Introduction
Psoriasis is a chronic, inflammatory skin disease characterized by thickened, silvery-scaled patches. (1) Its cause is not yet known, but numerous studies link it with inflammatory and immune mechanisms most likely associated with a genetic predisposition that can be triggered by stress. (2)
Because there is no cure for psoriasis, the multiple treatment options currently available only attempt to reduce the severity of symptoms. Non-pharmacological therapies include sunlight and stress avoidance, while pharmacological treatments are either topically applied in the form of creams or lotions, orally ingested, or injected. Most patients are treated with topical therapies sometimes combined with phototherapy and/or systemic medications.
Topical applications include:
* Anthralin--A synthetic substance made from a coal tar derivative used since the 19th century; however, it is a highly irritating substance that needs to be thoroughly washed off after each session.
* Calcipotriol--A synthetic form of vitamin [D.sub.3] that inhibits cell proliferation but may elevate serum calcium.
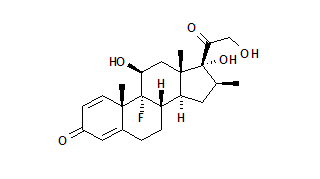
* Corticosteroid treatment--Common steroids such as Diprolene, Psorcon, Temovate, and Ultravate improve psoriatic lesions, but side effects include skin thinning, hair follicle infections, facial redness, rosacea, a worsening of diabetes mellitus, and reduced endogenous steroid production.
* Topical retinoids--Some patients experience partial clearing of psoriasis with topical retinoids, but often abandon therapy due to skin reddening and irritation.
* Topical Tacrolimus and Pimecrolimus--These topical treatments represent a new class of nonsteroidal topical immunomodulators; however, only a few studies have been performed and side effects include a burning sensation.
Oral medications are usually reserved for severe psoriasis cases because of potentially serious side effects. Among the systemic therapies associated with significant side effects are acitretin, methotrexate, cyclosporine, hydroxyurea, and thioguanine. Individuals on these medications must be closely monitored and the medications cannot be used for long-term treatment. (3) Other systemic therapies include monoclonal antibodies, (4) protein specifically targeting memory T cells, (5) fumaric acid esters, (6) novel retinoids, and macrolactams. (7) In addition to potential side effects, current oral and topical treatments are often only a partial or temporary solution.
Annual medical treatment costs for psoriasis in the United States are estimated at approximately $1.6-3.2 billion. The need exists for more effective treatment options with fewer side effects.
One such option is medical nutritional therapy. Although the American Dietetic Association promotes no specific diet for psoriasis, researchers have reported the effect on psoriasis of modifying various aspects of the diet. Strong scientific evidence exists for a gluten-free diet; (8-9) some scientific evidence exists for a vegan diet, (10) rice diet, (11) and supplementation with fish oil (12) and vitamin D; (13) and weak scientific evidence exists for a low protein diet, (14) fasting/starvation, (15) and supplementation with evening primrose oil, (16) taurine, (17) and zinc sulfate. (18-19)
Psoriasis patients showed significant improvement after six months when fed a gluten-free diet. (8) Naldi et al and Kavli et al noted in epidemiological studies that increased intake of fresh fruits and vegetables is linked with a decreased prevalence of psoriasis. (20,21) Pagano published a book for the general public (partially based on Edgar Cayce's readings) describing a diet composed primarily of fresh fruits and vegetables, with small amounts of fish, fowl, and lamb. (22)
The present study explores the effectiveness of a treatment protocol, based on Edgar Cayce's readings on psoriasis, that includes a dietary regimen, herbal supplements, and addressing intestinal permeability. Several lines of research support this systemic approach. Comorbidity studies link intestinal pathology with a variety of skin conditions, including psoriasis. (23-25)
Although there is evidence in cases of psoriasis for structural abnormalities in the intestine, (26-28) the data specifically linking intestinal permeability to psoriasis is mixed. Humbert et al compared intestinal permeability of psoriasis patients with healthy controls using the [sup.51]Cr-labeled EDTA absorption test, and found the psoriasis group had significantly increased bowel permeability. (29) On the other hand, Hamilton et al used the cellobiose/mannitol differential sugar absorption test, and although these latter researchers found an abnormal recovery ratio in seven of 29 psoriasis patients, they concluded this rate was similar to a control population. (30) The present study continues to explore this question.
The concept of increased intestinal permeability as a cause of psoriasis is based on the premise that substances from the diet larger than those normally absorbed can enter the circulation and initiate an immune system response resulting in psoriatic lesions. Until the early 20th century, "autointoxication" was widely accepted and various therapies (such as colonic irrigation) were commonly used for a variety of systemic disorders. Unsupported by scientific evidence, autointoxication tell out of favor several decades ago. (31) However, the growing body of information linking intestinal disease, excessive intestinal permeability, and systemic illness has revived the theory. (32,33) The concept of autointoxication gains support from several case studies suggesting hemodialysis and peritoneal dialysis are effective in the treatment of psoriasis. (34-37)
The conceptual basis of the present study is derived from the systems approach of Edgar Cayce, as described by Landsford and McMillin et al. In essence, the model focuses on excessive intestinal permeability (or the "leaky gut syndrome") as a primary factor in the pathogenesis of psoriasis. (38,39) According to this theory, various factors cause the walls of the small intestine to "thin" or become disturbed in some way that allows "toxic" substances to be absorbed into circulation. These substances eventually find their way into the superficial circulation and lymphatics and are eliminated through the skin, producing the plaques of psoriasis. (39) This study is based on a slightly different hypothesis, in that the current researchers suggest it is the immune system reacting to larger-than-normal substances absorbed by a compromised intestinal tract actually causing the skin to react in much the same way it does to common allergens. The approach in the present study combines the dietary treatment approach of Edgar Cayce, based on Meridian Institute publications, with evaluation of psoriasis symptoms and the measurement of intestinal permeability.
Subjects
This study was undertaken at the Meridian Institute, Virginia Beach, Virginia, involving five participants recruited by a notice in Venture Inward magazine. The criteria for inclusion included a medical diagnosis of psoriasis and the ability to travel to the clinic for required appointments; there were no exclusionary criteria. Some subjects were using treatments before and during the study (noted specifically under each case), and the protocol did not require them to change treatments. Accordingly, no one changed a previous course of treatment during the study, but simply added the study protocol. Subjects consisted of five patients diagnosed with chronic plaque psoriasis (two men and three women: mean age 52 years: range 40-68 years).
Methods and Materials
Each subject attended a 10-day, live-in program during which time bowel permeability and psoriasis symptoms were assessed by a dermatologist, and the subjects were trained to carry out the therapy protocol at home for six months. The dietary protocol included a diet rich in alkaline-forming fresh fruits and vegetables (Table 1) and daily use of saffron tea and slippery elm bark water. The raw herbs, American yellow saffron (Carthamus tinctorius) and slippery elm bark (Ulmus fulva) were packaged by and obtained from The Heritage Store, Virginia Beach, and prepared according to instructions, as follows:
* Saffron tea: 4 ounces of boiling water poured over a pinch of saffron and steeped for 15 minutes, consumed one-half hour before a meal.
* Slippery elm water: a pinch of raw herb placed in a glass of cool water, allowed to sit for five minutes, stirred, and consumed without straining.
An initial cleansing included external castor oil packs applied over the abdomen to improve elimination via the bowel, (40) colon hydrotherapy (colonic irrigations) to further assist with elimination, and spinal adjustments for each subject during the 10-day live-in program. Subjects also received instruction on maintaining regular use of castor oil packs, and were encouraged to receive further colonic irrigations and spinal adjustments (based on availability of local clinicians). Participants were advised on the importance of regular elimination and were encouraged to maintain regularity with the high fruit and vegetable diet (Table 1). Emotional counseling was also encouraged, with special emphasis on developing a positive attitude toward healing and viewing physical healing as part of a holistic process. The participants returned home, applied the protocol on a daily basis, and kept daily log sheets for six months.
Outcome Measures
The following four measurable outcomes were administered immediately before and after six months of therapy: Psoriasis Area and Severity Index (PASI) scores assessed by a medical doctor, Psoriasis Severity Scale (PSS) self-assessed by subjects, (41) before/after photograph comparisons by a medical doctor, and the lactulose/mannitol test of intestinal permeability.
The PASI standardized evaluation is a single number calculation representing severity of symptoms and area of coverage. (1) PASI scores range from 0-72, with lower scores indicating less severe symptoms and/or a smaller area of coverage. The PSS is a six-item subjective evaluation of psoriasis symptoms by the patient, (41) which is significantly correlated with objective measurement by a physician. (42) A lower score indicates less severe symptoms. The lactulose/mannitol test of intestinal permeability involves drinking a solution of two sugars; the normal bowel is relatively impermeable to lactulose, but relatively permeable to mannitol. A high lactulose/mannitol ratio in the urine indicates excess leakage of lactulose across the intestinal wall. This test is sensitive, low cost, simple to perform, and has the advantage of a simple enzyme assay. (43) It has been shown to have good repeatability and to be a reliable intestinal permeability test for sugars. (44) After an overnight fast, the participants voided a pre-test urine sample and then ingested the test solution provided by Great Smokies Laboratory (63 Zillicoa Street, Asheville, NC 28801). Urine was collected at the Meridian Institute for six hours in polyethylene bottles. Intake of at least 100 mL of water each hour was encouraged to ensure adequate urine production; food was allowed after four hours. The analysis was performed by Great Smokies Laboratory.
Results
Five participants returned for the six-month assessment and all showed improvement in PASI and PSS scores, and decreased intestinal permeability. The mean PASI score dropped from 18.2 to 8.7; the mean PSS score dropped from 14.6 to 5.4; and the mean lactulose/mannitol ratio dropped from 0.066 to 0.026. Because statistical analysis is not meaningful with five participants, each is addressed as a separate case study with the results for each participant summarized in Table 2.
Case 1
Case 1 was a 40-year-old woman exhibiting mild psoriasis on hands, elbows, and feet beginning in 1991. She used no other treatments, systemic or topical, throughout the course of the study. In the before/after pictures, Case 1 demonstrated major improvement. Her most prominent symptom--rough, red areas on her hands and elbows--were completely cleared. Psoriasis was still present on her feet. She also showed improvement on the two measures of psoriasis symptoms (Table 2). Her lactulose/mannitol ratio, which had been high (0.134) at the beginning, was normal (0.038) after six months. Regarding compliance with the protocol, Case 1 showed excellent compliance with the diet and the teas, good compliance with the colonics, and minimal compliance with the adjustments and castor oil packs.
Case 2
Case 2 was a 68-year-old man exhibiting moderate-to-severe psoriasis, initially presenting in 1985. Case 2 used no medications during the study. Photography showed large areas of reddened skin, with prominent white scaly areas. The before/after pictures of Case 2 revealed substantial healing. Most notable was the complete disappearance of the white scales on his back, although there were still large red areas. He also showed improvement on the two measures of psoriasis symptoms (Table 21). His lactulose/mannitol ratio, which had been high (0.084) at the beginning of treatment, was normal (0.022) after six months. Case 2 had excellent compliance with the diet, teas, and adjustments; good compliance with the colonics; and minimal compliance with the castor oil packs.
Case 3
Case 3 was a 47-year-old woman with moderate psoriasis beginning in 1997. She also presented with general health problems, specifically hepatitis C. She was overweight and noted her diet was poor and she craved and consumed many sweets. Case 3 used Clobetasol propionate (topical for scalp), Diprolene cream, Gingko, occasional UV light, and Allegra for allergies, both prior to and during the study. Improvement was difficult to detect in the before/after photographs. Her before photos revealed some psoriasis, while her after photos revealed no psoriasis. At the start of the study, she had moderate psoriasis over half her body, specifically her trunk and lower extremities, and slight psoriasis on the head and upper extremities. She showed substantial improvement on the two measures of psoriasis symptoms (Table 2). Her lactulose/mannitol ratio, which was in the normal range (0.034) at the onset of the study, was still normal, but lower (0.019), after six months. Case 3 also noted much improvement in her hepatitis C condition, although no medical record of the improvement was provided. Case 3 demonstrated excellent compliance with the castor oil packs; good compliance with the diet and the teas; and minimal compliance with the adjustments and colonics.
Case 4
Case 4 was a 44-year-old man, demonstrating mild psoriasis on scalp and fingers that had begun when he was five years old. He also complained of arthritis (type not specified). Prior to and during the study, Case 4 used Lipitor- for high triglycerides, Dovonex ointment, and one aspirin daily as a blood thinner. In the before/after pictures, change was difficult to perceive as his symptoms were barely visible. He showed improvement on the two measures of psoriasis symptoms (Table 2). The PASI score was zero, indicating no psoriasis symptoms at follow-up. His lactulose/mannitol ratio, which was in the normal range (0.047) at the beginning, was still normal, but lower (0.024), after six months. Case 4 maintained excellent compliance with the teas; fair compliance with the diet; and minimal compliance with the colonics, adjustments, and castor oil packs.
Case 5
Case 5 was a 59-year-old woman with severe psoriasis covering 60 percent of her body, initially presenting in 1953. Her psoriasis symptoms at the onset of the study were the most severe in the group. She also reported problems with osteoarthritis and abdominal bloating, especially at night. Case 5 reported using a steroid cream (type not specified) topically. In the before/after photographs, Case 5 had clearly visible improvement. Her most prominent symptom, red patches covering much of her back, had diminished in size and redness. She also showed improvement on the two measures of psoriasis symptoms (Table 2). Her lactulose/mannitol ratio was at the low end of the normal range (0.029) at the beginning and remained low (0.026) after six months. Regarding compliance with the protocol, Case 5 had excellent compliance with the diet, teas, and castor oil packs: and minimal compliance with the adjustments and colonics.
Discussion
The five psoriasis cases, ranging from mild to severe at the beginning of the study, improved on all measured outcomes over a six-month period when measured by the PASI criteria, the PSS, and the lactulose/mannitol test of intestinal permeability. These results suggest a treatment regimen based on Edgar Cayce's readings on diet and herbal teas or a related type of medical nutritional therapy may be an effective alternative or complementary (not exclusionary of conventional intervention) treatment for psoriasis. This study used a protocol including diet (high in fresh fruits and vegetables, small amounts of protein from fish and fowl, fiber supplements, olive oil, and avoidance of red meat, processed foods, and refined carbohydrates) and herbal teas.
Two of the five participants had abnormally high permeability; the intestinal permeability of all five decreased. The most difficult aspect of the treatment protocol for most participants was compliance with dietary restrictions. When, for various reasons such as travel, they did not adhere to the diet, the psoriasis symptoms partially returned, confirming the importance of this aspect of the treatment approach.
Psoriasis is characterized by epidermal hyperproliferation. (1) In normal skin, the cells of the epidermis continually divide and move to the surface of the skin, and are then sloughed off. This process normally takes approximately 28 days. In psoriatic skin, however, this process is accelerated and occurs in four days, with a 30-fold increase in new epidermal cells. The skin is thicker and the cells are less mature, resulting in scaling. Psoriatic skin is red and inflamed due to dilation of capillaries in the dermal layer surrounded by white blood cells. (45) The biochemical basis for the control of cell proliferation is via a delicate balance between two signaling compounds, cyclic adenosine monophosphate (cAMP) and cyclic guanosine monophosphate (cGMP). Increased levels of cAMP and decreased levels of cGMP are associated with enhanced cell maturation and reduced cell proliferation, (46) advantages in the care and management of psoriasis. Compared to unaffected skin, psoriatic plaques have been shown to contain decreased levels of cAMP and increased levels of cGMP, (46) which may contribute to epidermal hyperproliferation.
The improvement of psoriasis symptoms in all five subjects may have been due to lowering overall protein intake. Because epithelial proliferation relies on protein, reducing dietary protein may limit the potential amount of epithelial replication. Also, excess dietary protein may lead to incomplete protein digestion, leading to the formation of toxic polyamines as bowel bacteria break down the superfluous polypeptides. (47-79) Polyamines are elevated in the urine and skin of individuals with psoriasis, providing support for the concept of autointoxication. (50,51) Polyamines then inhibit the production of cAMP, leading to increased cell proliferation. (47-49) Although polyamine and cAMP levels were not measured in this study, the authors suggest that by lowering protein intake, polyamine levels in the subjects may have been reduced, resulting in higher levels of cAMP, decreased cell proliferation, and ultimately, symptom improvement.
In addition, allergic reactions often occur due to dietary proteins. If a compromised gastrointestinal tract allows protein substances larger than amino acids to pass into the bloodstream, then the body may react in an allergic-type fashion, resulting in one of the symptoms of allergies--a skin manifestation. Since allergic reactions are inflammatory responses involving the immune system, it is interesting to note psoriasis is an inflammatory condition that appears to benefit from newer immune therapies. The fact that a gluten-free diet improves the condition of some people with psoriasis (8) indicates the gastrointestinal tract may be involved.
Another important aspect of this diet was elimination of alcohol. Consumption of alcohol is a known trigger of psoriasis flare-ups. Although the mechanism is unknown, possible reasons for an alcohol trigger include stress on the liver or alcohol-induced increase in gut permeability. The fact that dialysis is effective in the treatment of psoriasis (34-37) indicates there may be substances in the blood, removed through dialysis, that can exacerbate psoriasis, such as endotoxins, immune complexes, or other substances related to the body's immune reaction. The authors believe this elusive mechanism involving the gastrointestinal tract, liver, and bloodstream holds the key to the core cause, and therefore effective treatment, for psoriasis. If this is the case, topical treatments or systemic anti-inflammatory medications are doing little to treat the cause of psoriasis. Perhaps this is why so few psoriasis treatments are successful.
Generous consumption of fresh fruits and vegetables was also a significant feature of the diet of the test subjects. The resulting boost in consumption of fiber may have aided in diminishing psoriasis symptoms. Both bacteria and yeasts inhabit the bowels and produce byproducts that may be carried away by fiber components (52) for elimination. Further hypothesizing the autointoxication theory, some of these byproducts from the intestine, such as endotoxins, may enter the systemic circulation due to intestinal hyperpermeability, leading to higher skin cGMP levels and the resulting rapid skin cell proliferation seen in psoriatics. (52) By increasing daily fiber intake it is possible to decrease the absorption of endotoxins, which could reduce cGMP levels in skin. Some researchers suggest a high-fiber, vegetarian diet also supports a healthy balance of normal intestinal microflora. Conversely, a diet high in animal protein encourages the growth of the microorganisms that produce endotoxins. (53,54)
Another aspect of diet that has been researched among psoriasis patients is the use of omega-3 fatty acid supplementation. Overall, fish oil consumption results in mild-to-modest improvement in psoriatic symptoms, (66,55-57) although some studies show fish oil was not superior to corn oil (58) or olive oil. (59) Psoriatic plaques have been shown to increase arachidonic acid and leukotriene levels (60) compared to normal skin. Arachidonic acid is an omega-6 fatty acid contained in animal products that, when metabolized, produces potent inflammatory leukotrienes. Leukotrienes are promoters of increased cGMP levels. (16,60) On the other hand, eicosapentaenoic acid (EPA), one of the active components offish oil, serves as a substrate for the production of anti-inflammatory prostaglandins. (61) In most of the studies employing fish oil supplementation, the diets of the subjects involved were not altered (55,57,62) and results have shown only slight improvement. This may have been due to the fact that study subjects continued to eat red meat; hence, arachidonic acid was in competition with the EPA. In the present study, however, all meat from sources other than fish, fowl, and lamb were excluded. Although arachidonic acid levels were not measured in this study, decreasing the intake of red meat and therefore arachidonic acid, and substituting protein from fish, consequently increasing EPA levels, may have contributed to decreased levels of leukotrienes, cGMP, and cellular proliferation.
Supplementation with certain herbal teas can improve inflammatory conditions. Yellow saffron (Carthamus tinctorius) has been shown to possess anti-inflammatory (63,64) and immune-modulating properties). (65) Slippery elm (Ulmus fulva) is an herb used traditionally for digestive difficulties, stomach and intestinal ulcers, and colitis. It is a demulcent, high in mucilage, noted for its ability to soothe or protect irritated mucous membranes, and perhaps acts as an inflammatory agent. (66)
In all five cases in this study, intestinal permeability improved during the course of treatment according to the lactulose/mannitol test (Table 2). However, interpretation of the role of permeability is complicated by the fact that in only two cases was initial permeability outside the norms provided by the testing laboratory. It is possible the dietary regimen employed in this study reduced intestinal permeability to previously present dietary compounds, despite the fact permeability was in the normal range in several cases. Further research could be directed toward analysis of skin cAMP, cGMP, and polyamine levels, as well as intestinal permeability in response to the Edgar Cayce diet.
These preliminary results are interesting and further research is warranted in order to determine if diet can truly play a significant role in the observed reduction of psoriatic symptoms. The study should employ a specific "psoriasis diet" combined with a diet diary prior, during, and after the study to ensure compliance and to allow dietary analysis of total nutrients. Measurable outcomes should be evaluated again four weeks after the diet's cessation to determine the frequency and severity of relapse.
References
(1.) Feldman SR. A quantitative definition of severe psoriasis for use in clinical trials. J Dermatolog Treat 2004;15:27-29.
(2.) Zachariae R, Zachariae H, Blomqvist K, et al. Self-reported stress reactivity and psoriasis-related stress of Nordic psoriasis sufferers. J Eur Acad Dermatol Venereol 2004;18:27-36.
(3.) Tristani-Firouzi P, Krueger GG. Efficacy and safety of treatment modalities for psoriasis. Cutis 1998;61:11-21.
(4.) Vincek V, Jacob SE, Nassiri M, et al. Infliximab monotherapy in psoriasis: a case of rapid clinical and histological response. Int J Dermatol 2004;43:303-308.
(5.) Ortonne JP, Prinz JC. Alefacept: a novel and selective biologic agent for the treatment of chronic plaque psoriasis. Eur J Dermatol 2004;14:41-45.
(6.) Balasubramaniam P, Stevenson O, Berth-Jones J. Fumaric acid esters in severe psoriasis, including experience of use in combination with other systemic modalites. Br J Dermatol 2004;150:741-746.
(7.) Singe F, Weinberg JM. Oral tazarotene and oral pimecrolimus: novel oral therapies in development for psoriasis. J Drugs Dermatol 2004;3:141-143.
(8.) Michaelsson G, Gerden B, Hagforsen E, et al. Psoriasis patients with antibodies to gliadin can be improved by a gluten-free diet. Br J Dermatol 2000; 142:44-51.
(9.) de Vos RJ, de Boer WA, Haas FD. Is there a relationship between psoriasis and coeliac disease? J Intern Med 1995;237:118.
(10.) Lithell H, Bruce A, Gustafsson IB, et al. A fasting and vegetarian diet treatment trial on chronic inflammatory disorders. Acre Derm Venereol 1983;63:397-403.
(11.) Newborg B. Disappearance of psoriatic lesions on the Rice Diet. N C Med J 1986;47:253-255.
(12.) Kojima T, Terano T, Tanabe E, et al. Long-term administration of highly purified eicosapentaenoic acid provides improvement of psoriasis. Dermatologica 1991;182:225-230.
(13.) Perez A, Chen TC, Turner A, et al. Efficacy and safety of topical calcitriol (1,25-dihydroxyvitamin D3) for the treatment of psoriasis. Br J Dermatol 1996;134:238-246.
(14.) Portnoy B. Psoriasis treated with low tryptophan diet. Br J Dermatol 1969;81:389.
(15.) Soter NA, Wilkinson DS, Fitzpatrick TB. Clinical dermatology (third of three parts). N Engl J Med 1973;289:296-302.
(16.) Kragballe K, Fogh K. A low-fat diet supplemented with dietary fish oil (Max-EPA) results in improvement of psoriasis and in formation of leukotriene B5. Acta Derm Venereol 1989;69:23-28.
(17.) Roe DA. Nutrient requirements in psoriasis. N Y State J Med 1965;65:1319-1326.
(18.) Clemmensen OJ, Siggaard-Andersen J, Worm AM, et al. Psoriatic arthritis treated with oral zinc sulphate. Br J Dermatol 1980;103:411-415.
(19.) Parodi A, Priano L, Rebora A. Chronic zinc deficiency in a patient with psoriasis and alcoholic liver cirrhosis. Int J Dermatol 1991;30:45-47.
(20.) Naldi L, Parazzini F, Peli L, et al. Dietary factors and the risk of psoriasis. Results of an Italian case-control study. Br J Dermatol 1996;134:101-106.
(21.) Kavli G, Forde OH, Arnesen E, Stenvold SE. Psoriasis: familial predisposition and environmental factors. Br Med J (Clin Res Ed) 1985;291:999-1000.
(22.) Pagano J. Healing Psoriasis: The Natural Alternative. Englewood Cliffs, NJ: The Pagano Organization, Inc.; 1991.
(23.) D'Amico E, Palazzi C, Capani F. Remission of psoriatic arthritis alter porto-caval anastomosis in a patient with primary biliary cirrhosis. J Rheumatol 1999;26:236.
(24.) Menzel I, Holzmann H. Reflections on seborrheic scalp eczema and psoriasis capillitii in relation to intestinal mycoses. Z Hautkr 1986;61:451-454. [Article in German]
(25.) Yates VM, Watkinson G, Kelman A. Further evidence for an association between psoriasis, Crohn's disease and ulcerative colitis. Br J Dermatol 1982;106:323-330.
(26.) Barry RE, Salmon PR, Read AE, Warin RP. Mucosal architecture of the small bowel in cases of psoriasis. Gut 1971;12:873-877.
(27.) Michaelsson G, Kraaz W, Gerden B, et al. Increased lymphocyte infiltration in duodenal mucosa from patients with psoriasis and serum IgA antibodies to gliadin. Br J Dermatol 1995;133:896-904.
(28.) Michaelsson G, Kraaz W, Hagforsen E, et al. Psoriasis patients have highly increased numbers of tryptase-positive mast cells in the duodenal stroma. Br J Dermatol 1997;136:866-870.
(29.) Humbert P, Bidet A, Treffel P, et al. Intestinal permeability in patients with psoriasis. J Dermatol Sci 1991;2:324-326.
(30.) Hamilton I, Fairris GM, Rothwell J, et al. Small intestinal permeability in dermatological disease. QJ Med 1985;56:559-567.
(31.) Ernst E. Colonic irrigation and the theory of autointoxication: a triumph of ignorance over science. J Clin Gastroenterol 1997;24:196-198.
(32.) Swank GM, Deitch EA. Role of the gut in multiple organ failure: bacterial translocation and permeability changes. World J Surg 1996;20:411-417.
(33.) Person JR, Bernhard JD. Autointoxication revisited. J Am Acad Dermatol 1986;15:559-563.
(34.) Glinski W, Jablonska S, Imiela J, et al. Continuous peritoneal dialysis for treatment of psoriasis. I. Depletion of PMNL as a possible factor for clearing of psoriatic lesions. Arch Dermatol Res 1979;265:337-341.
(35.) McEvoy J, Kelly AM. Psoriatic clearance during haemodialysis. Ulster Med J 1976;45:76-78.
(36.) Muston HL, Conceicao S. Remission of psoriasis during haemodialysis. Br Med J 1978;1:480-481.
(37.) Twardowski ZJ. Abatement of psoriasis and repeated dialysis. Ann Intern Med 1977;86:509-510.
(38.) Landsford FD. Psoriasis. In: McGarey WA, ed. Physicians Reference Notebook. Virginia Beach, VA: A.R.E. Press: 1983:303-309.
(39.) Mcmillin DL, Richards DG, Mein EA, Nelson CD. Systemic aspects of psoriasis. An integrative model based on intestinal etiology. Integr Med 2000;2:105-113.
(40.) Mein E. Keys to Health. New York, NY: Harper & Row Publishers, Inc.; 1989.
(41.) Gottlieb AB, Kang S, Linden KG, et al. Evaluation of safety and clinical activity of multiple doses of the anti-CD80 monoclonal antibody, galiximab, in patients with moderate to severe plaque psoriasis. Clin Immunol 2004;111:28-37.
(42.) McHenry PM, Doherty VR. Psoriasis: an audit of patients' views on the disease and its treatment. Br J Dermatol 1992:127:13-17.
(43.) Juby LD, Rothwell J, Axon AT. Lactulose/ mannitol test: an ideal screen for celiac disease. Gastroenterology 1989;96:79-85.
(44.) van Elburg RM, Uil JJ, Kokke FT, et al. Repeatability of the sugar-absorption test, using lactulose and mannitol, for measuring intestinal permeability for sugars. J Pediatr Gastroenterol Nutr 1995;20:184-188.
(45.) Klaber M. Common Skin Conditions in General Practice. Surrey, United Kingdom: Reed Business Publishing; 1991.
(46.) Voorhees JJ, Duell EA. Imbalanced cyclic AMP-cyclic GMP levels in psoriasis. Adv Cyclic Nucleotide Res 1975;5:735-758.
(47.) Proctor MS, Wilkinson DI, Orenberg EK, Farber EM. Lowered cutaneous and urinary levels of polyamines with clinical improvement in treated psoriasis. Arch Dermatol 1979;115:945-949.
(48.) Voorhees JJ. Polyamines and psoriasis. Arch Dermatol 1979;115:943-944.
(49.) McDonald CJ. Polyamines in psoriasis. J Invest Dermatol 1983;81:385-387.
(50.) Kaplan RP, Russell DH, Lowe NJ. Etretinate therapy for psoriasis: clinical responses, remission times, epidermal DNA and polyamine responses. J Am Acad Dermatol 1983;8:95-102.
(51.) Grekin RC, Ellis CN, Goldstein NG, et al. Decreased urinary polyamines in patients with psoriasis treated with etretinate. J Invest Dermatol 1983;80:181-184.
(52.) Rosenberg EW, Belew PW. Microbial factors in psoriasis. Arch Dermatol 1982;118:143-144.
(53.) Hao WL, Lee YK. Microflora of the gastrointestinal tract: a review. Methods Mol Biol 2004;268:491-502.
(54.) Kidd PM. Multiple sclerosis, an autoimmune inflammatory disease: prospects for its integrative management. Altern Med Rev 2001;6:540-566.
(55.) Bittiner SB, Tucker WF, Cartwright I, Bleehen SS. A double-blind, randomised, placebo-controlled trial of fish oil in psoriasis. Lancet 1988;1:378-380.
(56.) Collier PM, Payne CR. The dietary effect of oily fish consumption on psoriasis. Br J Dermatol 1996;135:858.
(57.) Maurice PD, Allen BR, Barkley AS, et al. The effects of dietary supplementation with fish oil in patients with psoriasis. Br J Dermatol 1987;117:599-606.
(58.) Soyland E, Funk J, Rajka G, et al. Dietary supplementation with very long-chain n-3 fatty acids in patients with atopic dermatitis. A double-blind multicentre study. Br J Dermatol 1994;130:757-764.
(59.) Bjorneboe A, Smith AK, Bjorneboe GE, et al. Effect of dietary supplementation with n-3 fatty acids on clinical manifestations of psoriasis. Br J Dermatol 1988;118:77-83.
(60.) Voorhees JJ. Leukotrienes and other lipoxygenase products in the pathogenesis and therapy of psoriasis and other dermatoses. Arch Dermatol 1983;119:541-547.
(61.) Adam O. Dietary fatty acids and immune reactions in synovial tissue. Eur J Med Res 2003;8:381-387.
(62.) Grimminger F, Mayser P, Papavassilis C, et al. A double-blind, randomized, placebo-controlled trial of n-3 fatty acid based lipid infusion in acute, extended guttate psoriasis. Rapid improvement of clinical manifestations and changes in neutrophil leukotriene profile. Clin Investig 1993;71:634-643.
(63.) Xu SX. Anti-inflammatory active constituents of Carthamus tinctorius (2). Zhong Yao Tong Bao 1986;11:42-44. [Article in Chinese]
(64.) Akihisa T, Yasukawa K, Oinuma H, et al. Triterpene alcohols from the flowers of Compositae and their anti-inflammatory effects. Phytochemistry 1996;43:1255-1260.
(65.) Lu ZW, Liu F, Hu J, et al. Suppressive effects of safflower yellow on immune functions. Zhongguo Yao Li Xue Bao 1991;12:537-542.
(66.) Langmead L, Dawson C, Hawkins C, et al. Antioxidant effects of herbal therapies used by patients with inflammatory bowel disease: an in vitro study. Aliment Pharmacol Ther 2002;16:197-205.
Amy C. Brown, PhD, RD--Assistant Professor of Human Nutrition, Department of Human Nutrition, Food & Animal Sciences, University of Hawaii at Manoa Correspondence address: Department of Human Nutrition, Food & Animal Sciences, University of Hawaii at Manoa, 1955 East West Road, Rm 216, Honolulu, HI 96822 Email: amybrown@hawaii.edu
Michelle Hairfield Stein, PhD--Senior Researcher, Tissue Genesis Incorporated, Honolulul, HI
Douglas G. Richards, PhD--Director of Research, Meridian Institute, Virginia Beach, VA
David L. McMillin, MA--Clinical Researcher, Meridian Institute, Virginia Beach, VA
Eric A. Mein, MD--Clinical Researcher, Meridian Institute, Virginia Beach, VA
Carl D. Nelson, DD--Clinical Researcher, Meridian Institute, Virginia Beach, VA
COPYRIGHT 2004 Thorne Research Inc.
COPYRIGHT 2004 Gale Group