Rationale: The airway surface liquid, the thin layer of liquid covering the airways, is essential for mucociliary clearance and as a barrier against microbial and other noxious agents. Proteins secreted into the airway surface liquid by epithelial and nonepithelial cells may be important in innate immunity and to improve the fluidity of mucous secretions.
Objectives: We aimed to identify proteins specifically secreted into the airway surface liquid by human bronchial epithelial cells, in resting conditions and after treatment with interleukin 4 (IL-4), a cytokine released in asthma.
Methods and Main Results: By using a proteomics approach, we found that one of the most abundant proteins was gelsolin, which breaks down actin filaments. Gelsolin mRNA and protein secretion were increased threefold in the airway surface liquid of epithelia treated with IL-4. These results were confirmed at the functional level by measuring actin depolymerization using a fluorescence assay. Gelsolin protein was also upregulated in the airways of subjects with asthma.
Conclusions: Our findings indicate that gelsolin is released by epithelial cells into the airways and that its secretion is increased by IL-4 in vitro. In addition, we found that the concentration of both IL-4 and gelsolin were raised in the bronchoalveolar lavage of patients with asthma. These results suggest that gelsolin might improve the fluidity of airway surface liquid in asthma by breaking down filamentous actin that may be released in large amounts by dying cells during inflammation.
Keywords: actin; epithelium; mucociliary clearance
Allergic asthma is an inflammatory disorder of the airways associated with bronchial hyperresponsiveness and variable airflow obstruction. In addition, individuals with asthma frequently suffer from mucus overproduction, which is believed to contribute to airway obstruction (1). There is compelling evidence that T-helper type 2 (Th2) lymphocytes, and the cytokines that they produce (i.e., interleukin 4 [IL-4], IL-5, IL-9, and IL-13), may be involved in the orchestration of airway inflammation. IL-4 is the major factor regulating IgE production by B cells, and is required for optimal Th2 lymphocyte differentiation (2). IgE-mediated immune responses are further enhanced by IL-4 through upregulation of IgE receptors on the surface of B cells. IL-4 contributes to airway obstruction in asthma through the induction of mucin gene expression and the hypersecretion of mucus (3). IL-4 promotes cellular inflammation in the asthmatic lung by the induction of vascular cell adhesion molecule-1 on vascular endothelium (3). In patients with asthma, T cells producing IL-4, IL-5, IL-9, and IL-13 have been identified in bronchoalveolar lavage fluid (BALF) (2,4, 5). Furthermore, concentration of IL-4 is elevated in BALF from patients with asthma, although the levels demonstrate considerable variability (6-8).
The airway surface is covered by a thin fluid layer, the airway surface liquid (ASL), which has an essential role as a barrier to protect the underlying epithelium (9). Air contains particulate material, such as pollen, ash, mineral dust, bacteria, and viruses, all of which are capable of damaging the lungs either directly or by predisposing the lung to infection. The airways must be able to handle this load by neutralizing, and discarding, injuring agents, as well as repairing any resultant damage to cells. In addition, recent studies have demonstrated that airway epithelial cells can produce a wide variety of cytokines that promote the differentiation of inflammatory cells and other multifunctional factors that initiate and amplify inflammatory events (2). We and other authors have previously shown that IL-4 and IL-13 (10,11) modify the ion transport properties of cultured cells by changing the expression and activity of ion channels favoring Cl- secretion over Na+ absorption. The consequent changes in volume and composition of ASL secretions could have a considerable influence on the mucociliary clearance and viscosity of mucous secretions. We hypothesized that some of the proteins secreted into the ASL to improve mucociliary clearance, or increase antimicrobial defense in asthma, could be modulated by IL-4. Recently, a database of proteins recovered by BAL has been created using two-dimensional electrophoresis (12). Moreover, Magi and colleagues (13), using a proteomics approach to study the BALF obtained from patients with sarcoidosis and idiopathic pulmonary fibrosis, have identified a number of proteins that may have pathogenic roles in these diseases. However, interpreting the source of proteins present in BALF is difficult because they may have many different origins, including diffusion from serum, production by pulmonary T cells, synthesis by alveolar cells or by alveolar macrophages, or secretion by surface bronchial epithelial cells or submucosal gland cells.
To overcome the problem of multiple cellular sources of secreted proteins in this study, we have used a proteomics strategy to identify the proteins secreted specifically by airway epithelial cells in resting and stimulated conditions. Analysis of the protein content from the ASL of polarized human bronchial epithelial cell cultures shows that one of the most abundant proteins is gelsolin, which breaks down actin filaments. We also find that gelsolin protein levels are increased in cell cultures treated with IL-4 and in BALF of patients with asthma. This finding suggests an important role for gelsolin in the ASL barrier function and indicates that exogenous gelsolin might be considered for therapeutic use in diseases characterized by chronic inflammation with significant levels of filamentous actin release, such as cystic fibrosis (CF) (14).
Some of the results of these studies have been previously reported in the form of an abstract (15).
METHODS
Human bronchi were obtained from lung resections or lobectomies and cultured as previously described (10, 16, 17). The collection and processing of human cells were approved by the local ethics committee. To obtain polarized epithelia, human bronchial epithelial cells were plated on transwell clear permeable supports (Corning Costar; Celbio, Milan, Italy). The apical culture medium was removed, and epithelia maintained in an air-liquid interface (i.e., with culture medium only on the basolateral side). Under these conditions, the epithelia maintain a thin layer of liquid similar to the ASL in vivo (18). IL-4, 10 ng/ml, was added daily to the basolateral medium and was maintained for 24 to 120 h. Collection of ASL proteins was achieved by washing the apical side of polarized epithelium with Ringer's solution.
BALF Samples
BALF samples were obtained from six nonasthmatic, nonatopic subjects (mean age, 32 ± 3 yr) on one occasion, and from six subjects with atopic asthma (mean age, 26 ± 1 yr) on two occasions, before and 24 h after inhaled allergen challenge (house dust mite, cat hair dander, or grass pollen, as appropriate). All subjects provided informed consent, and the study was approved by the local research ethics committee of King's College Hospital, London. Bronchoscopy was performed according to the standard operating procedure of King's College Hospital.
Two-Dimensional Gel Electrophoresis
BALF and ASL samples were treated as previously reported (f9, 20). Samples were separated in the first dimension on soft, immobilized pH gradient, in a nonlinear pH 3-10 interval (21, 22). In the second dimension, proteins were separated based on their molecular weight in polyacrylamide gels, 180 × 160 × 1.5 mm. Proteins were visualized by a double staining procedure: first, the methyl-trichloroacetate negative staining (23), followed by the silver staining (24) for the analytic image, or colloidal Coomassie staining (25) for mass spectrometry analysis. Additional details on the methods are provided in an online supplement.
Mass Spectrometry
After visualization with colloidal Coomassie blue staining, electrophoretic spots were excised and proteins digested as previously described (26). Peptide mass fingerprinting spectra were acquired using an Ettan MALDI-ToF mass spectrometer (Amersham Biosciences, Uppsala, Sweden). Peptide sequencing was performed using an LCQDeca ESI-Ion Trap mass spectrometer (Thermo, San Jose, CA). Database searching for protein identification was performed using available online software.
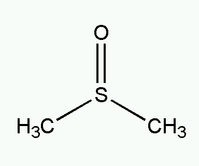
Gelsolin Functional Assay
Rabbit muscle actin was dissolved in a low-ionic-strength solution, diluted with a polymerizing buffer, and stored in small aliquots at -20°C. Rhodamine phalloidin was dissolved in dimethyl sulfoxide at a concentration of 500 µM and stored at -20°C. Human plasma gelsolin was dissolved and stored at -80°C at a final concentration of 400 nM. Fluorescence intensity was measured with a fluorescence microplate reader (FluoStar Galaxy; BMG LabTechnologies, Germany) using 96-well, black, clear-bottom plates. We used high-quality filters (Chroma Technology, Rockingham, VT) with maximal transmittance at 540 and 590 nm for excitation and emission, respectively. Additional details are provided in the online supplement.
Statistics
Results are presented as representative data or as arithmetic means plus SEM. Significance was determined on unpaired groups of data using two-tailed Student's t test, if not otherwise indicated, or by nonparametric Kruskal-Wallis followed by Dunn's multiple comparison test.
RESULTS
Two-Dimensional Gel Analysis of Cultured Cells' ASL
Analytic gels prepared with the proteins recovered from the apical surface of cultured airway epithelia showed hundreds of silver-stained spots (Figure 1, top panel). Side-by-side comparison of gels prepared with samples from cultures treated with and without IL-4 revealed changes in intensity and/or mobility of some of the spots. Particularly evident were the modifications of two clusters of spots or charge trains (circled in Figure 1, bottom panels) with apparent molecular weights of 85 and 45 kD. For each molecular weight, up to seven distinct spots could be distinguished that were positioned between an isoelectric point range of 5.6 to 6.2 for the 85-kD cluster, and 5 to 5.2 for the 45-kD cluster. As shown in Figure 1 (bottom panels), the spots in the two clusters were significantly increased in intensity when the cells were treated with IL-4. Preparative gels were generated for protein identification. Recovery of the single spots and subsequent mass spectrometric analysis revealed that the polypeptides in both spot clusters belonged to gelsolin. The presence of charge trains of the same protein indicates various degrees of in vivo modifications, such as glycosylation, phosphorylation, or acetylation, which affect electrophoretic mobility (27). The sequences of fragments from the low-molecular-weight spots matched with the carboxyl-terminal half of the human gelsolin sequence (Figure 2). Conversely, sequences obtained from the high-molecular-weight cluster matched with the whole gelsolin. Spots that were expected to correspond to actin were confirmed by mass spectrometry. In contrast to gelsolin, the intensity of actin charge trains was not modified by IL-4 (underlined in Figure 1). None of the spots recovered from two-dimensional gels corresponded to the amino-terminal half of gelsolin.
Quantification of Gelsolin Protein and mRNA
We performed densitometric analysis of protein spots from two-dimensional gels from untreated and IL-4-treated cells (Figure 3A). Our results demonstrated that secreted gelsolin increased threefold at 24 h after IL-4 stimulation and remained upregulated for the following 96 h. We confirmed the presence of 85- and 45-kD bands by Western blot using an antibody against human gelsolin (Figure 3B; for details on method, see online supplement). Intensity of both bands increased after IL-4 treatment, by approximately three- and twofold for the high- and low-molecular-weight material, respectively. We then reasoned that the upregulation of gelsolin protein was caused by an increase in gelsolin mRNA. We therefore quantified gelsolin mRNA using real-time reverse transcriptase-polymerase chain reaction (Figure 3C; for details on the method used, see online supplement). Our data showed that gelsolin transcript was significantly increased at 6 h after IL-4 addition, reached a peak at 24 h, and then started to decrease.
Functional Analysis of Gelsolin
Gelsolin cleaves actin filaments (28). To evaluate the presence and upregulation of gelsolin at the functional level in the ASL of cultured cells, we used an assay based on the properties of rhodamine-labeled phalloidin to increase its fluorescence emission when bound to polymerized but not to depolymerized actin (29). In the absence of gelsolin, addition of polymerized actin caused a fuorescence enhancement of 233 ± 15.8% (from 3,490 ± 203 to 8,121 ± 609 arbitrary units, n = 14). This effect was slow, requiring approximately 7 to 8 min to reach a stable fluorescence level (not shown). The addition of human gelsolin to the reaction mixture caused a dose-dependent reduction of actin-dependent signal (Figures 4A and 4B). The gelsolin response was normalized by taking the fluorescence with phalloidin plus actin and that with phalloidin alone as 100 and 0%, respectively (see Figure 4A). The fit of experimental data to a Michaelis-Menten function yielded a half-effective concentration of 24.7 nM. After generating a calibration curve, we tested the effect of ASL samples from cultured cells. The ASL lavage from untreated epithelia did not change the fluorescence of the phalloidin-actin complex (Figure 4C). In contrast, 20 µl ASL lavage from IL-4-treated epithelia caused a clear fluorescence reduction of 38.1 ± 12% (Figure 4D; n = 6; p
Detection of Gelsolin in BALF
To verify whether gelsolin is secreted into the airways in vivo, we analyzed BALF samples from six nonasthmatic and from six patients with asthma (Figure 5). Protein spots corresponding to the molecular weights of the two forms of gelsolin and actin were identified. The high-molecular-weight spots of gelsolin were partially covered by the big spot corresponding to albumin. However, two-dimensional gels showed that gelsolin spots of low molecular weight in patients with asthma were more intense than in control patients, whereas actin spots were unchanged (Figure 5, bottom). These findings were confirmed in Western blots using the antihuman gelsolin antibody and extended to the high-molecular-weight form of gelsolin as well (Figure 6). The 85- and the 45-kD bands, particularly the latter one, were more intense when obtained from patients with asthma than from nonasthmatic individuals. We also analyzed the BALF from patients with asthma after an allergen challenge (see METHODS). We found that the abundance of the high-molecular-weight gelsolin was similar before and after allergen, whereas the low-molecular-weight band intensity decreased to values similar to those of nonasthmatic patients.
Detection of IL-4 in BALF
We wanted to establish whether there was a correlation in BALF between gelsolin and IL-4 levels. We therefore measured IL-4 concentration by ELISA (see the online supplement) in the BALF of the same control subjects and subjects with asthma from which gelsolin was determined. The BALF from control patients contained low levels of IL-4 (0.68 ± 0.12 pg/ml). In contrast, the IL-4 content from patients with asthma was 14-fold higher (9.68 ± 1.7 pg/ml). After exposure to allergen, patients with asthma displayed IL-4 values similar to those of non-asthmatic subjects (0.76 ± 0.26 pg/ml).
DISCUSSION
Proteomics is a powerful approach to analyze the protein content in biological fluids. Comparison of two samples of protein mixtures (normal vs. affected, treated vs. untreated) by two-dimensional gel electrophoresis, followed by identification of the proteins by mass spectrometry, can detect the presence of novel proteins, reveal new roles for detected proteins, and discover patterns of regulated post-translational modifications (30). Regarding the airways, a database of BAL proteins has recently been created using two-dimensional electrophoresis (12). A variety of soluble components from human lung have been identified, including approximately 80 proteins. Analysis of BAL protein content is complicated by the presence of proteins derived from many different sources, including leukocytes, serum, submucosal glands, and surface epithelium. This study therefore adopted a simplified approach by using an in vitro model of differentiated airway epithelium. We have found that the ASL of polarized human bronchial epithelia contains gelsolin whose secretion is significantly stimulated by treatment with IL-4.
Gelsolin is the most potent protein that severs actin filament identified to date (28). This protein weakens noncovalent bonds between actin filaments so that they can then be broken. This effect is rapid, stoichiometric, and highly efficient. Interaction of gelsolin with actin is strongly Ca^sup 2+^-dependent (31). However, when gelsolin is cleaved by caspase-3, the effector caspase in apoptosis (28), or by other proteases, it becomes Ca^sup 2+^-independent. Indeed, gelsolin is formed by two tandem homologous halves connected by a long linker where the protease site is located. The isolated C-half can bind a single actin molecule but only when Ca^sup 2+^ concentration is higher than 1 µM. The isolated N-half binds two actin molecules even in the absence of Ca^sup 2+^ (28, 32). Recently, evidence that gelsolin is a substrate of metalloproteinase 14 has been provided (33). Gelsolin might also be cleaved by proteases involved in epithelial remodeling that are expressed in the airways, in particular, by metalloproteinases 2 and 9, which have been found increased in the lung in inflammatory lung diseases, including asthma (34).
We did not observe the amino-terminal half of gelsolin in our two-dimensional gels. Possible explanations are as follows: first, gelsolin is usually cleaved inside the cell, and only the complete and the C-half forms are secreted into the ASL; second, that the N-half is secreted into the ASL but it is further digested by other proteases; third, given that it is Ca^sup 2+^-independent, the N-half of gelsolin is bound to actin filaments present in the ASL and not loaded into the two-dimensional gels because of their big size. Besides being involved in the dynamic remodeling of actin filaments inside cells, gelsolin is also secreted into the extracellular space. Considerable amounts of actin are released into the extracellular space during acute lung injury, and circulating actin-gelsolin complexes can be detected in the peripheral blood (35). In the plasma, gelsolin acts as an actin-scavenging protein to prevent increases in blood viscosity due to actin leakage from dying cells. Gelsolin may serve a similar role in the ASL. Because actin is one of the most abundant intracellular proteins, cell death that may occur during inflammatory processes can release large amounts of filamentous actin in the airways, thus increasing the viscosity of mucous secretions. Evidence for this comes from studies on patients with CF. In CF, disruption of chloride secretion, mediated by the CFTR protein, causes dehydration of airway surface and inflammation (9). Mucociliary clearance is severely impaired and the airways become susceptible to mucus plugging and infection. It is well known that one of the major sources of sputum viscosity in CF comes from the DNA released by dying cells. Vasconcellos and colleagues (14) have shown that sputum samples from patients with CF also contain large amounts of filamentous actin, and that this contributes significantly to sputum viscosity. Indeed, the authors demonstrated that addition of gelsolin in vitro to CF sputum decreased the viscosity, thus emphasizing the possible use of exogenous gelsolin as a mucolytic agent. The presence of endogenous gelsolin in the airways was not investigated in that study.
Our results now demonstrate that gelsolin is a protein normally secreted into the ASL by bronchial epithelial cells, and that its levels are high and significantly upregulated by stimulation with IL-4. Quantification by real-time reverse transcriptase-polymerase chain reaction shows an increase of gelsolin mRNA in IL-4-treated cells, which is consistent with upregulation of the corresponding protein in the ASL. Therefore, our results are consistent with an increase in gelsolin protein synthesis due to enhanced gene transcription or enhanced stability of gelsolin mRNA.
We performed functional assays to check whether the gelsolin protein found in the cultured cells' ASL retains its ability to depolymerize actin filaments. We found no gelsolin-like activity in untreated cells. This could be due to lack of sensitivity of our assay or, more probably, to the fact that gelsolin was already complexed to endogenous actin. In contrast, in IL-4-treated cells we found significant depolymerization of exogenous actin, which could be due to excess of free gelsolin. Our findings suggest that the stimulation by IL-4 can create a reserve of gelsolin in airway periciliary fluid and this may in turn degrade filamentous actin that is leaked from dying cells.
IL-4 is a cytokine particularly important in asthma. It is part of a cascade that causes release of chemoattractant molecules, recruitment of leukocytes into the airway lumen, and consequent release of proinflammatory mediators, proteases, and mucus hypersecretion (36). Significant release of actin filaments would be expected as a consequence of the resulting inflammation and cell damage. We therefore speculate that IL-4-induced gelsolin upregulation may be part of a complex host antiinflammatory response.
Patients with asthma had increased amounts of gelsolin protein in their airways with respect to control subjects. It is tempting to conclude that, in agreement with our in vitro results, this upregulation is a result of the enhanced levels of IL-4 in the airways of patients with asthma. Indeed, we found that IL-4 was increased in the BALF of patients with asthma by 14-fold with respect to the level found in the BALF of nonasthmatic subjects. The low IL-4 values found in control subjects (0.68 ± 0.12 pg/ml) are similar to those reported by others (6, 7, 37). IL-4 levels in BALF from patients with asthma are more controversial, probably depending on patients' selection criteria and disease severity. Some authors reported IL-4 levels in patients with asthma similar to control subjects (6). Others reported undetectable IL-4 levels but using an assay with a lower sensitivity (7). Finally, other investigators have found increased IL-4 in the BALF of allergic patients with asthma (38) in agreement with our results. We found a correlation between IL-4 and gelsolin levels: both are low in control subjects and increased in patients with asthma. These data further support the notion that gelsolin secretion in asthma is regulated by IL-4.
Surprisingly, after stimulation with allergens, patients with asthma showed a decrease of the low-molecular-weight form of gelsolin. This finding and the role of the two gelsolin forms is not clear. The IL-4 level in the BALF was also reduced after allergen exposure and this result is in contrast with previous reports (6, 7). We have no explanation for this difference, but it is possible that allergen caused release of mast cell proteases and this might have cleaved the cytokine.
In conclusion, our study reports for the first time the expression and secretion of gelsolin by airway epithelial cells and its regulation by IL-4, supporting the view that ASL has an important role as a first line of host defense. A recent report reveals an important additional function that gelsolin may play in the airways (39). In that study, the authors show that the activity of some antimicrobial peptides, which have the characteristic of being polyvalent cations, is inhibited by filamentous actin through the formation of aggregates. The filament association, and thus the antimicrobial activity inhibition, is reversed by gelsolin. Therefore, gelsolin can be important not only to control mucus viscosity but also to preserve the innate antimicrobial activity in the airway surface. Given the stoichiometric nature of the interaction between gelsolin and actin, massive actin release, which happens during severe inflammatory processes as in CF, may overwhelm the capacity of endogenous gelsolin. This may perhaps be an indication for the therapeutic use of exogenous gelsolin or of other actin-severing agents in diseases characterized by massive airway inflammation with significant levels of filamentous actin release. Nevertheless, caution must be taken because, in another report, actin was found to bind IL-8 in the airways, preventing this chemokine from binding to neutrophil receptors (40). These authors found that gelsolin releases IL-8 from actin, increasing the proportion of free cytokine, and therefore the possible level of inflammation.
Conflict of Interest Statement: G.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. M.B. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. N.P. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. E.C. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. S.L. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. L.B. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. C.P. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. M.V. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. B.J.O. serves on advisory boards for GlaxoSmithKline (GSK), Boehringer Ingelheim, Atlana, Trinity Chiesi, and Celgene, and has received compensation for this activity. He has also received lecture fees from GSK and Pfizer. He runs a clinical academic research unit, which receives grants from major respiratory pharmaceutical companies, including GSK, Aventis, UCB, Pfizer, and Nicox to evaluate potential new therapies for asthma. He also received unrestricted grants to support Ph.D. studentships from GSK and Pfizer. T.H.L. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. L.J.V.G. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript. O.Z.-M. does not have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
References
1. Zhou Y, McLane M, Levitt RC. Th2 cytokines and asthma: interleukin-9 as a therapeutic target for asthma. Respir Res 2001;2:80-84.
2. Renauld JC. New insights into the role of cytokines in asthma. J Clin Pathol 2001;54:577-589.
3. Steinke JW, Borish L. Th2 cytokines and asthma. Interleukin-4: its role in the pathogenesis of asthma, and targeting it for asthma treatment with interleukin-4 receptor antagonists. Respir Res 2001;2:66-70.
4. Bakakos P, Pickard C, Smith JL, Frew AJ. TCR usage and cytokine expression in peripheral blood and BAL T cells. Clin Exp Immunol 2002;128:295-301.
5. Brightling CE, Symon FA, Birring SS, Bradding P, Pavord ID, Wardlaw AJ. TH2 cytokine expression in bronchoalveolar lavage fluid T lymphocytes and bronchial submucosa is a feature of asthma and eosinophilic bronchitis. J Allergy Clin Immunol 2002;110:899-905.
6. Batra V, Musani AI, Hastie AT, Khurana S, Carpenter KA, Zangrilli JG, Peters SP. Bronchoalveolar lavage fluid concentrations of transforming growth factor (TGF)-beta1, TGF-beta2, interleukin (IL)-4 and IL-13 after segmentai allergen challenge and their effects on alpha-smooth muscle actin and collagen III synthesis by primary human lung fibroblasts. Clin Exp Allergy 2004;34:437-444.
7. Kroegel C, Julius P, Matthys H, Virchow JC Jr, Luttmann W. Endobronchial secretion of interleukin-13 following local allergen challenge in atopic asthma: relationship to interleukin-4 and eosinophil counts. Eur Respir J 1996;9:899-904.
8. Virchow JC Jr, Kroegel C, Walker C, Matthys H. Inflammatory determinants of asthma severity: mediator and cellular changes in bronchoalveolar lavage fluid of patients with severe asthma. J Allergy Clin lmmunol 1996;98:S27-S33. [Discussion: S33-S40.]
9. Widdicombe JH. Regulation of the depth and composition of airway surface liquid. J Anat 2002;201:313-318.
10. Galietta LJV, Pagesy P, Folli C, Caci E, Romio L, Costes B, Nicolis E, Cabrini G, Goosscns M, Ravazzolo R, et al. IL-4 is a potent modulator of ion transport in the human bronchial epithelium in vitro. J Immunol 2002;168:839-845.
11. Danahay H, Atherton H, Jones G, Bridges RJ, Poll CT. Interleukin-13 induces a hypersecretory ion transport phenotype in human bronchial epithelial cells. Am J Physiol Lung Cell Mol Physiol 2002;282:L226-L236.
12. Noel-Georis I, Bernard A, Falmagne P, Waltiez R. Database of bronchoalveolar lavage fluid proteins. J Chromatogr B Analyt Technol Biomed Life Sci 2002;771:221-236.
13. Magi B, Bini L, Perari MG, Fossi A, Sanchez JC, Hochstrasser D, Paesano S, Raggiaschi R, Santucci A, Pallini V, et al. Bronchoalveolar lavage fluid protein composition in patients with sarcoidosis and idiopathic pulmonary fibrosis: a two-dimensional electrophoretic study. Electrophoresis 2002;23:3434-3444.
14. Vasconcellos CA, Allen PG, Wohl ME, Drazen JM, Janmey PA, Stossel TP. Reduction in viscosity of cystic fibrosis sputum in vitro by gelsolin. Science 1994;263:969-971.
15. Zegarra-Moran O, Candiano G, Bruschi M, Caci E, Bini L, Liberatori S, Pedemonte N, Galietta LJ. Increased gelsoilin secretion in interleukin-4 treated bronchial epithelial cells and in asthmatic patients. Pediatr Pulmonol 2004;S27:146.
16. Zegarra-Moran O, Romio L, Folli C, Caci E, Becq F, Vierfond JM, Mettey Y, Cabrini G, Fanen P, Galietta LJ. Correction of G551D-CFTR transport defect in epithelial monolayers by genistein but not by CPX or MPB-07. Br J Pharmacol 2002;137:504-512.
17. Galietta LJV, Lantero S, Gazzolo A, Sacco O, Romano L, Rossi GA, Zegarra-Moran O. An improved method to obtain highly differentiated monolayers of human bronchial epithelial cells. In Vitro Cell Dev Biol Anim 1998;34:478-481.
18. Johnson LG, Dickman KG, Moore KL, Mandel LJ, Boucher RC. Enhanced Na+ transport in an air-liquid interface culture system. Am J Physiol 1993;264:L560-L565.
19. Mastro R, Hall M. Protein delipidation and precipitation by tri-n-butylphosphate, acetone, and methanol treatment for isoelectric focusing and two-dimensional gel electrophoresis. Anal Biochem 1999;273: 313-315.
20. Herbert B, Galvani M, Hamdan M, Olivieri E, MacCarthy J, Pedersen S, Righetti PG. Reduction and alkylation of proteins in preparation of two-dimensional map analysis: why, when, and how? Electrophoresis 2001;22:2046-2057.
21. Candiano G, Musante L, Bruschi M, Ghiggeri GM, Herbert B, Antonucci F, Righetti PG. Two-dimensional maps in soft immobilized pH gradient gels: a new approach to the proteome of the third millennium. Electrophoresis 2002;23:292-297.
22. Bruschi M, Musante L, Candiano G, Ghiggeri GM, Herbert B, Antonucci F, Righetti PG. Soft immobilized pH gradient gels in proteome analysis: a follow-up. Proteomics 2003;3:821-825.
23. Candiano G, Porotto M, Lanciotti M, Ghiggeri GM. Negative staining of proteins in polyacrylamide gels with methyl trichloroacetatc. Anal Biochem 1996;243:245-248.
24. Candiano G, Ghiggeri GM, Delfino G, Biggi S, Queirolo C. Silver stain of proteins in ultra-thin gels containing carrier ampholytes: detection of glycosyl albumin with anionic and cationic charge in serums of diabetic patients. Clin Chim Acta 1984;139:195-201.
25. Candiano G, Bruschi M, Musante L, Santucci L, Ghiggeri GM, Carnemolla B, Orecchia P, Zardi L, Righetti PG. Blue silver: a very sensitive colloidal Coomassie G-250 staining for proteome analysis. Electrophoresis 2004;25:1327-1333.
26. Hellman U, Wernstedt C, Gonez J, Heldin CH. Improvement of an "ingel" digestion procedure for the micropreparation of internal protein fragments for amino acid sequencing. Anal Biochem 1995;224:451-455.
27. O'Farrell PH. High resolution two-dimensional electrophoresis of proteins. J Biol Chem 1975;250:4007-4021.
28. Sun HQ, Yamamoto M, Mejillano M, Yin HL. Gelsolin, a multifunctional actin regulatory protein. J Biol Chem 1999;274:33179-33182.
29. Allen PG, Janmey PA. Gelsolin displaces phalloidin from actin filaments: a new fluorescence method shows that both Ca2+ and Mg2+ affect the rate at which gelsolin severs F-actin. J Biol Chem 1994;269:32916-32923.
30. Jellum E, Thorsrud AK. High resolution two-dimensional protein electrophoresis in clinical chemistry. Scand J Clin Lab Invest Suppl 1986; 184:71-76.
31. Khaitlina S, Hinssen H. Ca-dependent binding of actin to gelsolin. FEBS Lett 2002;521:14-18.
32. Selden LA, Kinosian HJ, Newman J, Lincoln B, Hurwitz C, Gershman LC, Estes JE. Severing of F-actin by the amino-terminal half of gelsolin suggests internal cooperativity in gelsolin. Biophys J 1998;75:3092-3100.
33. Hwang IK, Park SM, Kim SY, Lee ST. A proteomic approach to identify substrates of matrix melalloproteinase-14 in human plasma. Biochim Biophys Acta 2004;1702:79-87.
34. Suzuki R, Miyazaki Y, Takagi K, Torii K, Taniguchi H. Matrix metalloproteinases in the pathogenesis of asthma and COPD: implications for therapy. Treat Respir Med 2004;3:17-27.
35. Smith DB, Janmey PA, Lind SE. Circulating actin-gelsolin complexes following oleic acid-induced lung injury. Am J Pathol 1988;130:261-267.
36. Pearlman DS. Pathophysiology of the inflammatory response. J Allergy Clin Immunol 1999;104:S132-S137.
37. Kim CK, Kim SW, Park CS, Kim BI, Kang H, Koh YY. Bronchoalveolar lavage cytokine profiles in acute asthma and acute bronchiolitis. J Allergy Clin Immunol 2003;112:64-71.
38. Walker C, Bode E, Boer L, Hansel TT, Blaser K, Virchow JC Jr. Allergic and nonallergic asthmatics have distinct patterns of T-cell activation and cytokine production in peripheral blood and bronchoalveolar lavage. Am Rev Respir Dis 1992;146:109-115.
39. Weiner DJ, Bucki R, Janmey PA. The antimicrobial activity of the cathelicidin LL37 is inhibited by F-actin bundles and restored by gelsolin. Am J Respir Cell Mol Biol 2003;28:738-745.
40. Perks B, Shute JK. DNA and actin bind and inhibit interleukin-8 function in cystic fibrosis sputa: in vitro effects of mucolytics. Am J Respir Crit Care Med 2000;162:1767-1772.
Giovanni Candiano, Maurizio Bruschi, Nicoletta Pedemonte, Emanuela Caci, Sabrina Liberatori, Luca Bini, Carlo Pellegrini, Mario Viganò, Brian J. O'Connor, Tak H. Lee, Luis J. V. Galietta, and Olga Zegarra-Moran
Laboratories of Uremic Physiopathology and Molecular Genetics, Istituto G. Gaslini, Genoa; Laboratory of Functional Proteomics, Molecular Biology Department, Università degli Studi di Siena, Siena; Cardiosurgery Section, IRCCS Policlinico San Matteo, Università degli Studi di Pavia, Pavia, Italy; and Department of Asthma, Allergy, and Respiratory Science, GKT School of Medicine, King's College London, London, United Kingdom
(Received in original form September 9, 2004; accepted in final form August 9, 2005)
Supported by a grant from the Italian Cystic Fibrosis Research Foundation. The Pediatrics Department, Università degli Studi di Cenova, has received support from Fondo per gli Investment) della Ricerca di Base (FIRB) funds.
Correspondence and requests for reprints should be addressed to Olga ZegarraMoran, M.D., Laboratorio di Genetica Molecolare, lstituto Ciannina Gaslini, L. go C. Gaslini S, Genoa-16148, Italy. E-mail: ozegarra@unige.it
This article has an online supplement, which is accessible from this issue's table of contents at www.atsjournals.org
Am J Respir Crit Care Med Vol 172. pp 1090-1096, 2005
Originally Published in Press as DOI: 10.1164/rccm.200409-1185OC on August 11, 2005
Internet address: www.atsjournals.org
Copyright American Thoracic Society Nov 1, 2005
Provided by ProQuest Information and Learning Company. All rights Reserved