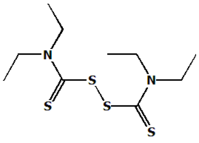
For nearly 50 years, many thousands of alcoholics worldwide have used disulfiram (Antabuse) as a part of their sobriety programs.(1) Up to 200,000 alcoholics in the United States take disulfiram regularly.(2) This article reviews the history, clinical use and side effects of this agent.
History
Disulfiram (tetraethylthiuram disulfide; TETD) was used in the rubber industry in the early part of the 20th century. In 1937, an American physician working in a chemical plant reported that workers exposed to TETD could not drink alcohol without developing a reaction consisting of flushing of the face, tachycardia and hypotension.(3) He suggested then that TETD might be useful in the treatment of alcoholism, but his suggestion was ignored.
In 1947, Hald and jacobsen (4) made a serendipitous discovery. They experimented with TETD as an anthelmintic, knowing that it could chelate the copper ion in the respiratory enzyme of lower life forms. The two took TETD themselves to investigate possible ill effects on humans and found that they both became ill after drinking alcohol. They concluded that TETD had somehow altered the metabolism of alcohol. Within a short time, disulfiram was being used by physicians to treat alcoholism.
In the early 1950s, it was customary to administer very large doses of disulfiram, as much as 3,000 mg daily for one or two weeks, to patients who were attempting to stop drinking. It was considered necessary for all patients to experience a disulfiram-ethanol reaction. Since the severity of the reaction is directly related to the amounts of alcohol and disulfiram ingested, the early high dosages of disulfiram resulted in severe reactions. These effects dampened enthusiasm for disulfiram use. Since 1960, however, the maximum recommended dosage of disulfiram has been 500 mg daily. The more commonly used dosage is 250 mg daily. The purposeful disulfiram-ethanol reaction "test" has been all but abandoned. Clinical Use of Disulfiram
Treatment for alcoholism can begin only after drinking stops and detoxification is complete. After that, an additional period of sobriety is necessary to restore cognitive skills to the point that realistic thinking is possible.(5,6) Disulfiram can help patients achieve this period of sobriety. We recommend that disulfiram be taken for at least one year after the initiation of rehabilitation, preferably under the supervision of a business associate or an interested and objective family member.
Disulfiram tablets should be crushed in water and taken with a water "chaser." Ideally, the first dose of disulfiram should be taken in the physician's off ice, at least 12 hours after the last drink. Taking the first dose in the physician's office avoids the temptation for another "last drink."(7)
Regular attendance at Alcoholics Anonymous meetings is mandatory during disulfiram therapy; Al-Anon, Alateen, Alatot and family therapy are essential supportive elements, in addition to individual counseling for the alcoholic. Indications for disulfiram treatment are listed in Table 1.( 7)
SIDE EFFECTS
The incidence of adverse reactions to disulfiram is low; there have been comparatively few reports of toxicity despite millions of disulfiram doses taken worldwide since 1948. Only the more frequent and serious side effects are discussed here; discussion of the other side effects may be found elsewhere.(1) Table2 lists the adverse reactions to disulfiram that have been reported more than five times to the U.S.
Food and Drug Administration.
Somnolence is probably the most common side effect. Drowsiness occurs at the beginning of treatment in up to 5 percent of patients taking disulfiram. It may last 10 to 14 days but is rarely incapacitating. If drowsiness persists or is severe, the dosage may be reduced by 50 percent for two weeks; the regular dosage can then be restored. This strategy can also be used for other side effects, such as asthenia, dyspnea, sweating, taste perversion, vasodilatation, impotence, amblyopia, dizziness, ataxia, hypertension and neurologic symptoms. Disulfiram should be immediately discontinued at the first sign of hepatitis or liver function abnormality.
Phenytoin (Dilantin) toxicity is possible in patients receiving disulfiram. Some patients taking phenytoin can tolerate disulfiram in a half dosage (250 mg three times a week). Occasional patients tolerate regular dosages of both drugs. The correct balance must be determined by close monitoring of the serum phenytoin level while carefully titrating the disulfiram dosage. Beginning Disulfiram Treatment
Initially, all patients must be fully informed about the disulfiram-ethanol reaction. Figure 1 is a sample of an informed consent document that should be used for this purpose. After consent is obtained, pretreatment screening should include a complete physical examination, urinalysis, complete,blood count, serology, SMA-12 profile, electrolyte determination, electrocardiogram, psychosocial history and psychiatric evaluation. Disulfiram therapy should not begin until the laboratory data are within normal limits or nearly so.
After pretreatment screening is complete, disulfiram therapy is begun at 250 mg daily for five days, then increased to 500 mg three times per week for at least one year, during which time the patient must participate in Alcoholics Anonymous, counseling and family therapy, and must learn to live without alcohol.
The SMA-12 should be repeated after one to two weeks of disulfiram therapy, and then periodically. If signs of liver dysfunction occur, disulfiram should be discontinued, and liver function should be watched carefully until it returns to normal.
Metronidazole (Flagyl) has been recommended for patients with contraindications to disulfiram, such as severe myocardial or coronary artery disease, psychosis or hypersensitivity to disulfiram. Relative contraindications include pregnancy, significant cerebral damage or the inability to comprehend the need to avoid alcohol while taking disulfiram.
The dosage of metronidazole is 250 mg daily for five days, then 250 mg three times per week. The side effects of metronidazole are similar to those of disulfiram, but the metronidazole-ahanol reaction is usually less severe than the disulfiram-ethanol reaction. There are some reports of the metronidazole-ethanol interaction being abused for the sake of the "rush" it provides.(8,9)
Treatment of Disulfiram-Ethanol Reaction
The general message conveyed by the literature is that treatment of the disulfiram-ethanol reaction with ascorbic acid is ineffective. In our experience, however, ascorbic acid alone has never failed to promptly resolve a mild disulfiram-ethanol reaction. Mild cases include those in which the pulse rate does not exceed 100 per minute and the patient's general condition is good. Such patients can be given 1 g of ascorbic acid orally. Mild cases of disulfiram-ethanol reaction usually resolve in 30 to 45 minutes.
Patients with moderately severe disulfiram-ethanol reactions have pulse rates between 100 and 150 per minute and blood pressure elevation (up to 150/100 mm Hg). In our experience, ascorbic acid, 1 g intravenously, resolves the disulfiram-ethanol reaction in two to five minutes, without residual effects.
In addition to the ascorbic acid, diphenhyclramine (Benadryl), 50 to 100 mg intravenously,(7) or chlordiazepoxide (Librium), barbiturates or spironolactone (Aldactone) are also options.(10)
Disulfiram and the Family
Because alcoholism is a family disease, all family members should be involved in treatment whenever possible. Alcoholics Anonymous must be a part of all sobriety programs, with the addition of Al-Anon, Alateen and Alatot. Disulfiram works best as part of alcoholism treatment if a person who is significant to the patient closely monitors the disulfiram ingestion. This supervision should continue until the alcoholic has remained sober for at least one year. At this point the patient can assume total responsibility for taking the drug.
After the year of disulfiram therapy is completed, the patient should continue to keep disulfiram on hand as an "insurance policy" against taking that critical first drink when a life crisis arises. In a crisis situation, disulfiram (or metronidazole) therapy should be started immediately and continued until the crisis resolves.
REFERENCES
1. McNichol RW, Ewing JA, Faiman MD. Disulfiram
Antabuse): a unique medical aid to
sobriety. Springfield, Ill.: Thomas, 1987.
2 .Mendelson JH, Mello NK, eds. The diagnosis
and treatment of alcoholism. New York: Mc - Graw-Hill, 1979:204.
3. Williams EE. Effects of alcohol on workers
with carbon disulfide. JAMA 1937; 109:1472.
4. Hald J, Jacobsen E. A drug sensitizing the
organism to ethyl alcohol. Lancet 1948;2:
1001-4.
5. DeFranco C, Tarbox AR, McLaughlin EJ.
Cognitive deficits as a function of years of
alcohol abuse. Am J Drug Alcohol Abuse
1985;11:279-93.
6. Yohman JR, Parsons OA, Leber WR. Lack of
recovery in male alcoholics' neuropsychological
performance one year after treatment.
Alcoholism 1985;9:114-7.
7. Zuska JJ, Pursch JA. Long-term management.
In: Gitlow SE, Peyser HS, eds. Alcoholism, a
practical treatment guide. New York: Grune
& Stratton, 1980:138-65.
8. Seinson RP. Long term trial of metronidazole
in male alcoholics. Br J Psychiatry 1971;119:
85-9.
9. Goodwin DW. Metronidazole in the treatment
of alcoholism: a negative report. Am J
Psychiatry 1967;123:1276-8.
10. Beyeler C, Fisch HU, Preisig R. The disulfiram-alcohol
reaction: factors determining and
potential tests predicting severity. Alcoholism
1985;9:118-24.
COPYRIGHT 1991 American Academy of Family Physicians
COPYRIGHT 2004 Gale Group