SCOTTSDALE, ARIZ. -- Headaches during pregnancy and the postpartum period are common, but challenges lie in considering safe diagnostic measures and the teratogenic risk of drugs when offering treatment, Dr. Christine Lay reported during a symposium that was sponsored by the American Headache Society.
Possible causes of headache during pregnancy include migraine and (less commonly) sinusitis, mass or tumor, sub-arachnoid hemorrhage, central venous thrombosis, idiopathic intracranial hypertension, and eclampsia.
If secondary headache is suspected, testing--including neuroimaging--should be considered, she advised at the meeting.
Head CT is considered to be "relatively safe" and helpful in cases of suspected subarachnoid hemorrhage or in head trauma cases, said Dr. Lay, a neurologist with the Headache Institute at St. Luke's-Roosevelt Hospital Center, New York.
Magnetic resonance imaging during pregnancy, however, may carry a potential risk and should be used only when absolutely necessary, according to Dr. Lay.
Gadolinium and CT contrast should be avoided in pregnant women, and lumbar puncture should follow imaging if raised intracranial pressure is suspected, but should not be delayed if meningitis is suspected, she said.
While migraines may either improve or worsen during pregnancy, Dr. Lay described findings from one recent study of 40O pregnant women indicating that 50% of women saw improvement by the end of their first trimester, and 90% reported either improvement or cessation of headache by the end of the third trimester.
"We think the improvement [in later pregnancy] is on the basis of stabilization of estrogen levels," Dr. Lay noted at the meeting.
Since most drugs cross the placenta, the risk of an adverse effect on the fetus must be considered in treating headaches.
She cautioned that negative results of drug testing on animal models may not predict a lack of teratogenicity in humans, as was demonstrated in the case of thalidomide.
With 3% of birth defects caused by drug exposure, Dr. Lay advised that migraine drugs should not be administered to pregnant women or to those who are trying to conceive.
Instead, she emphasized that reassurance, rest, ice packs, and biofeedback techniques can help women endure migraines before and during the first trimester, and in many cases, migraines improve later in pregnancy.
"If they can make it through the first trimester with nonpharmacologic approaches, that's huge because once 12 weeks have passed, much development has taken place and drugs have a reduced likelihood of having teratogenic effects," she added.
Both small doses of caffeine (less than 300 mg) and aceta minophen are generally safe for use during the first trimester, according to Dr. Lay.
Nonsteroidal anti-inflammatory drugs are sometimes used, but these should be avoided during the third trimester.
Category B NSAIDs, including diclofenac, flurbiprofen, ibuprofen, ketoprofen, and indomethacin, are all considered Category D in the third trimester.
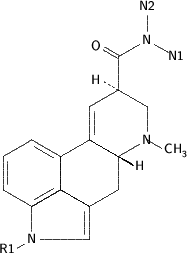
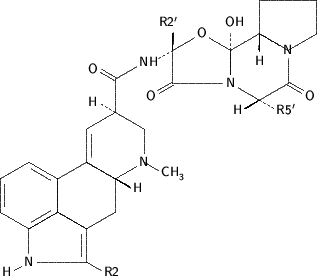
Dr. Lay cautioned that the use of aspirin, ergotamine, dihydroergotamine, and the triptans should be avoided in pregnancy.
Since severe, intractable migraine (often including nausea, vomiting, and dehydration) can pose a risk to a developing fetus, medical therapy may be indicated--including the administration of intravenous fluids and an intravenous antiemetic.
Preventive therapy may be necessary in cases of disabling migraine (three to four severe migraines per month), but should be offered only with full consent of the patient and her partner.
Most preventatives are Category C or higher.
The use of antidepressants has been suggested as possibly increasing risk of miscarriage.
Fluoxetine may be safer, but its effectiveness on migraine prophylaxis may not be substantial.
Anticonvulsants are not recommended for migraine prophylaxis in pregnant women.
The rapid drop in estrogen levels is believed to increase the likelihood of migraine recurrence in the postpartum period and, since many women are breast-feeding, certain drugs should be avoided.
The American Academy of Pediatrics cautions that drugs to be avoided during breast-feeding include antihistamines, ergotamine, bromocriptine, and most tricyclics.
In addition, caution should be used in prescribing triptans, benzodiazepines, antidepressants, and neuroleptics, she added.
COPYRIGHT 2004 International Medical News Group
COPYRIGHT 2004 Gale Group