Douglas E Moore*, Kifle A. Ghebremeskel, Bruce B. C. Chen and Elaine Y. L. Wong
ABSTRACT
The nonsteroidal anti-inflammatory drugs (NSAID), naproxen, sulindac and indomethacin, were shown to donate electrons to nitro blue tetrazolium (NBT) when irradiated with UV light in deoxygenated aqueous buffer solution (pH 7.4, 30(deg)C). The reaction was monitored spectrophotometrically by the appearance of the diformazan reduction product from NBT. The electron transfer process facilitates the decomposition of the drugs. Naproxen in the presence of NBT is photodegraded principally to the alcohol (2-[1-hydroxyethyl]-6-methoxynaphthalene) at a rate approximately 20-fold faster than when irradiated alone in deoxygenated conditions. The photoproduct from naproxen also participates in the electron transfer to NBT but at a much slower rate than naproxen. Irradiation of sulindac or indomethacin in the presence of NBT caused the slow photoreduction of NBT to diformazan. In the absence of NBT, indomethacin and sulindac are essentially unreactive when irradiated in aqueous solution. The ability of a number of NSAID to act as electron donors in their ground state was studied by observing their oxidation by potassium peroxodisulfate in pH 7.0 phosphate buffer at 50(deg)C. The HPLC analysis of the drug remaining showed that the 2-arylpropionic acid NSAID (naproxen, ibuprofen, ketoprofen and suprofen) reacted at a rate equivalent to the thermal decomposition of peroxodisulfate. The major products were the same as detected in the photooxidation of these drugs, resulting from decarboxylation and oxygen addition but also included a dimeric compound. On the other hand, the NSAID that do not contain the propionic acid substituent all reacted more slowly with peroxodisulfate, enabling specific reaction rate constants to be evaluated.
tAbbreviations: BCDS, bathocuproin disulfonic acid; Cyt, cytochrome-c; EPR, electron paramagnetic resonance; NBT, nitro blue tetrazolium; NSAID, nonsteroidal anti-inflammatory drug; SOD, superoxide dismutase.
INTRODUCTION
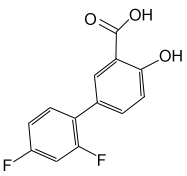
It has frequently been noted as paradoxical that a group of therapeutic agents, the nonsteroidal anti-inflammatory drugs (NSAID)^^ that are designed to alleviate inflammatory responses, are themselves a significant cause of inflammation when combined with sunlight exposure (1). The NSAID as a group are diverse in chemical structure but are consistent in their ability to inhibit the enzyme cyclooxygenase, regarded as a marker for inflammation (2). While gastrointestinal irritation is the dominant adverse side effect of their use, a significant number of these drugs are associated with photosensitivity responses in patients. Figure 1 shows the chemical structures of some of the more widely used NSAID.
A number of investigations of the photochemistry and photobiology of NSAID have shown that the most photoactive are the 2-arylpropionic acid derivatives (naproxen, ibuprofen, ketoprofen and suprofen) (3-9). The photochemistry of the 2-arylpropionic acids is dominated by an efficient photodecarboxylation process, although the specific aryl chromophore influences the nature of the primary photoprocess. For example, naproxen in neutral aqueous solution undergoes photoionization and the resulting radical readily decarboxylates to the benzylic radical from whence oxidative products are obtained in aerated solutions and reductive products in deaerated solutions (3-5). On the other hand, for ketoprofen the primary reaction under similar conditions involves an intramolecular electron transfer from the carboxyl to the carbonyl group as the pathway to decarboxylation (6,7). Ibuprofen is unusual among this group of drugs in that its absorption spectrum does not reach into the sunlight region. Nonetheless, ibuprofen is photoreactive when irradiated with UVC light, giving products analogous to those obtained with the other aryl propionic acids (8).
The generation of free radicals from the irradiation of naproxen and ketoprofen has been demonstrated by spin-trapping electron paramagnetic resonance (EPR) and the initiation of free radical polymerization of acrylamide (3,9). The radicals trapped were the decarboxylated drug and the free electron. In flash photolysis experiments with naproxen, the electron was detected in relatively high concentration (3), whereas more detailed studies on ketoprofen showed that photoionization is not a major process when the irradiation was performed at 355 nm (7). Singlet oxygen yields on irradiation of the 2-arylpropionic acids (determined by timeresolved near-IR emission) were shown to vary according to the solvent and state of ionization of the drug, with the notable exception of naproxen, which was relatively consistent (10).
While the photooxidation of susceptible biological substrates, such as membrane lipids, by singlet oxygen or free radical pathways is widely believed to lead to cell disruption and the initiation of the adverse responses (11), it is possible that, in conditions of low oxygen concentration, or when the sensitizer is located close to susceptible substrates, direct electron transfer between sensitizer and substrate may become a significant contributor. Oxygen may also be involved as an electron carrier in the form of the superoxide anion radical. The question thus arising is whether it is possible that direct electron transfer between sensitizer and substrate may become a significant contributor to the production of phototoxic responses. The spin-trapping EPR experiments provide qualitative evidence for the transfer of an electron from the sensitizer to an acceptor substrate.
Other reagents that act as electron acceptors include nitro blue tetrazolium (NBT), cytochrome-c (Cyt) and the copper (II) complex with a bifunctional ligand such as bathocuproine disulfonic acid (BCDS) (12-15). A number of photosensitizing drugs previously tested in this laboratory (3,16-18) have been shown to undergo photoionization and/or are active in free radical generation. It was found that some of these also participate in electron transfer processes. For example, 6-mercaptopurine reacts with NBT or p-nitrosodimethylaniline when irradiated in an oxygen-free solution (16), and the antibacterial drug sulfamethoxazole was also found to participate in photo-initiated electron transfer to NBT and Cyt. (17). The novel anti-inflammatory agent benzydamine was found, on UV irradiation, to be able to transfer electrons to all three reagents, NBT, Cyt and BCDS (18).
In addition to the reactivity from their photoexcited states, NSAID also participate in electron transfer processes in the ground state. Oxidative decarboxylation of substituted phenylacetic acids can be mediated by metallic and nonmetallic oxidants or by electrolytic means (19-21). Naproxen is the only NSAID studied in this type of reaction. When naproxen was treated with cerium (IV) or peroxodisulfate, the product pattern was similar to that from photolysis (22). When certain other NSAID (diflunisal, indomethacin, sulindac, piroxicam and aspirin) were added to the acrylic monomer acrylamide undergoing free radical-initiated polymerization, the rate of reaction was reduced due to direct reaction of the NSAID with the carbon-centered polyacrylamide radical (23). The reaction mechanism was postulated to involve reduction of the drug by electron transfer from the polymer radical to the drug molecule. On the other hand, the 2-arylpropionic acids, naproxen and ibuprofen, were able to compete with acrylamide for the initiating free radical from the thermal decomposition of peroxodisulfate, thereby inhibiting the overall polymerization reaction. In this process, the drug is oxidized following donation of an electron by the drug molecule to the sulfate radical anion.
In this paper we report further on electron transfer reactions involving NSAID in their ground or photoexcited states. In the first part we have extended the study of their reaction with potassium peroxodisulfate, previously reported with naproxen by Bosca et al. (22), to ketoprofen, ibuprofen and suprofen (all 2-arylpropionic acids) as well as sulindac, indomethacin, diclofenac, diflunisal and piroxicam. In the second part, electron transfer from the photoexcited state of selected NSAID to NBT was investigated. For this part, naproxen was chosen as an example of the 2-arylpropionic acids, for comparison with sulindac and indomethacin as examples of aryl acetic acid derivatives.
MATERIALS AND METHODS
Diflunisal, sulindac and indomethacin were kindly provided by Merck, Sharp and Dohme (Sydney, Australia), ibuprofen by SmithKline-Beecham (Sydney, Australia), naproxen by Syntex (Sydney, Australia) and piroxicam by Pfizer (Sydney, Australia). The HPLC analysis indicated no detectable impurities in each of these substances so they were used without further purification. Potassium peroxodisulfate (Ajax Chemicals, Sydney, Australia) was twice recrystallized from water double distilled from an all-glass apparatus. The NBT came from Sigma Chemicals (St. Louis, USA). Other chemicals used were of analytical reagent grade (BDH and Ajax Chemicals, Sydney).
Stock solutions of the drugs were prepared by dissolving the required amount of drug in 10 mL acetonitrile, then diluting with 0.05 M pH 7.0 phosphate buffer in a 25 mL volumetric flask. The use of the organic solvent rather than dilute alkali for the dissolution of these acidic drugs was adopted to circumvent the fact that indomethacin and piroxicam hydrolyze readily at alkaline pH. The selected concentration of the test drug in the reaction mixture was achieved by further dilution with phosphate buffer. Acetonitrile was selected because of the known capacity of primary alcohols (e.g. methanol or ethanol) to be oxidized by potassium peroxodisulfate (24).
Thermal reactions of NSAID with peroxodisulfate. Each reaction mixture of total volume 10 mL was prepared in a stoppered flask by the addition of the appropriate volume of preequilibrated solutions of 50 mM potassium peroxodisulfate, 2.0 mM drug and phosphate buffer (0.05 M, pH 7.0) to give the desired concentrations. The flask was placed in a thermostat at 50.0+/-0.05(deg)C and samples were withdrawn by syringe for immediate analysis of the amount of drug remaining by HPLC. The isocratic HPLC system consisted of an LKB-Bromma model 2150 pump with a Rheodyne 20 (mu)L loop injector and a Merck Lichrosphere 60 RP-18 column (5 (mu)m, 125 X 4 mm) with a Shimadzu SPD-6A variable wavelength detector. The mobile phase was acetonitrile, water and glacial acetic acid in the ratio 40:60:0.4 at a flow rate of 1.0 mL/min. For identification of the products, the HPLC system was interfaced with a Hewlett-Packard model 1040A diode-array spectrophotometric detector or a Finnigan TSQ 7000 mass spectrometer.
Electron transfer reactions photosensitized by NSAID. Buffered aqueous solutions (phosphate, 0.05 M, pH 7.4) containing NBT (5.0 x 10^sup 5^ M) with 50 (mu)M drug were flushed with gas (N^sub 2^ or O^sub 2^ as required) for 40 min before irradiating. The samples were contained in stoppered cylindrical quartz vessels of 10 mm pathlength and irradiated with a 400 W medium-pressure mercury arc (Applied Photophysics Ltd., UK) through a 2 mm Pyrex glass filter (Coming O53). The arc source, filter and reaction vessel assembly was immersed in a thermostat maintained at 30.0(deg)C. The photoreduction of NBT was followed as a function of the irradiation time by determining the increase in absorbance at 560 nm due to the diformazan product (12). Quantum yields were determined by ferrioxalate actinometry as previously described (25).
RESULTS AND DISCUSSION
Thermal electron transfer reactions of NSAID with potassium peroxodisulfate
The extent of reaction of naproxen, ibuprofen, ketoprofen, suprofen, sulindac, indomethacin, piroxicam and diclofenac with potassium peroxodisulfate at 50(deg)C was determined by HPLC assay of the reaction mixture at various times to quantify the amount of drug remaining. In the absence of potassium peroxodisulfate, there were no significant changes in the chromatograms over a period of at least 4 h. This indicates that the drugs are all thermally stable in solution at 50(deg)C under the conditions used for the subsequent studies. In the presence of peroxodisulfate, the rate of loss of drug varied according to the nature of the drug and the concentration of peroxodisulfate. To gain conveniently observable reaction rates that were independent of the peroxodisulfate concentration, relatively high concentration ratios of potassium peroxodisulfate to the drug (25-200 times) were used.
The reaction data fell into two distinct classes according to the drug involved. Plots of drug concentration versus time for the reaction of the 2-arylpropionic acids (naproxen, ketoprofen, suprofen or ibuprofen) with different concentrations of potassium peroxodisulfate were linear, indicating the kinetics of the reaction to be zero order with respect to these drugs. When the zero-order rate constant was plotted versus potassium peroxodisulfate concentration, a linear response was obtained to show the rate constant to be directly proportional to the peroxodisulfate concentration. The slopes of the plots for naproxen, ketoprofen, suprofen and ibuprofen all agreed within experimental error with the reported value (1.5 +/-0.9) X 10^sup -6^ s^sup -1^ for the rate constant of the decomposition of potassium peroxodisulfate in pH 7.0 aqueous solution at 50C (26). In other words, the rate-limiting step is the decomposition of peroxodisulfate, and each of the 2arylpropionic acid drugs is capable of reacting with the sulfate radical anion as soon as it is formed. In our earlier study of the reaction of NSAID with polyacrylamide radicals (23) naproxen and ibuprofen were shown to be able to compete with acrylamide for the sulfate radical anion that initiated the polymerization reaction. Hence the rate constant for reaction of the sulfate radical anion with naproxen or ibuprofen should be on the order of 2 X 10^sup 8^ M^sup -1^s^sup -1^, which is the value for reaction of the sulfate radical anion with acrylamide (27).
On the other hand, for sulindac, indomethacin, piroxicam and diclofenac, the plot of the logarithm of the remaining drug concentration versus time was linear, indicating the kinetics of the reaction to be first order. In this case, the reaction of the drug with the sulfate radical anion is slower than for the 2-arylpropionic acids, and competes with the solvent water (24). These rate constants were found to be on the order of 10^sup 7^ M^sup -1^ s^sup -1^ and can be compared with the estimate of at least l0^sup 8^ M^sup -1^ s^sup -1^ for the 2-arylpropionic acids (see above). All are comparable with values for the limited number of aromatic compounds reported in pulse radiolysis studies of the reaction of the sulfate radical anion (27). Values ranged from 1.7 X 10^sup 7^ M^sup -1^ s^sup -1^ for 1,2,4,5-benzenetetracarboxylate ion to 8.5 X 10^sup 9^ M^sup -1^ s^sup -1^ for 2,3-dimethoxybenzoate ion (27). However it would be desirable to verify the values determined here by a direct pulse radiolysis study of the reaction of the NSAID with the S04- radical anion. The ranking of these NSAID with respect to their ability to react with the sulfate radical anion is piroxicam > sulindac > indomethacin > diclofenac > diflunisal. It should be noted that this order is not the same as found for the reaction of the same NSAID with polyacrylamide radicals (sulindac > diflunisal > piroxicam > indomethacin). However the latter reaction involves electron uptake and reduction of the drugs, whereas in the former case, electron donation occurs to the sulfate radical anion and the NSAID are being oxidized in the process.
The oxidative decarboxylation reaction of substituted phenylacetic acids has been studied extensively using peroxodisulfate and other oxidizing agents (19-21). It is now clear that the side-chain oxidation involves a benzylic radical cation intermediate formed by electron transfer from the carboxylate group (Kolbe reaction) or the (pi)-system of the aromatic ring (pseudo-Kolbe reaction) to the sulfate radical anion. Using a series of model compounds, Tanner and Osman (21) showed that the rate of the electron transfer process was more sensitive to aromatic-ring substituents than to benzylic substituents (methyl or phenyl). The NSAID involved in the present study are more diverse in structure than the model compounds but would appear to contradict that conclusion, because the 2-arylpropionic acids (naproxen, ketoprofen, suprofen and ibuprofen) reacted significantly faster than the arylacetic acids (indomethacin, sulindac, diclofenac), which were comparable to the arylcarboxylic acid (diflunisal) and piroxicam (no carboxylic group).
The previous study by Bosca et al. (22) of the reaction of peroxodisulfate with naproxen showed that the products formed following decarboxylation were the alcohol (2-[1hydroxyethyl]-6-methoxynaphthalene), the ketone (2-acetyl6-methoxy-naphthalene) and a dimeric compound (1,1'bis[6-methoxy-2-naphthyl]-ethoxyethane). The first two are the main products obtained in the photooxidation of naproxen (3,4). Using diode-array and mass spectral detection in HPLC, we verified the formation of all three products for naproxen, and in addition, the ethyl reduction product (2ethyl-6-methoxynaphthalene) that was detected in greater yield as the reaction mixture was deaerated. Analogous products were found arising from ketoprofen and suprofen in yields of similar proportions to naproxen, while for ibuprofen, the dimeric compound was not detected.
For the other NSAID the product patterns were much more complex, and all the products have not yet been unequivocally identified. While the acetic acid group is a feature of some, there was no evidence to suggest that there is a common pathway for the reaction of these NSAID with peroxodisulfate. The product profile may be complicated by aromatic ring hydroxylation by peroxodisulfate in addition to side-chain reactions (28). There is also no analogy in photodegradation of these particular compounds to suggest a common pathway.
Photoreduction of NBT sensitized by NSAID
The capability of naproxen, sulindac and indomethacin to act as electron-transferring photosensitizers was tested using NBT as an electron acceptor in phosphate buffer solution at pH 7.4. The drug concentration used was 5 X 10^sup -5^ M for each, even though this gave substantially different levels of absorption, as shown by the UV spectra in Fig. 2. The photoreduction of NBT was observed as a function of irradiation time by determining the increase in absorbance at 560 nm due to the appearance of the formazan product. Control experiments revealed that no detectable reduction occurred when NBT in N^sub 2- or O^sup 2-flushed solutions were irradiated in the absence of sensitizer or when the sensitizer and NBT were mixed but not irradiated.
Naproxen. The time course of the reduction of NBT photosensitized by naproxen is shown in Fig. 3. The reaction occurred rapidly in N^sup 2-^saturated solution but to a lesser extent when an air-saturated solution was employed under otherwise identical conditions and was inhibited completely when the solution was flushed with OZ before and during irradiation. Thus, it appears that reduction of NBT photosensitized by naproxen can be a direct reaction from the excited state of naproxen to NBT but strongly subject to interference by molecular oxygen. From Fig. 3 it is clear that the reduction sensitized by naproxen under anaerobic conditions is biphasic, with a short rapid initial phase followed by a much slower one. The magnitude of the response depended directly on the naproxen concentration up to 10-4 M, whereafter the response plateaued. In aerated conditions the absorbance at 560 nm increased slowly but linearly with time. This behavior is similar to that observed with benzydamine (18) but different from sulfamethoxazole (17) or (alpha)terthienyl (29), where a linear relationship was observed in N^sub 2-^saturated solution, and there was no difference between air- or O^sub 2-^saturated solutions. The HPLC analysis of the reaction revealed that by the irradiation time of 5 min, 90% of the original naproxen had been degraded. The quantum yield for the initial disappearance of naproxen irradiated in the presence of NBT (both 5 x 10^sup -5^ M) was estimated to be 0.020 +/-0.004. The slowing down of the reduction of NBT is consistent with the disappearance of the sensitizer and its replacement by one of lesser capability. Under these conditions, the photodegradation product detected in about 80% yield was 2-(1-hydroxyethyl)-6-methoxynaphthalene. Analysis of a deaerated naproxen solution irradiated in the absence of NBT showed that the drug degraded much more slowly, in accord with the previously reported quantum yield of 0.001 (3). The strength of the electron-donating capability of naproxen is therefore embodied in the decarboxylation of the propionic acid group, with the photoreaction proceeding more rapidly in the presence of a suitable electron acceptor. The reaction can also be demonstrated with Cyt and the copper(II)-BCDS complex acting as the electron acceptors, as shown for sulfamethoxazole and benzydamine (17,18).
In the presence of oxygen, the process could be complicated by the formation of either or both singlet oxygen and superoxide. For enzymic and photochemical reactions under aerobic conditions, it has been widely believed that reduction of NBT to diformazan occurs by electron transfer from superoxide anion that acts as an intermediate. Thus, suppression of the reduction by the enzyme superoxide dismutase (SOD) is used frequently as a diagnostic for the participation of superoxide (30). Addition of SOD to the air-saturated reaction mixture of NBT with naproxen irradiated for 15 min showed a 70% inhibition of the formation of formazan, implying the involvement of superoxide when some oxygen was present. On the other hand, addition of SOD to the same system under deaerated conditions had no effect, an expected result because oxygen was not present. Thus, electron transfer from the naproxen triplet state to NBT can be direct or involve superoxide as an intermediate, although the direct reaction is more efficient. Similar results were also reported for photoreduction of NBT sensitized by riboflavin and methionine (30), anthracene (31), 6-mercaptopurine (16), sulfamethoxazole (17) and benzydamine (18). Because other 2arylpropionic acid NSAID (ketoprofen, suprofen and ibuprofen) have differing chromophores yielding differences in photoreactivity (7,10), it does not necessarily follow that they would react with NBT in a similar manner to naproxen.
Sulindac and indomethacin. When sulindac or indomethacin was used as photosensitizer, the reduction of NBT was much slower than for naproxen. A simple linear increase in absorbance was observed with time (Figs. 4 and 5) with a concomitant slow degradation of indomethacin or sulindac detected by HPLC analysis. The rate of the reduction reaction was maximal when the solution was irradiated under N^sub 2-^flushed conditions and less significant when O^sub 2^ was present. However, complete saturation with O^sub 2^ did not have any further effect compared to air saturation of the solutions. It can be concluded that direct electron transfer from the excited state of sulindac or indomethacin to NBT can occur in deoxygenated conditions. Because of the effect that oxygen has on the electron transfer process, it is probable that it is the triplet excited state that is involved. This is particularly evident for naproxen, which has a relatively strong capacity to generate singlet oxygen, whereas indomethacin and sulindac did not display such ability (3) (unpublished observations).
The reported incidence in Australia of phototoxic reactions involving sulindac is about 60% that of naproxen, whereas for indomethacin it is negligible (32). When tested by two in vitro assays-photohemolysis of erythrocytes and growth inhibition of Candida albicans (33)-as well as an in vivo assay-the mouse tail technique (34)-no activity was found for sulindac and indomethacin. These studies are in accord with the minimal photosensitizing activity in aqueous solution, in terms of singlet oxygen and free radical generation (3). From that study it was clear that indomethacin is relatively stable when irradiated in aqueous solution, even though irradiation in nonpolar solvents leads to decomposition by an oxygen-independent mechanism (35-37). A free radical intermediate, formed by decarboxylation of indomethacin, was detected by spin-trap EPR and a weak triplet state by flash photolysis of benzene solutions (35). The stability of the indomethacin molecule in polar solvents may be attributed to a resonance-stabilized chromophore extension through the amide link between the indene and p-chlorophenyl groups. Free rotation about this link apparently provides an efficient pathway for internal conversion or triplet state decay to occur at room temperature. The very low level of photochemical activity recorded for indomethacin despite its strong UV absorption spectrum has led to studies that show that this drug has a capacity to act as a sunscreening or photoprotective agent when applied topically (38,39).
Sulindac is yellow in color and has an extensive absorption spectrum across the UVA range (Fig. 2), yet no detailed study of its photochemistry has been reported. There is some structural analogy to indomethacin, except that the chromophore is clearly seen to extend through the molecule via the olefinic bond without the need for resonance stabilization. The process of photoisomerization about this olefinic bond was found to occur (unpublished observations), thereby dissipating the excited-state energy and accounting for the very limited photochemical activity of sulindac.
Naproxen and other 2-arylpropionic acids can act as photosensitizers of lipid peroxidation and hemolysis of erythrocytes (4,8,9,17). However, we found that neither sulindac nor indomethacin when irradiated with linoleic acid was able to raise the rate of oxidation of the unsaturated fatty acid above the level recorded in the absence of the drugs. Their lack of effect in the photohemolysis of erythrocytes has been reported (33).
CONCLUSIONS
These studies have shown that the presence of a suitable acceptor facilitates electron transfer for both the ground and excited states of the NSAID naproxen, sulindac and indomethacin, thereby promoting their degradation. In the case of naproxen, the reaction rates are relatively rapid and yield similar decarboxylated products from ground- and excitedstate reactions. The implications for biological systems are that ground-state naproxen is capable of scavenging strongly oxidizing species (a beneficial effect in, say, oxidative stress) while naproxen raised to its excited state by the absorption of sunlight becomes a more powerful reductant potentially capable of reacting with less readily oxidizable species. This latter aspect may be relevant in the photosensitizing action of naproxen. For the other 2-arylpropionic acids (ketoprofen, ibuprofen and suprofen) the ground-state reactivity with peroxodisulfate was similar to naproxen. There are known differences in the photochemistry of these molecules because of the different chromophores, so it remains to be determined whether the reactivity with NBT differs from that shown by naproxen.
For indomethacin and sulindac, as well as diclofenac, piroxicam and diflunisal, ground-state reactivity with peroxodisulfate was slow enough to enable differentiation of their reaction rates, thereby indicating their ability to scavenge highly oxidizing species. Indomethacin and sulindac also reacted slowly with NBT upon irradiation with UV light. This minor level of photoreactivity represents the only photosensitizing activity reported to date for these drugs in aqueous solution, in accord with the low incidence of adverse biological photosensitivity. On the other hand, diclofenac (40), piroxicam (41) and diflunisal (42) have significant photoreactivity both in vitro and in vivo and will be investigated for their reactivity with NBT and other electron transfer reagents.
Acknowledgements-This work was supported in part by the Australian Research Council and by scholarships provided by the Australian International Development Assistance Bureau and The University of Sydney Overseas Postgraduate Scholarship Scheme.
REFERENCES
1. Kochevar, 1. E. (1989) Phototoxicity of non-steroidal anti-inflammatory drugs: coincidence or specific mechanism? Arch. Dermatol. 125, 824-826.
2. Vane, J. R. and R. M. Botting (1995) New insights into the mode of action of anti-inflammatory drugs. Inflammation Res. 44, 1-10.
3. Moore D. E. and P. P. Chappuis (1988) A comparative study of the photochemistry of the non-steroidal anti-inflammatory drugs, naproxen, benoxaprofen and indomethacin. Photochem. Photobiol. 47, 173-181.
4. Costanzo, L. L., G. De Guidi, G. Condorelli, A. Cambria and A. Fama (1989) Molecular mechanism of naproxen photosensitization in red blood cells. J. Photochem. Photobiol B Biol. 3, 223-225.
5. Bosca, F., M. A. Miranda, L. Vano and F. Vargas (1990) New photodegradation pathways of naproxen, a phototoxic non-steroidal anti-inflammatory drug. J. Photochem. Photobiol. A Chem. 54, 131-134.
6. Bosca, F., M. A. Miranda, G. Carganico and D. Mauleon (1994) Photochemical and photobiological properties of ketoprofen associated with the benzophenone chromophore. Photochem. Photobiol. 60, 96-101.
7. Monti, S., S. Sortino, G. De Guidi and G. Marconi (1997) Photochemistry of 2-(3-benzoylphenyl)-propionic acid (ketoprofen). Part 1. A picosecond and nanosecond time resolved study in aqueous solution. J. Chem. Soc. Faraday Trans. 93, 2269-2275. 8. Castell, J. V., M. L. Gomez-L., M. A. Miranda and I. M. Morera (1987) Photolytic degradation of ibuprofen. Toxicity of the isolated photoproducts on fibroblasts and erythrocytes. Photochem. Photobiol. 46, 991-996.
9. Costanzo, L. L., G. De Guidi, G. Condorelli, A. Cambria and M. Fama (1989) Molecular mechanism of drug photosensitization-II. Photohemolysis sensitized by ketoprofen. Photochem. Photobiol. 50, 359-365.
10. De la Pena, D., C. Marti, S. Nonell, L. A. Martinez and M. A. Miranda (1997) Time-resolved near infrared studies on singlet oxygen production by the photosensitizing 2-arylpropionic acids. Photochem. Photobiol. 65, 828-832.
11. Spikes, J. D. (1989) Photosensitization. In The Science of Photobiology, 2nd ed. (Edited by K. C. Smith), pp. 79-110. Plenum Press, New York.
12. Kirby, T. W. and I. Fridovich (1982) A picomolar spectropho
tometric assay for superoxide radical. Anal. Biochem. 127, 435440,
13. Auclair, C., M. Torres and J. Hakim (1978) Superoxide anion involvement in NBT reduction catalysed by NADPH-cytochrome p-450 reductase. FEBS Lett. 89, 26-28. 14. Zak, B. (1958) Simple procedure for the single sample determination of serum copper and iron. Clin. Chem. Acta 3, 328332.
15. Costanzo, L. L., G. De Guidi, S. Guiffrida, E. Rizzarelli and G. Vecchio (1993) Determination of SOD-like activity of copper(II) complexes. J. Inorg. Biochem. 50, 273-281. 16. Hemmens, V. J. and D. E. Moore (1986) Photochemical sensitization by azathioprine and its metabolites-I. 6-mercaptopurine. Photochem. Photobiol. 43, 247-255. 17. Zhou, W. and D. E. Moore. (1997) Photosensitizing activity of the anti-bacterial drugs sulfamethoxazole and trimethoprim. J. Photochem. Photobiol. B Biol. 39, 63-72. 18. Moore, D. E. and J. Wang (1998) Electron transfer mechanisms in photosensitization by the anti-inflammatory drug benzydamine. J. Photochem. Photobiol. B. Biol. 43, 175-180. 19. Trahanovsky, W. S., J. Cramer and D. W. Brixius (1974) Oxidation of organic compounds with cerium (IV). XVIII. Oxidative decarboxylation of substituted phenylacetic acids. J. Am. Chem. Soc. 96, 1077-1081.
20. Coleman, J. P., R. Lines, J. P. Utley and B. C. L. Weedon (1974) Electro-organic reactions. Part II. Mechanism of the Kolbe electrolysis of substituted phenylacetate ions. J. Chem. Soc. Perkin Trans. II, pp. 1064-1069.
21. Tanner, D. D. and S. A. A. Osman (1987) Oxidative decarboxylation. On the mechanism of the potassium persulfate promoted decarboxylation reaction. J. Org. Chem. 52, 46894693. 22. Bosca, F., R. Martinez-Manez, M. A. Miranda, J. Primo, J. Soto and L. Vano (1992) Oxidative decarboxylation of naproxen. J. Pharm. Sci. 81, 479482.
23. Moore, D. E. and B. C. Chen (1997) Reactions of non-steroidal anti-inflammatory drugs with polyacrylamide free radicals. Redox Rep. 3, 41-47.
24. Dogliotti, L. and E. Hayon (1967) Flash photolysis of persulfate ions in aqueous solutions. Studies of the sulfate and ozonide radical anions. J. Phys. Chem. 71, 2511-2516. 25. Moore, D. E. (1987) Principles and practice of drug photode
gradation studies. J. Pharm. Biomed. Analysis 5, 441-455. 26. Behrman, E. J. and J. O. Edwards (1980) The thermal decomposition of peroxodisulphate ions. Rev. Inorg. Chem. 2, 179206.
27. Neta, P., R. E. Huie and A. B. Ross (1988) Rate constants for reactions of inorganic radicals in aqueous solution. J. Phys. Chem. Ref. Data 17, 1027-1284.
28. Walling, C., D. M. Camaioni and S. S. Kim (1978) Aromatic hydroxylation by peroxydisulfate. J. Am. Chem. Soc. 100, 48144818.
29. Kagan, J., M. Bazin and R. Santus (1989) Photosensitization with ct-terthienyl: the formation of superoxide ion in aqueous media. J. Photochem. Photobiol. B Biol. 3, 165-174. 30. Beauchamp, C. and I. Fridovich (1971) Superoxide dismutase: improved assays and an assay applicable to acrylamide gels. Anal. Biochem. 44, 276-287.
31. Joshi, P. C. and M. A. Pathak (1984) The role of active oxygen (singlet oxygen and superoxide anion radical) induced by crude coal tar and its ingredients used in photochemotherapy of skin diseases. J. Invest. Dermatol. 82, 67-73. 32. Adverse Drug Reactions Advisory Committee (1987) A sunburnt country revisited. Adverse Drug Reactions Bulletin, Australian Department of Health, Canberra.
33. Ljunggren, B. (1985) Propionic acid-derived non-steroidal antiinflammatory drugs are phototoxic in vitro. Photodermatology 2, 3-9.
34. Ljunggren, B. and K. Lundberg (1985) In vivo phototoxicity of non-steroidal anti-inflammatory drugs evaluated by the mouse tail technique. Photodermatology 2, 377-382. 35. Dabestani, R., R. H. Sik, D. G. Davies, G. Bubay and C. F. Chignell (1993) Spectroscopic studies of cutaneous photosensitizing agents. XVIII. Indomethacin. Photochem. Photobiol. 58, 367-373.
36. Pawelczyk, E. and B. Knitter (1977) Kinetics of indomethacin degradation. Pharmazie 32, 698-699.
37. Weedon, A. C. and D. F. Wong (1991) The photochemistry of indomethacin. J. Photochem. Photobiol. A Chem. 61, 27-33. 38. Lim, H. W., G. J. Thorbecke, R. L. Baer and I. Gigli (1983) Effect of indomethacin on alteration of ATPase-positive Langerhans cell density and cutaneous sunburn reaction induced by ultraviolet-B radiation. J. Invest. Dermatol. 81, 455458. 39. Schwartz, T., F. Gschnait and F. Greiter (1985) Photoprotective effect of topical indomethacin-an experimental study. Dermatologica 171, 450-458.
40. Moore, D. E., S. Roberts-Thomson, Z. Dong and C. C. Duke (1990) Photochemical studies on the anti-inflammatory drug diclofenac. Photochem. Photobiol. 52, 685690. 41. Miranda, M. A., F. Vargas and G. Serrano (1991) Photodegradation of piroxicam under aerobic conditions. The photochemical keys of the piroxicam enigma? J. Photochem. Photobiol. B Biol. 8, 199-202.
42. De Guidi, G., R. Chillemi, S. Giuffrida, G. Condorelli and M. Cambria Fama (1991) Molecular mechanism of drug photosensitization. Part 3. Photohemolysis sensitized by diflunisal. J. Photochem. Photobiol. B Biol. 10, 221-237.
School of Pharmacy, The University of Sydney, Sydney, Australia Received 28 April 1998; accepted 5 August 1998
*To whom correspondence should be addressed at: School of Pharmacy (A15), The University of Sydney, Sydney 2006, Australia. Fax: + 61 2 9351 4391; e-mail: demoore@pharm.usyd.edu.au
Copyright American Society of Photobiology Nov 1998
Provided by ProQuest Information and Learning Company. All rights Reserved