Mutant mice provide clues to how DES wreaked havoc in the womb
First, do no harm. Physicians try to adhere religiously to this creed, but sometimes the best of intentions go awry.
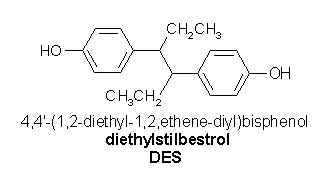
In the 1940s, physicians began giving diethylstilbestrol (DES) to pregnant women, several million of them in the United States alone. The first synthetic version of the hormone estrogen, DES was available as a pill, making it an eagerly welcomed drug for the physicians of the time who believed that insufficient amounts of estrogen led to a miscarriage. DES grew so popular that it was even prescribed for pregnant women not at high risk of a miscarriage and for treating conditions such as acne and cancer.
Although a study in 1953 concluded that DES didn't reduce the miscarriage rate, and actually seemed to increase it slightly, physicians continued to give the hormone to pregnant women until 1971. That year, another study linked several young women's development of a rare cancer of the vagina and cervix to their DES exposure while in the womb. Seven months after the study's publication, the Food and Drug Administration warned physicians not to prescribe DES to pregnant women. Subsequently, hundreds of cases of the cancer have been attributed to DES exposure.
As researchers have followed up on the side effects of the drug, they also have found that women exposed as embryos, the so-called DES daughters, may have abnormally developed reproductive tracts, causing such problems as infertility and miscarriages.
Although the evidence isn't as definitive, males exposed to DES in the womb may not have escaped the drug's wrath, either. Some research has indicated that DES sons have a higher-than-normal frequency of reproductive-tract abnormalities but no decreased fertility (SN: 5/27/95, p. 324).
Much like thalidomide, another drug that caused unexpected birth defects when given to pregnant women (see sidebar), DES has provided a sobering lesson on the importance of thoroughly testing a drug's safety. Yet, despite realizing that DES exposes the fetus to an unintended flood of estrogen, scientists have remained at a loss to explain exactly how the compound brings about its tragic effects.
In the past decade, however, developmental biologists have made great strides in identifying the genes that drive the growth of an embryo. These insights may now have solved the mystery of DES. In the November 1998 Nature Genetics, scientists present evidence from mouse studies that the synthetic hormone suppresses the activity of a gene, called Wnt-7a, that normally plays a vital role in the development of the male and female reproductive tracts.
"I think Wnt-7a is probably the primary target of DES," says coauthor David A. Sassoon of the Mount Sinai School of Medicine in New York.
While DES is no longer prescribed, DES-like drugs, such as tamoxifen, are now used to treat cancers and other illnesses. Moreover, some scientists have expressed concern about estrogenlike compounds in the environment (SN: 1/22/94, p. 56). Determining DES's modus operandi may be of more than historical interest, Sassoon argues.
Embryonic development is essentially a story of cells telling other cells where to go and what roles to take on. Cells communicate these messages by secreting proteins, and many of these signals are encoded by a large family of genes related to Wnt-7a. In vertebrates, for example, this gene family has 16 members, notes Sassoon.
To gauge each gene's embryonic role, researchers have taken to creating mice with mutations in Wnt genes. If the gene that was mutated has essential duties in development, the mouse often dies as an embryo. If it survives until birth, biologists usually can determine the mutated gene's role by looking for abnormalities.
Several years ago, Andrew P. McMahon of Harvard Medical School in Boston and his colleagues pursued this so-called gene-knockout strategy to study Wnt-7a. The mutant mice survive, but the absence of a working Wnt-7a gene during development leads to severe limb malformations, the researchers reported in 1995. The dorsal and ventral aspects of the limbs are confused. For example, hair shows up on the underside of paws.
A brief remark by McMahon's group captured the attention of Sassoon and his colleagues, who had already shown that Wnt-7a is active in the reproductive tract of embryonic and adult mice. The report "mentioned, just in passing, that the mice were sterile," says Sassoon.
Intrigued, he approached McMahon about studying the reproductive systems of Wnt-7a-knockout mice, a contact that led to the publication of papers by each group last year. In the Oct. 15, 1998 Nature, McMahon and his colleague Brian A. Parr, now at the University of Colorado at Boulder, describe how the absence of Wnt-7a alters the earliest steps in the development of a mouse's reproductive tissues.
Regardless of its sex, a mammalian embryo starts out with the rudiments of both the male and female reproductive system. The early embryo, for example, has Mullerian and Wolffian ducts. In females, the former develop into the oviduct, uterus, cervix, and vagina; in males, the latter give rise to the epididymis and vas deferens, tubes that carry sperm from the testes.
As development proceeds, the embryo establishes its sex, and either the Mullerian or Wolffian ducts regress. That's one place where Wnt-7a enters the picture. "A male produces a hormone that basically gets rid of the female system. The ability to respond to that [hormone] depends upon Wnt-7a," explains McMahon.
In male mice lacking a working copy of the gene, Mullerian ducts persist into adulthood as thin tubes paralleling the epididymis and vas deferens. Although the male reproductive system seems otherwise normal, the feminine structures block the passage of sperm in the vas deferens, causing infertility.
Both McMahon's group and Sassoon's, which described its results in the August 1998 Development, also looked at female mice lacking Wnt-7a. The researchers found that although the Wolffian ducts regress, the Mullerian ducts don't develop normally, leading to dramatic abnormalities in the female reproductive system.
The uterus, for example, doesn't develop the glands that would normally secrete substances vital to an embryo's survival. The animals' oviducts--tubes that carry eggs to the uterus--are also malformed.
"The oviducts normally look like hollow springs. They're tightly coiled," says Sassoon. In female mice lacking Wnt-7a, however, the oviducts were abnormally short and made one or no turns instead of the normal seven or eight. Either the absence of the uterine glands or the oviducts' abnormality would be sufficient to guarantee sterility.
As Sassoon and his colleagues pondered the developmental changes in the Wnt-7a-knockout mice, they looked for reports of similar abnormalities. "We kept pulling up papers describing the effects of DES, either in humans or in mice. We thought this was probably more than a coincidence," says Sassoon.
An embryo normally protects itself from its mother's estrogen by producing proteins that bind and inactivate the hormone. Unfortunately, the structure of DES differs just enough from estrogen that those protective proteins can't grasp the drug. Consequently, a pregnant woman exposed to DES blasts her developing baby with an onslaught of synthetic hormone.
Since the maturation of the female reproductive tract occurs in response to estrogen, it's not surprising that DES interferes with this process. It has long been recognized that DES can turn on or off some genes in cells that respond to estrogen. The mystery has been, what genes?
To test whether the drug works through Wnt-7a, Sassoon and his colleagues gave DES daily to mice during days 15 to 18 of pregnancy. They then compared the DES-exposed female mouse pups with unexposed pups missing Wnt-7a. The resulting reproductive-tract abnormalities in the two groups, such as malformed oviducts and missing uterine glands, closely resembled each other, says Sassoon.
The investigators next determined that uteri of newborn pups exposed to DES in the womb had unusually low Wnt-7a activity, although the gene's activity returned to normal 5 days after birth. That interference apparently lasted long enough for DES to cause major problems in the maturing female reproductive system.
"DES turns off Wnt-7a at a critical period of development," concludes Sassoon.
The investigator cautions that a temporary suppression of Wnt-7a may not be the full explanation. The Wnt-7a-knockout females have a smaller-than-normal reproductive tract, while that of DES-exposed pups is larger than normal, for example.
Then, there's the cancer issue. DES daughters have an increased risk of developing clear-cell carcinoma, a rare cancer of the vagina or cervix. Not surprisingly then, many mice that are exposed to DES while they are embryos later exhibit precancerous cells in their vaginas, as do most Wnt-7a-knockout mice.
Yet a mouse study last year found that DES granddaughters--the daughters of female mice exposed to DES as embryos--also face an increased chance of developing cancers of the genital tract even though they are free of any reproductive--tract abnormalities.
Since Sassoon believes DES does not mutate Wnt-7a but only turns it off temporarily, he's perplexed that the increased cancer risk is passed on to the next generation.
In addition to testing Wnt-7a's connection to DES, Sassoon is examining the role of other Wnt genes in the female reproductive system. He's created mice with mutations in Wnt-5a and Wnt-4, the other Wnt genes known to be active in the female reproductive tract.
Like people, mice carry two copies of each Wnt gene. In different mouse strains, Sassoon mutated one copy of each. By crossing those strains, he created mice with combinations of Wnt mutations. "They come down with disorders that look like much more' common reproductive pathologies," notes Sassoon, who hasn't yet published this research.
Some people might wonder why researchers continue to investigate the effects of DES on pregnancies long after physicians abandoned its use. One motivation, argues Sassoon, is a growing concern that estrogenlike agents in the environment may alter prenatal development.
Sassoon also notes that tamoxifen, the most widely prescribed drug to prevent breast cancer recurrence (SN: 4/11/98, p. 228), is a DES-like compound that has estrogenic activity. There is evidence that tamoxifen raises a woman's risk of developing uterine cancer (SN: 11/23/96, p. 335).
Through understanding the genes that DES affects, Sassoon believes, scientists can learn how to create a safer form of tamoxifen. "We could much more intelligently design a drug," he says.
RELATED ARTICLE: Theorizing about the dark side of thalidomide
Perhaps the only drug more infamous than DES is thalidomide, a compound that caused severe birth defects in thousands of infants when prescribed to pregnant women as a sedative and nausea medication in the late 1950s and early 1960s. Thalidomide-affected babies were born with stunted legs or arms or even with rudimentary flippers in place of hands or feet. Remarkably, as in the case of DES, scientists have yet to unravel the details of how thalidomide interferes with the growth of an embryo.
That issue has become more pressing of late, as thalidomide has gotten a new lease on life. In recent years, researchers have found that the compound may help treat conditions including leprosy, brain cancer, AIDS, and rheumatoid arthritis (SN: 12/24&31/94, p. 424).
Investigators are now seeking safer but equally potent versions of the compound. "If we can declaw an analog [of thalidomide] so that it is nontoxic to the embryos, we will truly have a wonder drug," says Trent D. Stephens of Idaho State University in Pocatello.
The best way to design a safe analog, however, would be to begin by explaining why the original is so devastating. Stephens has a new theory that may do just that.
Over the years, scientists trying to explain how thalidomide causes birth defects have put forth more than 2 dozen theories, Stephens says. His own contribution, described last year at the International Limb Development and Regeneration Conference in Sun Valley, Idaho, marries many of those theories.
Although the issue remains controversial, most researchers believe that thalidomide does not directly mutate DNA. Studies have shown, however, that the compound can transiently slip in between nucleotides, the building blocks of DNA. For unknown reasons, the drug seems to prefer to move into DNA sequences rich in guanine (G) over the other three nucleotides: adenine (A), cytosine (C), and thymine (T). Other research has shown that thalidomide can alter the activity of genes encoding proteins involved in cell-cell adhesion and others that control cell growth.
Seeking to pull those pieces of data together, Stephens and his colleague Bradley J. Filmore looked at how the genes affected by thalidomide might be regulated. Every gene has its own promoters, specialized DNA sequences that, when activated by particular proteins, help determine a gene's activity.
"We were on a fishing expedition. We were wondering if there was anything unique about these promoters," explains Stephens.
While the promoter sequences for many genes remain unknown, more than 90 percent of those documented have promoters containing either the nucleotide sequence GATA or CCAAT or both, notes Stephens. As he and Filmore studied the various genes affected by thalidomide, however, they noticed that many had unusual promoters. Instead of containing GATA or CCAAT, their promoters were rich in guanines.
"The more we followed this trail, the more amazing it seemed to us," says Stephens. Thalidomide's well-known penchant for causing only specific kinds of birth defects could stem from its specificity for this small subset of promoters, he says.
The genes scrutinized by Stephens and Filmore as possible thalidomide targets participate in a pathway of biochemical signals leading to the growth of new blood vessels, a process called angiogenesis. Thalidomide is widely known to inhibit angiogenesis in adult humans and animals: Cancer physicians use the drug because it deprives tumors of a blood supply.
In embryos, Stephens hypothesizes, thalidomide attaches to guanine-rich promoters and interferes with the activity of genes necessary for angiogenesis. As a result, he concludes, the drug "shuts off circulation to developing limbs."
"Inhibition of angiogenesis by thalidomide has never been demonstrated to occur in the embryo," counters Diether Neubert of the Free University Berlin in Germany. His team has shown that the drug alters the distribution of cell-adhesion molecules on monkey embryonic cells.
"We are not in need of more hypotheses," Neubert says. "There are already too many. We need good experimental data."
Generation of such data is easier said than done. Unlike DES, thalidomide doesn't cause birth defects in mice, making it difficult to study. Researchers must test their theories about the drug in monkeys, rabbits, or chickens.
Still, resolving this pharmaceutical mystery is vital, says Stephens. He notes that thalidomide-affected babies continue to be born in developing countries where the drug has continued to be a popular treatment for leprosy.
Moreover, the continuing confusion over the compound stymies efforts to prevent similar tragedies. "Because we don't understand the mechanism of thalidomide, we run the risk of a new thalidomide coming on the market at any time," says Stephens. --J.T.
COPYRIGHT 1999 Science Service, Inc.
COPYRIGHT 2000 Gale Group