Neurologic changes in a child with varicella suggest several serious complications. The differential diagnosis should include the spread of varicella to the central nervous system, adverse reaction to pharmacotherapy, or another disease entity. Several findings from the patient's history, physical examination, and laboratory results may be useful in determining the cause of the neurologic changes. Here we report such a case and the diagnostic clues that suggested diphenhydramine toxicity.
Case Presentation
A 19-month-old female child was brought to the family practice clinic by her parents. According to the parents, the child had broken out with a typical varicella rash 5 days earlier. The night before presentation at the clinic she had been restless and had difficulty going to sleep, but seemed normal otherwise. The following morning she was found playing with her older sibling when the parents arose. Two hours later she began behaving strangely. Her parents were concerned that she might be having a seizure when she began rolling her eyes back into her head.
The parents had been treating her with acetaminophen for fever and colloidal oatmeal baths for skin comfort. Caldadryl lotion had been applied to her entire body three or four times a day, after the baths. Diphenhydramine syrup had occasionally been given in varying doses, either by capful or dropperful. Two capfuls of diphenhydramine (approximately 50 mg) had been given to the child that morning, and Caladryl had been applied.
The child's past medical history was unremarkable, and her immunization status was up to date. She lived in an intact nuclear family with both parents and two siblings, the younger of whom had experienced a varicella infection 2 weeks before the patient's onset of illness.
A physical examination revealed a well-developed female child with typical varicella lesions and a film of pink chalky substance covering most of her body. Her weight was 11.5 kg (25 lb 10 oz), her pulse was 140 beats per minute, her respiratory rate was 24 breaths per minute, and her temperature was 37.3[degrees]C (99.1[degrees]F). Physical examination findings were normal except for mild cervical adenopathy, a skin rash, and neurologic abnormalities. Her skin was covered with papules, some of which were vesicular, some ulcerated, and others crusted over. During neurologic examination, the child was awake but did not interact with the examiner. She appeared moderately agitated and frightened, and would not respond to commands. She had a wide-eyed stare and exhibited occassional grimacing, tongue-chewing, and lip-smacking motions. Her pupils were widely dilated without nystagmus and sluggishly reactive to light. Choreiform movements were present intermittently, and she staggered when she walked. Deep tendon reflexes and plantar reflexes were normal, and there was no clonus present. She had on a dry diaper, possibly indicating urinary retention. A catheter was inserted, and 165 mL of urine was drained from her bladder.
Laboratory results were as follows: white blood cell count (WBC), 4.2 x [10.sub.9]/L (4200/cu mm); WBC differential, 39% neutrophils, 10 band forms; and hemoglobin 119 g/L (11.9 g/dL). Liver enzymes were within normal limits with an alkaline phosphatase level of 305 U/L, aspartate transanimase, 41 U/L; alanine transanimase, 13 U/L; and lactic dehydrogenase, 220 U/L. Cerebrospinal fluid was normal; glucose, 65 mg/dL; protein, 12 mg/dL; red blood cell count, 100/cu mm; and no WBCs. Blood and spinal fluid specimens were taken for culture and a blood sample was sent to SmithKline Bioscience Laboratory to determine diphenhydramine level.
The patient was bathed in the family practice clinic to remove the Caladryl and was then admitted to the hospital for hydration, cardiac monitoring, and observation. Over the next 24 hours the patient improved, although she became markedly somnolent. Her heart rate, pupillary size, gait, and disposition all improved, and she became more responsive to her parents' commands. She required bladder catherization again. Over the second 24-hour period the patient returned to normal except for a trace of gait instability, which later resolved. She was able to eat, drink, urinate, play, and interact normally at the time of her discharge from the hospital.
Although her blood and spinal fluid cultures were negative, her serum diphenhydramine level was subsequently reported to be 1948 ng/mL. Diphenhydramine's antihistamine effects are present at levels above 25 ng/mL, while its sedative-hypnotic effects are seen at levels above 50 ng/mL. Levels greater than 100 ng/mL may be toxic.[1]
Discussion
Indications of neurological involvement associated with varicella encephalitis may include ataxia, nystagmus, hallucinations, and unusual behavior, all of which were present in this child. However, there was no lethargy, decreased level of consciousness, or coma, as one would expect if varicella encephalitis were present. Furthermore, there were no cranial nerve abnormalities, abnormal reflexes, or papilledema to suggest encephalitis.[2] Seizures can occur in either varicella or toxic encephalopathy. Other central nervous system diseases associated with varicella infections, including Guillain-Barre syndrome and Reye's syndrome, were not suggested by the history, physical examination, or laboratory results in this case.[3]
There were, however, important physical findings that strongly suggested diphenhydramine toxicity. The child's entire body was covered with Caladryl lotion, an over-the-counter product containing 1% diphenhydramine. She had markedly dilated pupils, which reacted sluggishly to light. She also had repetitive writhing motions of her mouth, suggesting tardive dyskinesia. She was agitated and tachycardic though afebrile, and had urinary retention. These physical findings are not present with varicella encephalitis. In addition, one would expect an abnormal spinal fluid WBC count if varicella encephalitis were present.
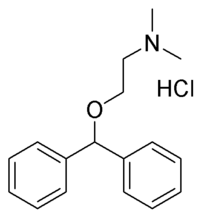
Diphenhydramine is a reversible competitive inhibitor of the action of histamine on [H.sub.1]-receptors. It is often used to treat allergic conditions and is found in many over-the-counter preparations. Anticholinergic side effects of diphenhydramine include dilated pupils, diplopia, dry mouth, flushed face, fever, urinary retention, and delirium. The drug also has sedative effects. Children more often than adults may exhibit a paradoxical excitation that is manifested by restlessness, nervousness, insomnia, seizures, hallucinations, or psychosis. Severe overdoses may result in cerebral edema, tremors, athetosis, tonic-clonic seizures, coma, cardiovascular collapse, or death.
Numerous cases of diphenhydramine toxicity in children have been reported, including several deaths.[4] It is interesting to note that the other cases of topically induced toxicity all involved treatment for varicella,[2,5-9] and most, as in this case, combined oral and topical administration of the drug. Topical application of this drug has not been associated with any deaths, even though the reported blood levels are quite high. This may reflect a relatively slow rise in serum levels of the drug as opposed to overdoses by ingesting the drug.
Once toxicity occurs, withdrawal of the drug and observation is the most acceptable treatment, with continuous ECG monitoring to detect arrhythmias. Frequent blood pressure monitoring is important to detect extreme changes. Seizures usually respond to intravenously administered diazepam, and intubation and respirator care may be necessary in some cases. Physostigmine (0.5 mg administered intravenously, slowly in children) is indicated for the treatment of severe seizures, life-threatening arrhythmias, or hypertensive crises. Physostigmine should be used only as the treatment of last resort, however, as it may itself cause respiratory collapse, arrhythmias, hypotension, and seizures.[10]
Conclusions
Varicella is a common childhood illness for which health care providers are frequently consulted. We are usually careful to warn parents not to use aspirin during this illness to avoid the development of Reye's syndrome. We should likewise caution parents to refrain from using topical diphenhydramine to avoid a serious life-threatening drug toxicity. The Caladryl label specifically warns against use in the treatment of varicella and measles except under the supervision of a physician. In fact, there is probably no role for topical diphenhydramine in the symptomatic treatment of either. Symptomatic relief can be provided by applying lotions that do not contain diphenhydramine and orally administering prescribed doses of diphenhydramine syrup, thus limiting the drug to therapeutic levels.
References
[1.] Gilman AG, Goodman LS, Rall TW, Murad F. Goodman and Gilman's The pharmacological basis of therapeutics. 7th ed. New York: Macmillan, 1985:1685.
[2.] Woodward GA, Baldassano RN. Topical diphenhydramine toxicity in a five year old with varicella. Pediatr Emerg Care 1988; 4:18-20.
[3.] Rudolph AM, Hoffman JIE, Axelrod S, eds. Pediatrics. 18th ed. Norwalk, Conn: Appleton & Lange, 1987:1685-8.
[4.] Huston RL, Cypcar D, Cheng GS, Foulds DM. Toxicity from topical administration of diphenhydramine in children. Clin Pediatr 1990; 29:542-5.
[5.] Filloux F. Toxic encephalopathy caused by topically applied diphenhydramine. J Pediatr 1986; 108:1018-20.
[6.] Tomlinson G, Helfaer M, Wiedermann BL. Diphenhydramine toxicity mimicking varicella encephalitis. Pediatr Infect Dis 1987; 6:220-1.
[7.] Patrenella R. Diphenhydramine toxicity due to topical application of Caladryl. Clin Pediatr 1986; 25:163.
[8.] Reilly JF, Weisse ME. Topically induced diphenhydramine toxicity. J Emerg Med 1990; 8:59-61.
[9.] Chan JCY, Wallander KA. Diphenhydramine toxicity in three children with varicella-zoster infection. Ann Pharmacother 1991; 25:130-2.
[10.] Mack RB. Anthistamine overdose--throw physic to the dogs. Contemp Pediatr 1990; Oct:45-57.
COPYRIGHT 1992 Dowden Health Media, Inc.
COPYRIGHT 2004 Gale Group