Information on age-specific population, drug requirement and coverage achieved in rural and urban areas are given in Table I. The coverage in drug distribution (excluding infants) reported by the drug distributors ranged between 80.9 and 99.4 per cent in different PHCs with an average of 92.07 per cent. In urban areas the coverage was 92.39 per cent, ranging from 77.95 to 98.97 per cent in different towns. The coverage was relatively higher in urban areas when compared to rural areas. As many as 1,08,62,525 DEC tablets were distributed covering a population of 20,91,148 (92.14%). The proportion of population considered as not eligible (infants, pregnant women and sick persons) was 2.02 per cent:
The coverage (the percentage of people contacted) and compliance (the percentage of people who actually consumed the drug of those who were contacted) were also assessed through sample surveys using pre-tested questionnaire in 30 PHCs covering 3,936 individuals by external agencies following the second round. The proportion of people reported to have consumed DEC under direct supervision was 26.55 per cent. The estimated coverage was 90.04 per cent and compliance was 82.13 per cent. Among those who did not take the drug, about 27 per cent reported that they were not present at the time of drug distribution and 5 per cent did not receive the drug from the family members with whom the drug was left. Perceived side reactions was reported by 22.08 per cent of the respondents. On classification it was found that most of the side reactions were non-specific which included giddiness (53.59%), vomiting (10.69%) and nausea (1.40%). Side reactions, considered specific to infection were fever (14.49%) and headache (19.83%).
A series of meetings was held at the district headquarters to plan various activities of the programme. Sensitization was carried out using various IEC tools (Table II). These IEC tools were designed at the Directorate of Public Health and the materials were supplied to district headquarters. Health personnel, staff from other government sectors (Table III) and NGOs were involved in sensitization. Orientation camp for medical officers was held at district level in carrying out this awareness programme. Village health nurses in their respective areas, over five days carried out enumeration of household members in the family register. As many as 2,552 personnel from health and other departments were engaged in drug distribution. There were 1,276 teams, each with one provider and one assistant. During the first round of DEC distribution, the entire population was covered in two days and therefore the total person days required was 5,104. Students were treated in their respective schools while the rest of the population by door-to-door visits. Medical officers of the respective PHC area did the supervision. Vehicles from the Public Health Department were engaged and the total distance travelled was 47,659 km for different activities of this Programme. Process evaluation showed that all the villages and towns were covered and record keeping by the PHC staff was good in terms of proper entries of new additions of population and administration of correct dosages. This shows the commitment and competence of the health personnel in drug distribution. Cross sectional parasitological surveys, carried out in selected areas showed 0.32 per cent microfilaria prevalence during the pre control (baseline) period and 0.30 per cent after two rounds of mass drug distribution.
The total resources (financial cost) spent for the implementation of the first round of NFD Programme covering 22.05 lakhs population are summarized as itemized cost menu in Table 11. The per capita cost was Rs. 0.97. Among the resource-input categories, supplies were the major cost component, contributing to about 96 per cent of the total cost. Cost on drug (DEC 50 mg) alone was Rs. 19.62 lakhs (89%), the per capita cost on drug being Rs. 0.87. Government vehicles were used to cover a total of 47,659 km and the per capita-running cost on transport was Rs.0.04 and the cost on sensitization materials and family enumeration register was Rs.0.06.
Drug distribution was the most expensive activity of the Programme, demanding about 91 per cent of the total financial cost. The remaining cost was shared by sensitization (5.02%), enumeration (2,49%), supervision (1.06%) and planning (0.32%). Drug and transport costs were the only cost component under the functional category of drug distribution.
The opportunity cost on diverted labour and capital. input under different activities is shown in Table III, the per capita cost being Rs. 0.35. Cost on personnel was the major cost component (Rs.6.91 lakhs) accounting for about 87 per cent of the total opportunity cost. The share of capital cost on vehicle, which was estimated in relation to distance run (km), was only 13 per cent. Comparison of cost between the activities showed that drug distribution required rc relatively a higher labour force accounting for about 40 pcr cent of total opportunity cost. Planning and supervision required allocation of minimum personnel time. The total economic (financial + opportunity) cost of the Programme at district level was Rs.30.04 lakhs with a per capita cost of Rs.l .32.
Estimation of Programme cost at the PHC level with the existing infrastructure showed that the additional cost required for each round of mass drug distribution was Rs.27,824 (Table IV) to cover 24,250 individuals eligible for treatment (97%). The opportunity cost was estimated to be Rs. 16,947 (Table V). When this is extrapolated to cover the entire population of 4,280 1 lakhs at risk of filarial infection in India, it will require financial allocation of about Rs. 5,365 lakhs for the entire programme, every year. The cost on diverted labour and capital item will amount to Rs.3,267 lakhs. Estimation of present value of future cost of the Programme for subsequent rounds of drug administration for five years showed that each PHC would require an additional financial allocation of Rs. 1.7 lakhs for this Programme when 50 mg tablets are used.
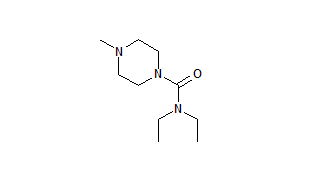
Sensitivity analysis of drug price showed that switching over from 50 mg tablet to 100 mg could reduce the cost by 20 per cent (Fig.). This will result in saving Rs. 31,400 at PHC level in financial cost for five annual rounds. of mass DEC. When combination of 50 and 100 mg is used, cost saving will be about 19 per cent.
Discussion
The burden of filarial disease in terms of disability adjusted life years (DALYs) lost in India has been estimated to be 2.8 and 1.6 lakhs for men and women respectively'. Annually about Rs. 12 crores are spent to protect 460 lakh population under the National Programme through anti-larval measures and detection-- cum-treatment of microfilaria carriers in urban areas9'''. The per capita recurring cost of this Programme is Rs.2.60 per year (estimated cost of Rs. 14.37 for five years). Analysis of costs of current mass annual single dose DEC Programme showed that the per capita cost for five annual rounds would be only Rs. 7.29. This covers the entire operation of the programme including the cost on personnel.
Analysis of the per capita cost of different intervention-strategies of a pilot study", carried out between 1966-1975 to control brugian filariasis showed that one round of selective DEC treatment was low cost option (Rs.'I 1.70) when compared to one round of weekly doses of mass DEC treatment for 12 wk (Rs. 13.34), 36 rounds of HCH residual spray (Rs.83.34), its supplementation with selective treatment (Rs. 86.47), and its supplementation with mass chemotherapy (Rs.89.03) . Another study showed that the per capita cost of DEC medicated salt programme to control bancroftian filariasis in Lakshadweep2 was Rs. 7.43 (present value). The cost to screen an individual for selective DEC treatment was reported to be Rs. 3.00 (present value)21. Cost effectiveness analysis of those interventions for which effectiveness data are available shows that the DEC medicated salt programme is more cost effective as the cost (present value) per 1 per cent reduction in microfilaraemia prevalence was the lowest (Rs. 0.09) when compared to the rest. The intervention with 36 rounds of HCH spray was the least cost-effective intervention (Rs. 1.10). However, this analysis has some limitations such as no uniformity in costing and implementation at different points of time. In view of these difficulties, the costing of the present mass single dose DEC programme has been carried out systematically. Though information on effectiveness is available after two rounds of mass treatment, it will be too early to assess the impact of the programme in terms of change in microfilaraemia prevalence. With the revised sampling design in epidemiological evaluation of the programme for impact assessment of this programme, it will be possible to carry out cost effectiveness analysis after subsequent rounds. Yet, mass annual single dose DEC distribution remains to be cheaper with a per capita economic cost of Rs. 1.32 at district level for each round, including the time cost on personnel which accounts for only 27 per cent of the total cost when compared with all other strategies.
Cost saving to an extent of 20 per cent by switching over to 100 mg tablets of DEC can be considered while planning large scale control programmes. Operationally it may be possible to use only 100 mg tablet by giving 1/2 tablet for 50 mg dosage or rounding the dosage to the nearest 100. Palatable syrup may be operationally convenient with high compliance to cover children below five years of age. Considering the cost of syrup (100 ml=Rs.12.65), the additional cost would be only 1.7 per cent of the total cost when tablets are replaced with syrup for the age class 1-4 yr. However, its operational feasibility needs to be assessed.
Estimates of both direct and, indirect costs due to filariasis are available for different communities2z. The estimated number of days lost due to acute attacks of filariasis respectively for Wuchereria bancrofti and Brugia malayi was 23.4 and 26.5 days23. Based on this, the economic loss due to lymphatic filariasis in India was estimated to be Rs.6,300 crores (US$ 1.5 billion) per year24. This can be considered as minimum as there appears to be underestimates on costs due to some uncertainties. With the estimated per capita financial cost of Rs. 1.14 at PHC level, the revised strategy would cost Rs.48.79 crores per annum to cover the entire population at risk in India. This is only less than 1 per cent of the annual economic loss due to filariasis. Though this Programme is integrated with the PHC system with no additional resources for personnel, distribution of DEC drug is an added work burden to the existing public health workers. Therefore, the ot.portunity cost of the diverted services of health personnel to distribute drug to control filariasis should not be neglected while planning large scale control operations.
The efficacy of mass single dose DEC treatment has been studied extensively9,25-28-'-x and this strategy has been recommended for the control/elimination of filariasis'-y. The present study shows that mass single dose DEC distribution is operationally feasible in terms of good coverage reflecting the commitment of the PHC staff and compliance (community acceptance as the side reactions are minimal). Thus this revised strategy differs from our earlier experience with mass single dose DEC continuously for five days during 1955-6014 which was abandoned due to poor coverage and precipitation of drug reactions provoking public resistance. Another study of mass treatment with 12 weekly doses of single dose DEC also showed a very low coverages. Therefore, with a good coverage and compliance with minimal side reactions as observed in the present study, mass annual single dose DEC can be considered operationally feasible and a low cost option for large scale control of lymphatic filariasis in India. The ongoing exploratory study on pilot scale is also expected to resolve some of the issues such as the duration of programme implementation, the level below which the transmission ceases spontaneously and the minimum coverage to be achieved. It is also essential to collect data on various resource inputs utilized for the implementation of the present pilot programme in different operational settings so as to optimize the inputs in maximizing the effectiveness in view of uncertainties in some cost components. The present economic analysis can be used as a guideline for planning and implementing the revised filariasis control strategy with mass annual single dose DEC distribution at different levels.
Acknowledgment
The authors are grateful to Dr R.T. Porkaipondian, Deputy Director of Health Services, Dr K. Senthamizhselvi, District Malaria Officer, Cuddalore district and Dr R. Meera, Filaria Officer, Filaria Control Unit for providing some details of programme implementation in Cuddalore district.
References
1. World Bank. World Development Report. Investing in health (World development indicators). New York: Oxford University Press; 1993 p. 215-23.
2. Foster S, Phillips-M. Economics and its contribution to the fight against malaria. Ann Trop Med Parasitol 1998; 92: 391-8.
3. Haddix AC, Shaffer PA. Cost effectiveness analysis. In: Haddix AC, Teutsch SM, Shaffer PA, Dunet DO, editors. Prevention effectiveness. A guide to decision analysis and economic evaluation. Oxford: Oxford University Press; 1996 p.103-29.
4. Drummond M, O'Brien B, Stoddart G, Torrance G. Methods for the economic evaluation of health care programmes. London: Oxford University Press; 1987 p. 39-167.
5. Evans DB, Gelband H, Vlassoff C. Social and economic factors and the control of lymphatic filariasis: a review. Acta Trop 1993; 53: 1-26.
6. Michael E, Meyrowitsch DW, Simonsen PE. Cost and cost effectiveness of mass diethylcarbamazine chemotherapy for the control of bancroftian filariasis: comparison of four strategies in Tanzania. Trop Med Int Health 1996; 1: 414-26.
7. Barlow R, Grober LM. Cost and benefits of controlling parasitic diseases, PHN Technical Note 85-17. Washington DC: Population, Health and Nutrition Department, The World Bank; 1985 p. 4-28.
8. World Health Organisation. The World Health Report 1996. Fighting disease fostering development. Geneva: World Health Organisation; 1996 p. 1-137.
9. World Health Organisation. Lymphatic filariasis infection and disease: Control strategies. Report of a WHO Consultative Meeting held at the Universiti Sains Malaysia, Penang, Malaysia. Document TDR/CTD/FIL/PENANG/94.1 Geneva: World Health Organisation; 1994 p. 1-30.
10. Michael E, Bundy DAP, Grenfell BT. Re-assessing the global prevalence and distribution of lymphatic filariasis. Parasitology 1996; 112: 409-28.
I 1. Sharma RS, Biswas H, Saxena NBL. National Filaria Control Programme. Operational manual. Delhi: National Malaria Eradication Programme; 1995 p.6.
12. Biswas G, Raina VK, Rao CK. A revised strategy for the control of lymphatic filariasis in India. Report and recommendations of the WHO Sponsored Workshop, Delhi: National Malaria Eradication Programme; 1996 p. I-43.
13. Basu PC, Raghavan NGS, Gaur MP Filariasis in India- facts and figures. Part X - Tamil Nadu. J Commun Dis 1971; 3: 113-25.
14. Ramakrishnan SP, Raghavan, NGS, Krishnaswamy AK, Nair CP, Basu PC, Singh D, et al. National Filaria Control Programme in India; a review. Indian J Malariol 1960; 14: 457-94.
IS. Crewe A, Parker D. Cost analysis-in primary health care. A training manual for programme managers. Geneva: World Health Organization; 1994 p. 1-147.
16. Phillips M, Mills A, Dye C. Guidelines for cost-effectiveness analysis of vector control. Panel of Experts on Environmental Management for Vector Control. PEEM Guidelines series No. 3, Geneva: World Health Organisation; 1993 p. 1-192.
17. Guyatt H, Evans D, Lengeler C, Tanner M. Controlling schistosomiasis: the cost - effectiveness of alternative delivery strategies. Health Policy Planning 1994; 9: 385-95.
18. Clemmer B, Haddix AC. Cost benefit analysis. In: Haddix AC, Teutsch SM, Shaffer PA, Dunet DO, editors. Prevention effectiveness. A guide to decision analysis and economic evaluation. Oxford: Oxford University Press; 1996 p. 85-102.
19. Rao CK, Chandrasekharan A, Kaul SM, Narasimham MVVL, Sharma SP. Relative effectiveness of different methods of control of Brugian filariasis in India. Indian J Med Res 1980; 72: 194-202.
20. Rao CK, Rao PP, Russel S, Hamzakoya KK, Chandrasekharan A, Roychowdhury SP, et aL Control of bancroftian filariasis with common salt medicated with diethylcarbamazine in Lakshadweep. Indian J Med Res 1981; 73: 865-73.
21. Sharma SP, Kosare GJ, Biswas H, Das M, Trivedi GK, Sharma GK Control of Bancroftian filariasis in rural areas through selected treatment with diethylcarbamazine. J Commun Dis 1986; 18: 283-6.
22. Ramaiah KD, Ramu K, Guyatt H, Vijar Kumar KN, Pani SP. Direct and indirect costs of the acute form of lymphatic filariasis to households in rural areas of Tamil Nadu, south India. Trop Med Inr Health 1998: 3: 108-15.
23. Sabesan S, Krishnamoorthy K, Pani SP, Panicker KN. Man days lost due to repeated acute attacks of lymphatic filariasis. Trends Life Sci 1992; 7: 5-7.
24. World Health Organization. Lymphatic filariasis: Reasons for hope. WHO/CTD/FIL/97.4 Geneva: World Health Organization; 1997 p. 1-20.
25. Kimura E, Spears GFS, Singh KI, Samarawickrema WA, Penaia L, Sone PF, et al. Long-term efficacy of single-dose mass treatment with diethylcarbamazine citrate against diurnally subperiodic Wuchereria bancrofti: eight years' experience in Samoa. Bull World Health Organ 1992; 70: 769-76.
26. Kimura E, Mataika JU. Control of lymphatic filariasis by annual single-dose diethylcarbamazine treatments. Parasitol Today 1996; 12: 240-4.
27. Addiss DG, Eberhard ML, Lammie PJ, McNeeley MB. Lee SH, McNeeley DF, et al. Comparative efficacy of clearing dose and single high dose ivermectin and diethylcarbamazine against Wuchereria bancrofti microfilaraemia. Am J Trop Med Hyg 1993; 48: 178-85.
28. Kazura J, Greenberg J, Perry R, Weil G, Day K, Alpers M. Comparison of single-dose diethylcarbamazine and ivermectin for treatment of bancroftian filariasis in Papua New Guinea. Am J Trop Med Hyg 1993: 48: 804-11..
29. Ottesen EA, Duke BOL, Karam M, Behbehani K. Strategies and tools for the control/elimination of lymphatic filariasis. Bull World Health Organ 1997; 75: 491-503.
30. Rao CK, Sen T, Roychowdhury SP, Datta KK, Das M, Krishna Rao Ch, et al. Rural filariasis control with diethylcarbamazine. J Commun Dis 1978; 10: 194-6.
K. Krishnamoorthy, K. Ramu, A. Srividya, N.C. Appavoo*, N.B.L. Saxena**, Shiv Lal** & P.K. Das
Vector Control Research Centre, Pondicherry, *Directorate of Public Health, Govt. of Tamil Nadu, Chennai &
**Directorate of National Anti Malaria Programme, Delhi
Accepted March 13, 2000
Reprint requests: The Director, Vector Control Research Centre, Indira Nagar, Pondicherry 605006
Copyright Indian Council of Medical Research Mar 2000
Provided by ProQuest Information and Learning Company. All rights Reserved