To the Editor:
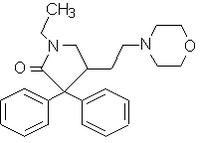
Evidence suggests the relationship between the perceptibility of dyspnea and the hypoxic ventilatory response. (1,2) Doxapram, a potent ventilatory stimulant, is known to affect primarily the hypoxic ventilatory response by acting on peripheral chemoreceptors. (3) Although the ventilatory effect of doxapram has been investigated, (4,5) the effect of doxapram on the sensation of dyspnea has not been investigated. Therefore, we investigated the effect of doxapram on the perception of dyspnea during inspiratory resistive loading.
Hypoxic ventilatory response and perception of dyspnea during inspiratory resistive load (20.0 cm [H.sub.2]O/L/s and 30.9 cm [H.sub.2]O/L/s) was measured using the rebreathing circuit with a Validyne pressure transducer (Validyne Engineering; Northridge, CA) as previously described (1) in seven healthy male volunteers (age range, 26 to 46 years) who did not know the purpose of the study. (1) All subjects were previously measured without doxapram administration. The experiment was performed in a single-blind fashion; however, in each case, doxapram was administered after saline solution placebo in order to avoid the residual effects of the drug. Measurements of dyspnea and the hypoxic response were started after a 15-min placebo infusion via a forearm vein at the rate of 10 mL/h and after the ventilation rate became stable. Following the completion of the measurements with placebo treatment, the infusion was stopped for i h as a resting period, and then doxapram diluted in saline solution was infused in the same manner as placebo at the rate of 2.0 mg/kg/h. The measurements were started 15 min after the doxapram infusion because 15 min is required to stabilize the serum doxapram concentration. (5)
All subjects completed the experiments without any side effects. Ventilatory parameters such as minute ventilation (VE), frequency, tidal volume, mouth pressure 0.1 s after the start of inspiration against occluded airway ([P.sub.0.1]), peak inspiratory mouth pressure, and arterial oxygen saturation (Sp[O.sub.2]) during stable ventilation were not significantly different between placebo and doxapram infusion. The end-tidal tension of carbon dioxide was significantly lower during doxapram infusion than placebo infusion. The hypoxic ventilatory responses expressed in the VE slope ([DELTA]VE/[DELTA]Sp[O.sub.2]) and the [P.sub.0.1] slope ([DELTA]Sp[O.sub.2]) were significantly increased during doxapram infusion (p < 0.05 for both by paired t test; Fig 1). The Borg scores of individual subjects during breathing with resistances of 20.0 cm [H.sub.2]O/L/s and 30.9 cm [H.sub.2]O/L/s also significantly increased during doxapram infusion (p < 0.01 and p < 0.05, respectively, by paired t test).
[FIGURE 1 OMITTED]
These results showed that doxapram administration augments the dyspnea sensation as well as the hypoxic ventilatory response. Although we could not clarify the mechanisms by which doxapram augments the perception of dyspnea with resistive load, our finding provides some clinical implications. Since doxapram is occasionally used for the treatment of patients with respiratory failure, one should be aware that this drug possibly increases dyspnea. However, it has been reported that the blunted perception of dyspnea as well as lowered hypoxic chemosensitivity play a role in some pathologic conditions such as death from asthma and respiratory failure in Parkinson disease. (1,2) Because doxapram can improve both dyspnea sensation and hypoxic chemosensitivity, it is of interest to investigate the effect of a drug like doxapram on these patients.
Correspondence to: Satoru Ebihara, MD, PhD, Department of Geriatric and Respiratory Medicine, Tohoku University School of Medicine, Seiryo-machi 1-1, Aoba-ku, Sendai 980-8574, Japan; e-mail: dept@geriat.med.tohoku.ac.jp
REFERENCES
(1) Kikuchi Y, Okabe S, Tamura G, et al. Chemosensitivity and perception of dyspnea in patients with a history of near-fatal asthma. N Engl J Med 1994; 330:1329-1334
(2) Onodera H, Okabe S, Kikuchi Y, et al. Impaired chemosensitivity and perception of dyspnea in Parkinson's disease. Lancet 2000; 356:739-740
(3) Mitchell RA, Herbert DA. Potencies of doxapram and hypoxia in stimulating carotid-body chemoreceptors and ventilation in anesthetized cats. Anesthesiology 1975; 42: 559-566
(4) Burki NK. Ventilatory effects of doxapram in conscious human subjects. Chest 1984; 85:600-604
(5) Calverley PMA, Robson RH, Wraith PK, et al. The ventilatory effects of doxapram in normal man. Clin Sci 1983; 65:65-69
COPYRIGHT 2002 American College of Chest Physicians
COPYRIGHT 2002 Gale Group