The cent of diagnosis and optimal management of cluster headache remain challenging. This most painful of primary headaches affects 0.1 per-adults. (1) The male-to-female ratio has diminished from 6.2 to 1 in the 1960s to 2.1 to 1 in the 1990s. (2) Men may first experience cluster headache in their early 20s, with peak onset in their 40s. In one study, (3) the most frequent age at onset for women was in their 60s. Cluster headache may be underdiagnosed in black women, (4) but ethnic differences in prevalence have not been studied. Having a family history of headaches, smoking, head injury, or shift work has been associated with cluster headache.
Clinical Features and Classification
In 2004, the International Headache Society published new criteria for diagnosing cluster headache. To fulfill criteria for diagnosis, patients must have had at least five attacks occurring from one every other day to eight per day; and attributable to no other disorder. (5) In addition, headaches must cause severe or very severe unilateral orbital, supraorbital, or temporal pain lasting 15 to 180 minutes if untreated, and be accompanied by one or more of the following: ipsilateral conjunctival injection or lacrimation, ipsilateral nasal congestion or rhinorrhea, ipsilateral eyelid edema, ipsilateral forehead and facial sweating, ipsilateral miosis or ptosis, or a sense of restlessness or agitation. (5) Episodic cluster headache is defined as at least two cluster periods lasting seven to 365 days and separated by pain-free remission periods of one month or longer. Chronic attacks recur over more than one year without remission or with remission lasting less than one month. (5)
Called "suicide headache" because of its severity and "alarm clock" headache because of its periodicity, cluster headache is characterized by unilateral excruciating pain (a hot-poker or stabbing sensation) in the ocular, frontal, or temporal areas. Pain often radiates to the upper teeth, jaw, and neck. Associated signs include ptosis, ipsilateral lacrimation, conjunctival injection, and rhinorrhea. The pain usually is unilateral, with 60 percent of patients reporting headaches on the right side, but 14 percent of patients report a side shift during an attack, and 18 percent report involvement of different sides in subsequent attacks. (6)
Other symptoms include facial flushing or pallor, tenderness on palpation of the ipsilateral carotid artery, bradycardia, and abnormal feeling of scalp hairs. The absence of aura, nausea, or vomiting has helped distinguish cluster from migraine headaches, but recent studies indicate that 14 percent of patients with cluster headache experience aura, 51 percent have a personal or family history of migraine, 56 percent report photophobia, 43 percent report phonophobia, and 23 percent report osmophobia. (7) Thus, the presence of aura, nausea, vomiting, or photophobia should not rule out a diagnosis of cluster headache. (8) A characteristic feature of cluster headache, noted by 93 percent of patients in one study, (7) is restlessness, with behaviors such as pacing and rocking the head and trunk with head in hands. (9) Most of these headaches last 15 minutes to three hours and recur at the same time of day, often at night. Many attacks begin during the first rapid-eye-movement sleep phase. Patients may report a seasonal pattern, with spring and autumn peaks.
Cluster headache is diagnosed by history, and the key feature is a pattern of recurrent bouts of near-daily attacks lasting for days, weeks, or months. Patients fearing an attack may be afraid to go to sleep. Precipitants of cluster headache include hypoxia, which may occur with sleep apnea. Vasodilators such as nitroglycerin, alcohol, and carbon dioxide may trigger a headache during a cluster period. (10)
Although similar to cluster headache, paroxysmal hemicrania headaches are briefer and are treated effectively with indomethacin. (5) Orbital myositis may mimic cluster headache, but the headache has a longer duration.
Etiology
Positron emission tomographic (PET) scanning and functional magnetic resonance imaging are helping to clarify the poorly understood etiology of cluster headache. The basic pathophysiology is in the hypothalamic gray matter. (11) In some families, an autosomal dominant gene may be involved, but calcium channel activity or nitric oxide sensitivity alleles have not been identified. (12) Carotid and ophthalmic artery vasodilation and an increased sensitivity to vasodilator stimuli during an attack may be triggered by trigeminal parasympathetic reflexes. Abnormal heart rate variability and increased nocturnal lipolysis during attacks and in remission reinforce the theory of an autonomic function abnormality with increased parasympathetic drive and decreased sympathetic function. Attacks often begin during sleep, implicating a disorder of circadian rhythm. (13) An increased incidence of sleep apnea in patients with cluster headache suggests that periods of reduced oxygenation of key tissues may trigger an attack. (14)
Treatment
Cluster headache treatment requires a dual strategy. Acutely, the attack must be aborted or subdued. Concurrently, prophylaxis is initiated to suppress the recurrent headaches expected throughout the remaining cluster period; prophylaxis is continued for the expected duration of the cluster period and then tapered off. Patients with chronic cluster headache require long-term prophylaxis. In patients with intractable headaches, more aggressive intervention, including surgery, may be required.
ACUTE OR ABORTIVE
The treatments of choice for acute cluster headache are oxygen (7 L per minute for 15 minutes), sumatriptan, or a combination of the two (Table 1). (15-21) Both therapies appear to be underprescribed. Sumatriptan is available as a subcutaneous injection or as a nasal spray. (16-18) It is contraindicated in patients with ischemic heart disease, uncontrolled hypertension, or peripheral vascular disease, and it should not be combined with ergotamine. Tachyphylaxis does not occur when the drug is used for long periods. Higher sumatriptan doses (12 mg subcutaneously) were not found to be more effective and had more side effects than 6mg doses. (18)
Intranasal dihydroergotamine can reduce attack severity, but it does not reduce attack frequency or duration. This nasal spray has fewer adverse reactions and better bioavailability than oral ergotamine. (19) Intranasal lidocaine has been shown to decrease pain after five minutes, with nine of nine treated patients free of pain after 35 minutes. (20) Intranasal capsaicin, which is hypothesized to deplete substance P from sensory nerve terminals, is used in treatment of other pain states, including herpes zoster. In a study of patients with cluster headache, it reduced the severity of headaches after seven days of treatment. (21)
The effectiveness of melatonin is unclear because of conflicting studies. (22) Its role, if any, will be in the initial prevention of attacks, theoretically by resetting the circadian rhythm.
PROPHYLACTIC
Oral sumatriptan has not been shown to be effective prophylactically. (23) Verapamil in dosages of 360 to 480 mg daily is one of the few treatments for episodic cluster headache tested in a randomized controlled trial (RCT) and found effective in reducing attack frequency (Table 2). (13,24-31) This treatment also is underused, with only 4 percent of patients with cluster headache reporting prophylactic verapamil use.
Prednisone often is used in prophylaxis, starting at a dosage of 50 to 80 mg daily and tapered over 10 to 12 days. A 1975 study that used a double-blind control methodology led to improvement in 17 of 19 patients compared with placebo, but the study quality was limited. (26) A recent nonrandomized study of cluster headache prophylaxis that used three days of 250 mg of intravenous methylprednisolone followed by a prednisone taper indicated fewer headaches in the active phase than with previous treatments in a group of 14 men. (32) In small studies, the anti-epileptic drugs divalproex and topiramate were found to be useful. (28) Gabapentin and baclofen have been tried with some success in case reports and nonrandomized trials. (28) However, no RCTs have been conducted to ndetermine conclusively the effectiveness of antiepileptic drugs.
Historically, ergotamine in a dosage of 2 to 4 mg per day has been a common agent for episodic prophylaxis, but no RCT of oral ergotamine has been reported. Ergotamine and sumatriptan should not be taken concurrently. In addition, patients with peripheral vascular disease should not take ergotamine. A recent review summarizes management guidelines for patients who continue to use ergotamine or who cannot tolerate verapamil or other prophylactic medications. Patients who experience attacks at night may be given 1- or 2-mg tablets orally or by suppository before bedtime. (13) When headaches start consistently at the same time each day, patients may be advised to take ergotamine 30 to 60 minutes before the time of their usual attack. A combination of verapamil and ergotamine may be considered. (13)
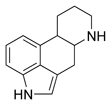
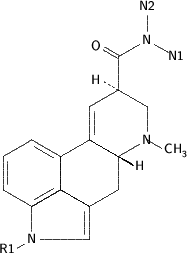
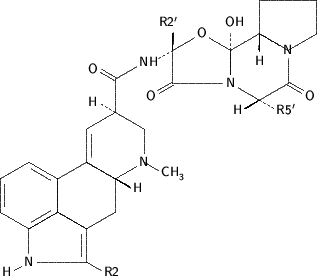
Methysergide previously was used for cluster headache prophylaxis, but its use has been discontinued in the United States because it can cause retroperitoneal, cardiac, and pleuropulmonary fibrosis. Methylergonovine maleate should be restricted to use in refractory cases and should never be used for more than six months continuously. Methylergonovine, probably the active metabolite of methysergide, decreased cluster headache frequency by more than 50 percent in 19 of 20 patients in a pilot study. (32) Contraindications include hypertension and pregnancy. Methylergonovine should be used with caution, if at all, in patients with cardiac or peripheral vascular disease, or hepatic or renal insufficiency. Hallucinations can occur because it is a lysergic acid derivative. (30)
CHRONIC CLUSTER HEADACHE
Verapamil is used in the treatment of chronic cluster hadache. (24) Lithium has been used as long-term prophylaxis for years on the basis of case series demonstrating effectiveness (Table 3). (25,33-35) In an RCT of lithium in episodic cluster headache, substantial improvement occurred in both groups: six (43 percent) of 14 patients in the placebo group and eight (62 percent) of 13 in the lithium group. The study, which was stopped because superiority over placebo could not be demonstrated, challenges physicians to look at the positive treatment effect of placebo. (34)
SURGICAL OPTIONS FOR INTRACTABLE HEADACHE
Microvascular decompression of the fifth cranial nerve with or without section of the nervus intermedius was performed in 30 patients. (35) Initially, 77.3 percent of patients experienced relief, but after five years, only 46.6 percent reported continued excellent or good outcome. Repeat surgeries did not add benefit. It is important to choose a surgical intervention that maintains nerve supply so that facial numbness and corneal anesthesia are less likely to occur.
NEW DIRECTIONS
Patients with severe snoring and cluster headache should be evaluated for sleep apnea. In some patients diagnosed with sleep apnea, treatment for apnea also proved to be effective for the headaches. (14)
Botulinum toxins A and B are being studied as treatments for various headaches, with evidence of some efficacy and mixed reports as to side effects. An ongoing study is addressing their role in chronic cluster headache.
A recent report (35) described a patient with intractable cluster headache; PET scanning revealed activation of the posterior inferior hypothalamic gray matter during attacks. A stereotactic electrode was implanted in this area, with a permanent generator placed in a subclavicular pocket. When stimulation was provided at a frequency of 180 Hz, the attacks disappeared after 48 hours. Twice, the stimulator was turned off without the patient's knowledge, and attacks returned within 48 hours. The latter attacks disappeared 48 hours after the generator was restarted. Thirteen months later, the pain had not recurred.
Behavior and Lifestyle Interventions
Although little research has assessed the effectiveness of psychologic and behavior strategies on cluster headache, these approaches have been supported in the management of migraine and other chronic headaches. Strategies that have proved effective for other headaches target pain intensity and resultant disability, analgesic overuse, adherence to prescribed regimens, and psychiatric comorbidity. The difference between a functional life with pain and a life of significant disability often is related to the patient's ability to pace activities and regulate emotions (thereby decreasing the fear of pain and subsequent autonomic arousal), engage in healthy behaviors, and function despite the presence of pain.
To maximize the quality of life in patients with cluster headache, strategies including relaxation, biofeedback, smoking cessation, and alcohol intake reduction should be considered. The prevalence of cigarette smoking is higher in patients with cluster headache than in control patients. In one retrospective study, (7) however, patients with cluster headache who had stopped smoking did not notice any change in their symptom pattern. Heavy alcohol use is more common in patients who progress to chronic cluster headache compared with those who have episodic headache, although it is unknown whether alcohol is a cause or result of living with chronic pain.
Relaxation training paired with thermal biofeedback is effective in tension and migraine headache treatment. Biofeedback may be effective in patients with post-traumatic headache. (36) For patients with cluster headache and a history of head trauma or migraine, these options may be considered. If cluster headache is an autonomic disorder, biofeedback may be valuable. Cognitive behavior interventions with proven value in migraine treatment (38) that may be considered in patients with cluster headache include discussing reasonable expectations, keeping simple behavior diaries, and emphasizing personal responsibility. Patients are taught self-assessment and self-regulation skills that help them challenge irrational beliefs such as all-or-nothing thinking, catastrophizing outcomes, or attributional styles that lead them toward ineffective strategies (e.g., "I have no control over the pain"). Providing patients with ongoing compassion, knowledge about cluster headache, coping skills, and a long-term trust relationship is crucial in helping them cope with this difficult and painful condition.
* Patient information: A handout on cluster headaches, written by the authors of this article, is provided on page 728.
See page 639 for strength-of-recommendation labels.
REFERENCES
(1.) Newman LC, Goadsby P, Lipton RB. Cluster and related headaches. Med Clin North Am 2001;85:997-1016.
(2.) Manzoni G C. Gender ratio of cluster headache over the years: a possible role of changes in lifestyle. Cephalalgia 1998;18:138-42.
(3.) Swanson JW, Yanagihara T, Stang PE, O'Fallon WM, Beard CM, Melton LJ 3d, et al. Incidence of cluster headaches: a population-based study in Olmsted County, Minnesota. Neurology March 1994;44(3 pt 1):433-7.
(4.) Wheeler SD, Carrazana EJ. Delayed diagnosis of cluster headache in African-American women. J Natl Med Assoc 2001;93:31-6.
(5.) Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders. 2d ed. Cephalalgia 2004;24(suppl 1):9-160.
(6.) Zakrzewska JM. Cluster headache: review of the literature. Br J Oral Maxillofac Surg 2001;39:103-13.
(7.) Bahra A, May A, Goadsby PJ. Cluster headache: a prospective clinical study with diagnostic implications. Neurology 2002;58:354-61.
(8.) Van Vliet JA, Eekers PJ, Haan J, Ferrari MD, Dutch RUSSH Study Group. Features involved in the diagnostic delay of cluster headache. J Neurol Neurosurg Psychiatry 2003;74:1123-5.
(9.) Blau JN. Behaviour during a cluster headache. Lancet 1993;342:723-5.
(10.) Ekbom K, Sjostrand C, Svensson DA, Waldenlind E. Periods of cluster headache induced by nitrate therapy and spontaneous remission of angina pectoris during active clusters. Cephalalgia 2004;24:92-8.
(11.) May A, Bahra A, Buchel C, Frackowiak RS, Goadsby PJ. Hypothalamic activation in cluster headache attacks. Lancet 1998;352:275-8.
(12.) Sjostrand C, Modin H, Masterman T, Ekbom K, Waldenlind E, Hillert J. Analysis of nitric oxide synthase genes in cluster headache. Cephalalgia 2002;22:758-64.
(13.) Ekbom K, Hardebo JE. Cluster headache: aetiology, diagnosis and management. Drugs 2002;62:61-9.
(14.) Nobre ME, Filho PF, Dominici M. Cluster headache associated with sleep apnoea. Cephalalgia 2003;23:276-9.
(15.) Fogan L. Treatment of cluster headache. A double-blind comparison of oxygen v air inhalation. Arch Neurol 1985;42:362-3.
(16.) Treatment of acute cluster headache with sumatriptan. The Sumatriptan Cluster Headache Study Group. N Engl J Med 1991;325:322-6.
(17.) Gobel H, Lindner V, Heinze A, Ribbat M, Deuschl G. Acute therapy for cluster headache with sumatriptan: findings of a one-year long-term study. Neurology 1998;51:908-11.
(18.) Van Vliet JA, Bahra A, Martin V, Ramadan N, Aurora SK, Mathew NT, et al. Intranasal sumatriptan in cluster headache: randomized placebo-controlled double-blind study. Neurology 2003;60:630-3.
(19.) Andersson PG, Jespersen LT. Dihydroergotamine nasal spray in the treatment of attacks of cluster headache. A double-blind trial versus placebo. Cephalalgia 1986;6:51-4.
(20.) Costa A, Pucci E, Antonaci F, Sances G, Granella F, Broich G, et al. The effect of intranasal cocaine and lidocaine on nitroglycerin-induced attacks in cluster headache. Cephalalgia 2000;20:85-91.
(21.) Marks DR, Rapoport A, Padla D, Weeks R, Rosum R, Sheftell F, et al. A double-blind placebo-controlled trial of intranasal capsaicin for cluster headache. Cephalalgia 1993;13:114-6.
(22.) Pringsheim T, Magnoux E, Dobson CF, Hamel E, Aube M. Melatonin as adjunctive therapy in the prophylaxis of cluster headache: a pilot study. Headache 2002;42:787-92.
(23.) Monstad I, Krabbe A, Micieli G, Prusinski A, Cole J, Pilgrim A, et al. Preemptive oral treatment with sumatriptan during a cluster period. Headache 1995;35:607-13.
(24.) Leone M, D'Amico D, Frediani F, Moschiano F, Grazzi L, Attanasio A, et al. Verapamil in the prophylaxis of episodic cluster headache: a double-blind study versus placebo. Neurology 2000;54:1382-5.
(25.) Bussone G, Leone M, Peccarisi C, Micieli G, Granella F, Magri M, et al. Double blind comparison of lithium and verapamil in cluster headache prophylaxis. Headache 1990;30:411-7.
(26.) Jammes JL. The treatment of cluster headaches with prednisone. Dis Nerv Syst 1975;36:375-6.
(27.) Couch JR Jr, Ziegler DK. Prednisone therapy for cluster headache. Headache 1978;18:219-21.
(28.) Rozen TD. Antiepileptic drugs in the management of cluster headache and trigeminal neuralgia. Headache 2001;41(suppl 1):S25-S32.
(29.) Mathew NT, Kailasam J, Meadors L. Prophylaxis of migraine, transformed migraine, and cluster headache with topiramate. Headache 2002;42:796-803.
(30.) Mueller L, Gallagher RM, Ciervo CA. Methylergonovine maleate as a cluster headache prophylactic: a study and review. Headache 1997;37:437-42.
(31.) Leone M, D'Amico D, Moschiano F, Fraschini F, Bussone G. Melatonin versus placebo in the prophylaxis of cluster headache: a double-blind pilot study with parallel groups. Cephalalgia 1996;16:494-6.
(32.) Mir P, Alberca R, Navarro A, Montes E, Martinez E, Franco E, et al. Prophylactic treatment of episodic cluster headache with intravenous bolus of methylprednisolone. Neurol Sci 2003;24:318-21.
(33.) Steiner TJ, Hering R, Couturier EG, Davies PT, Whitmarsh TE. Double-blind placebo-controlled trial of lithium in episodic cluster headache. Cephalalgia 1997;17:673-5.
(34.) Lovely TJ, Kotsiakis X, Jannetta PJ. The surgical management of chronic cluster headache. Headache 1998;38:590-4.
(35.) Leone M, Franzini A, Bussone G. Stereotactic stimulation of posterior hypothalamic gray matter in a patient with intractable cluster headache. N Engl J Med 2001;345:1428-9.
(36.) Ham LP, Packard RC. A retrospective, follow-up study of biofeedback-assisted relaxation therapy in patients with posttraumatic headache. Biofeedback Self Regul 1996;21:93-104.
(37.) Kropp P, Gerber WD, Keinath-Specht A, Kopal T, Niederberger U. Behavioral treatment in migraine. Cognitive-behavioral therapy and blood-volume-pulse biofeedback: a cross-over study with a two-year follow-up. Funct Neurol 1997;12:17-24.
ELLEN BECK, M.D., is director of community education in the Division of Family Medicine in the Department of Family & Preventive Medicine at the University of California, San Diego (UCSD), School of Medicine, in La Jolla. She is director of the UCSD student free clinic project and a clinician at La Maestra community health center in San Diego. She received her medical degree from McGill University and completed a family medicine residency at Jewish General Hospital, both in Montreal, Quebec.
WILLIAM J. SIEBER, PH.D., is assistant clinical professor in the Department of Family & Preventive Medicine at UCSD. He earned a doctoral degree in clinical psychology from Yale University.
RAUL TREJO, M.D., is faculty in the Scripps Chula Vista family practice residency and Department of Family & Preventive Medicine at UCSD School of Medicine, and a clinician at the San Ysidro Community Health Center in Chula Vista, Calif. He received his medical degree from Harvard Medical School, Boston, and completed a family practice residency at the Scripps Family Practice Residency Program in Chula Vista, Calif.
Address correspondence to Ellen Beck, M.D., University of California, San Diego, Department of Family & Preventive Medicine, 9500 Gilman Dr., La Jolla, CA 92093-0696 (e-mail: ebeck@ucsd.edu). Reprints are not available from the authors.
The authors thank Alicia Johnson and Carol Bloom-Whitener for administrative support and assistance in the preparation of the manuscript.
Members of various family medicine departments develop articles for "Practical Therapeutics." This article is one in a series from the Department of Family and Preventive Medicine at the University of California, San Diego. The coordinator of the series is Tyson Ikeda, M.D., director of the Family Medicine Residency Program.
The authors indicate that they do not have any conflicts of interest. Sources of funding: none reported.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group