We reviewed the results of the use of the Dumon silicone stents in patients experiencing tuberculous tracheobronchial stenosis since 1994, using a retrospective ease review in a university teaching hospital with 1,450 beds serving a population of > 1.8 million. Between February 1994 and September 2001, seven patients with tuberculous tracheobronchial stenosis (mean age, 43 years) underwent a total of 11 dilatations with placement of 10 straight stents and 1 Y stent. Under general anesthesia, all patients underwent rigid bronchoscopy and dilatation of the stenosis with placement of a Dumon stent. There were no deaths. One patient developed a pneumothorax. Two patients experienced migration of the stent, which required reintervention for adjustment of position of the stent. The stents were left in situ for a mean period of 32 months. There was marked improvement in dyspnea in all patients after the procedure, as determined by visual analog scale. Endoscopic dilatation with placement of a silicone stent is an effective treatment for patients with tuberculous tracheobronchial stenosis.
Key words: stents; therapeutic bronchoscopy; tracheobronchial stenosis; tuberculosis
**********
The symptoms of major airway stenosis, regardless of the etiology, are always distressing. Use of a tracheobronchial stent has been established as a complementary form of management for patients with major airway stenosis. It is the procedure of choice in the palliation of airway stenosis for patients with terminal malignant disease. Since Montgomery (1) described the use of a T-tube in 1965, a variety of endotracheal stents and prostheses have been described. However, controversies still exist concerning the use of intraluminal stenting as the definitive management strategy for benign tracheobronchial stenosis.
In the West, benign stenosis of the major airway is often the result of iatrogenic airway injury, such as that occurring from prolonged intubation. (2,3) Surgical resection and appropriate reconstruction always have been the standard treatment. (4,5) The successful application of silicone stents in the management of this group of patient has been described. (6-8) In Hong Kong, endobronchial tuberculosis with airway stenosis remains a common cause of benign tracheobronchial stenosis. (9) Surgical treatment, with lung resection or complex tracheobronchoplasty, has been the established treatment for patients with airway strictures secondary to tuberculosis. (10-12)
Dumon (13) described his dedicated stent (Dumon stent; Cometh; Marseille, France) in 1990. The surface of the stent is studded to prevent its migration within the airway. In our institution, the Dumon stent has been used since 1993 for the management of patients with malignant or benign airway obstructions. There have been few reports specifically focusing on the use of this stent for patients with tuberculous tracheobronchial stenosis. A report on our experience in this area forms the basis of this paper.
MATERIALS AND METHODS
Between February 1993 and September 2001, 55 patients underwent endobronchial placement of silicone stents for major airway obstructions of both benign and malignant etiologies. Thirteen patients had benign airway stenoses, of whom 5 had iatrogenic airway injury secondary to tracheostomy or prolonged endotracheal intubation and 7 had tuberculous tracheobronchial stenoses. These seven patients (six women), who had a mean age of 43 years (range, 17 to 61 years), had both histologic and microbiological documentation of either previous or current Mycobacterium tuberculosis infection. One patient had experienced blunt chest trauma and left main bronchial injury with resulting stenosis at the site of partial transection. Another patient had relapsing polychondritis with multiple strictures within the trachea and distal bronchial tree. She received multiple tracheobronchial stenting with silicone and flexible metal stents. Of the patients with tuberculous tracheobronchial strictures, five had experienced active tuberculosis on medical therapy, while
two had a history of tuberculous infection > 5 years ago.
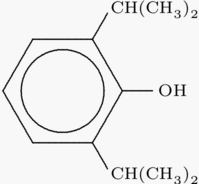
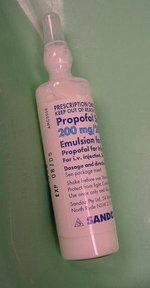
All patients underwent flexible bronchoscopy under local anesthesia for assessment of the feasibility of stenting. Patients who were found to have complete bronchial occlusion and those who had had collapsed distal airways for > 3 months were deemed unsuitable for stenting. Preoperative CT scanning of the thorax was performed in two patients with severe stenosis that could not be assessed thoroughly by flexible bronchoscopy (Fig 1). Rigid bronchoscopy was performed in the operating room under general anesthesia with either gas induction or IV propofol (Diprivan; Zeneca; Macclesfield Cheshire, UK). The patient received assisted spontaneous ventilation throughout the operation. A ventilating rigid bronchoscope (Efer-Dumon bronchoscope; La Ciolat, France) with Hopkins telescope was introduced perorally into the trachea. The telescope was connected to a three-chip camera system (model 784; Stryker; Kalamazoo, MI). The video-assisted bronchoscope was used as an optically guided endotracheal ventilation tube. A Porges dilator (Neoflex; Kaohsiung, Taiwan) was used to initiate the dilatation of the tuberculous stricture. All patients were monitored with pulse oximetry for 24 h after undergoing stenting. Chest physiotherapy was started the next day. Symptomatic improvement was assessed on a 10-point visual analog scale 48 h after the operation (0, no improvement; 10, complete relief). A repeat flexible bronchoscopy was performed 1 week after the procedure, and all patients were regularly reviewed in the outpatient clinic. Bronchoscopy will be repeated if the patient presents with any change in symptoms.
[FIGURE 1 OMITTED]
RESULTS
A total of 11 stents were placed in seven patients with tuberculous major airway stenosis. The sites of the stenosis are shown in Table 1. Five patients had left main bronchial stenosis, while two patients had stenosis of the trachea. The stents that were inserted ranged from 9 to 16 mm in diameter and 3 to 4 cm in length. There was no mortality associated with this procedure. All patients except one were discharged from the hospital on postoperative day 2. All patients experienced subjective improvement in symptoms with a mean dyspnea improvement score of 7.4 after stenting. A 20-year-old woman with very tight, left main bronchial stenosis experienced a left-sided pneumothorax after stenting. However, there was no surgical emphysema or pneumomediastinum shown on her chest radiograph. Most likely, this was a coincidental spontaneous pneumothorax, and she was treated conservatively with chest tube drainage and was discharged on postoperative day 8. The duration of in situ stent placement ranged from 1 to 74 months (mean, 28 [+ or -] 25 months). Two patients with left main bronchial stenosis experienced migration of the stents, which required adjustment of the stent position after placement. One patient presented with distal tracheal and severe right main bronchial stenosis. A 13 x 40 mm Dumon stent was placed within the distal trachea, and a 9 x 20 mm stent was put in the right mainstem bronchus (Fig 2). The patient presented again with progression of disease 5 months later. The distal tracheal stent was replaced with a 16 x 20 mm stent after dilatation, and an additional 9 x 20 mm right main bronchial stent was introduced. Despite that, the disease had progressed further 6 months later. The distal tracheal and bronchial stents then were replaced by a 14 x 10 mm Y-stent. All patients had resumed normal daily activity on follow-up. Two patients in this series (patients 1 and 2) have been reported on previously in a 1998 article (14) on our overall experience with video-assisted bronchoscopy and in another article (15) on the management of tracheobronchial obstruction.
[FIGURE 2 OMITTED]
DISCUSSION
Tuberculous tracheobronchial stenosis is uncommon in the West but is prevalent in many Asian countries. In Hong Kong, the incidence has been reported to be as high as 18% in patients with parenchymal tuberculosis. (9) Our results are compatible with those of previous studies (16) in that the predominant sex was female. It has been postulated that the caliber of the airway in women is smaller and that this results in the stasis of secretions containing the tuberculous bacilli. (10) Endobronchial tuberculosis is caused either by direct inoculation of the bacilli from the lung parenchyma or by infiltration of the airway by bacilli from adjacent mediastinal lymph nodes. (11) The left mainstem bronchus is commonly involved, as has been shown in this study. The site predilection is due to its compression by the aortic arch and the prevalence of tuberculous adenopathy on the left side. (10) Surgical resection of the stenotic area together with bronchoplastic reconstruction has been suggested by some authors (12,17,18) to be the preferred method of management. However, reanastomosis after resection has always been a concern in this group of patients with compromised pulmonary reserve and ongoing infections. Anastomotic leakage, stenosis, and respiratory failure are well-known complications. Endoluminal dilatation and stenting is an attractive alternative management strategy. Endoluminal stenting always has been looked on as a temporary measure for patients who are unfit for surgery as uncertain long-term results have been reported with the use of the Gianturco self-expanding metallic stent (19) and T-tubes. (20) Concern has been expressed about the use of metallic stents in the presence of inflammation. (21) The retrieval of a metallic stent after long-term use under benign conditions is technically difficult. (22) Dumon (13) described in 1990 the use of a silicone prosthesis, and this has gained much popularity. We have reported (14,15) on the use of the silicone stent in patients with malignant major airway obstructions with satisfactory outcomes. High efficacy and tolerance of this silicone stent in the maintenance of major airway patency have been well-documented. (23) It remains uncertain as to how long the stent could be left within the airway in order to achieve optimal results. (24) Dumon initially recommended a period of 6 to 12 months. In a study of 63 patients with benign stenosis who were treated with the silicone stent, it has been shown (6) that the stent can be well-tolerated for a period of up to 18 months without major complications. However, all the patients in this study experienced iatrogenic airway injury with resulting stenosis, and the role of bronchial stenting for the treatment of tuberculous tracheobronchial stricture was not specifically investigated. A recent series (8) showed that the silicone stent could be left in situ for 5 years without complications in patients with iatrogenic airway strictures. It remains to be seen whether tracheobronchial stenting now can be regarded as the definitive management tool for benign airway obstructions in selected patients.
The timing of intervention is controversial, and there is no way to predict which patient will develop endobronchial tuberculosis with residual strictures or when that patient will develop the condition. Five patients in our series had active tuberculous infection and developed tracheobronchial strictures with progression of disease despite intensive antituberculous therapy. Steroid therapy was once advocated for the treatment of tuberculosis, but it was later shown to be ineffective, (24) potentially causing a flare-up of the infection. Preoperative planning with three-dimensional reconstruction CT scanning and multiplanar two-dimensional images has been shown to provide a correlative map of the bronchoscopic and-surgical anatomy before invasive intervention of the airway in most instances. (25) Caution, however, is required in interpreting images that are suggestive of distal occlusion, as these may represent mucus plugging rather than true anatomic obstruction. Flexible bronchoscopy should always be performed to confirm the condition. Dilatation of the stenosis can be accomplished with the use of dilators or a balloon. (8) The bronchoscope itself can act as a form of dilator, but its use with the more rigid fibrotic benign stenosis may lead to perforation. We preferred graded dilatation with a Porges dilator under bronchoscopic guidance.
The majority of our patients spent 2 days in the hospital postoperatively. The morbidity associated with a thoracotomy can be avoided. All of the patients in our study could resume a normal life shortly after undergoing the operation. Endoluminal dilatation and bronchial stenting have now become our first-line therapy for the management of patients with tuberculous tracheobronchial strictures. However, this procedure is not without complications. Perforation and injury have been mentioned. The migration rate of the Dumon stent has been reported to be 18.6%. (26) Stent migration appears to be more common in patients with benign stenosis. (14) This may be due to the fact that the surface area for anchorage is smaller in the localized benign lesion, or it may be that the surfaces of benign lesions are smoother compared to tumor tissue, which tends to grow in between the studs of the Dumon stent. Furthermore, benign disease may regress with treatment, and the original stent may become too small for the stenosis. (14) Therefore, one should always aim to place the largest possible stent in the first instance. Nonetheless, repeated rigid bronchoscopy and repositioning of the stent are not uncommon. In our experience, repeated repositioning of the stent in patients with tuberculous strictures is not uncommon. Regular surveillance bronchoscopy and follow-up of the patient are important. Endoscopic dilatation and stenting provide an alternative and effective means of treating patients with tuberculous tracheobronchial stenoses.
REFERENCES
(1) Montgomery WW. T-tube tracheal stent. Arch Otolaryngol 1965; 82:320-321
(2) Wood DE, Mathisen DJ. Late complications of tracheotomy. Clin Chest Med 1991; 12:597-609
(3) Streitz JM, Shapshay SM. Airway injury after tracheotomy and endotracheal intubation. Surg Clin North Am 1991; 71:1211-1230
(4) Maasen W, Greschuschna D, Vogt-Moykopf I, et al. Tracheal resection: state of the art. Thorac Cardiovasc Surg 1985; 33:2-7
(5) Grillo HC, Donahue DM, Mathisen DJ, et al. Postintubation tracheal stenosis: treatment and results. J Thorac Cardiovasc Surg 1995; 109:586-593
(6) Martinez-Ballarin JI, Diaz-Jimenez JP, Castro MJ, et al. Silicone stents in the management of benign tracheobronchial stenoses: tolerance and early results in 63 patients. Chest 1996; 109:626-629
(7) Vergnon JM, Costes F, Polio JC. Efficacy and tolerance of a new silicone stent for the treatment of benign tracheal stenosis: preliminary results. Chest 2000; 118:422-426
(8) Schmidt B, Olze H, Borges AC, et al. Endotracheal balloon dilatation and stent implantation in benign stenoses. Ann Thorac Surg 2001; 71:1630-1634
(9) So SY, Lam WK, Yu DYC. Rapid diagnosis of suspected pulmonary tuberculosis by fiberoptic bronchoscopy. Tubercle 1982; 63:195-200
(10) Ozawa K, Wada S, Hirose Y, et al. Bronchial tuberculosis: a clinical study on 26 cases. Jpn J Chest Dis 1982; 40:42-44
(11) Watanabe Y, Murakami S, Oda M, et al. Treatment of bronchial stricture due to endobronchial tuberculosis. World J Surg 1997; 21:480-487
(12) Inagaki K, Yamamoto S, Fujii Y, et al. Airway reconstruction for stricture due to tracheobronchial tuberculosis. J Jpn Soc Bronchol 1994; 16:830-831
(13) Dumon JF. A dedicated tracheobronchial stent. Chest 1990; 97:328-332
(14) Yim APC, Abdullah V, Izzat MB, et al. Video-assisted interventional bronchoscopy: the Hong Kong experience. Surg Endosc 1998; 12:444-447
(15) Abdullah V, Yim APC, Wormald PJ, et al. Dumon silicone stents in obstructive tracheobronchial lesions: the Hong Kong experience. Otolaryngol Head Neck Surg 1998; 118:256-260
(16) Ip MSM, So SY, Lain WK, et al. Endobronchial tuberculosis revisited. Chest 1986; 89:727-730
(17) Yano M, Arai T, Inagaki K, et al. Functional results of sleeve lobectomy for tuberculous bronchial stenosis. J Jpn Assoc Bronchol 1995; 17:561-563
(18) Kato R, Kakizaki T, Hangai N, et al. Bronchoplastic procedures for tuberculous bronchial stenosis. J Thorac Cardiovasc Surg 1993; 106:1118-1121
(19) Hashizume T, Wantanabe M, Kawamura M, et al. A case of treatment with silicone T-tube for tracheal stenosis. J Jpn Soc Bronchol 1991; 13:182
(20) Varela A, Maynar M, Irving D. Use of Gianturco self-expandable stents in the tracheobronchial tree. Ann Thorac Surg 1990; 49:806-809
(21) Nashef S, Dromer C, Velly JF. Expanding wire stents in benign tracheobronchial disease; indications and complications. Ann Thorac Surg 1992; 52:937-940
(22) Dasgupta A, Dolmatch BL, Abi-Saleh WJ. Self-expandable metallic airway stent insertion employing flexible bronchoscope. Chest 1998; 114:106-109
(23) Diaz-Jimenez JP, Farrero M, Martinez B. Silicone stents in the management of obstructive tracheobronchial lesions: 2-year experience. J Bronchol 1994; 1:15-18
(24) Nemir RL, Cardona J, Lacoius A, et al. M. Prednisone therapy as an adjunct in the treatment of lymph node bronchial tuberculosis in childhood. Am Rev Tuberc 1963; 74:189-198
(25) LoCicero J III, Costello P, Campos C, et al. Spiral CT with multiplanar and three-dimensional reconstructions accurately predicts tracheobronchial pathology. Ann Thorac Surg 1996; 62:811-817
(26) Dumon JF, Cavaliere S, Diaz J. Seven year experience with Dumon prosthesis. J Bronchol 1996; 3:6-10
* From the Department of Surgery, The Chinese University of Hong Kong, Prince of Wales Hospital, Hong Kong SAR, China. Manuscript received November 20, 2001; revision accepted February 27, 2002.
Correspondence to: Anthony P.C. Yim, MD, FCCP, Professor and Chief, Division of Cardiothoracic Surgery, Department of Surgery, The Chinese University of Hong Kong, Prince of Wales Hospital, Shatin, New Territories, Hong Kong SAR, China; e-mail: yimap@cuhk.edu.hk
COPYRIGHT 2002 American College of Chest Physicians
COPYRIGHT 2002 Gale Group