Study objective: To determine if the administration of systemic corticosteroids diminishes the effectiveness of the pleurodesis induced by the intrapleural injection of doxycycline.
Study design: Thirty New Zealand white male rabbits were classified into three groups (n = 10 rabbits), all of which received doxycycline, 10 mg/kg intrapleurally, in a volume of 2 mL. Rabbits in the control group received only the intrapleural injection of doxycycline; the steroid-once group received triamcinolone, 0.8 mg/kg IM, 24 h before the intrapleural injection; and the steroid-weekly group received triamcinolone, 0.8 mg/kg IM, 24 h before the intrapleural injection and weekly over the next 3 weeks. All rabbits had a chest tube placed before the intrapleural administration of doxycycline and underwent pleural fluid aspiration twice daily. The rabbits were killed after 28 days, and the pleura and lungs were examined macroscopically and microscopically.
Results: The administration of corticosteroids resulted in both a significant decrease in the macroscopic adhesion score (p < 0.001) and a tendency toward a decreased microscopic fibrosis score (p = 0.056) after 28 days. Animals receiving weekly corticosteroid injections had lower scores than animals receiving only one injection.
Conclusion: This study demonstrates that the administration of corticosteroids (triamcinolone, 0.8 mg/kg) 24 h before the intrapleural injection of doxycycline, 10 mg/kg, decreases the effectiveness of pleurodesis in rabbits. Weekly injections decreased the effectiveness even more. If these results can be extrapolated to humans, efforts should be made to minimize the administration of exogenous corticosteroids when pleurodesis is attempted. (CHEST 2002; 121:216-219)
Key words: corticosteroids; doxycycline; pleural effusion; pleurodesis
**********
Pleurodesis is frequently considered for the management of recurrent pneumothoraces or pleural effusions. The pleurodesis is produced by the intrapleural injection of a sclerosing agent that induces an inflammatory response leading to a fibrotic process that fuses the parietal and visceral pleura, and obliterates the pleural space. (1)
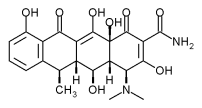
Corticosteroids are drugs known for their anti-inflammatory properties. A significant percentage of patients who are candidates for pleurodesis may be receiving corticosteroids at the time that pleurodesis is attempted. (2) We have shown previously (3) that when pleurodesis is induced in rabbits with talc slurry, the concomitant use of corticosteroids decreases the initial inflammatory process and diminishes the efficacy of the pleurodesis. The mechanisms of pleurodesis are largely unknown but are likely different for talc slurry and doxycycline, the two most commonly employed agents. This is supported by a recent report (4) demonstrating that blocking antibodies to tumor necrosis factor-[alpha] diminish the pleurodesis resulting from tale but not that from doxycycline.
The objective of this study was to evaluate the effect of corticosteroids on the pleurodesis induced by doxycycline in rabbits. We hypothesized that the pleurodesis would be less effective in rabbits receiving corticosteroids.
MATERIALS AND METHODS
The protocol was approved by the animal care committees of the Veterans Administration Medical Center, Long Beach, CA, and Vanderbilt University, Nashville, TN. The protocol utilized for the present study was similar to that used previously. (5,6) Thirty New Zealand white male rabbits weighing 2.0 to 3.0 kg were classified into three groups (10 animals in each group). The first group (control group) did not receive corticosteroids. The second group (steroid-once group) received one injection of triamcinolone, 0.8 mg/kg IM, 24 h before the intrapleural injection. The third group (steroid-weekly group) received triamcinolone, 0.8 mg/kg IM, 24 h before the pleural injection and then weekly for the duration of the study. All rabbits received doxycycline, 10 mg/kg, injected intrapleurally through the chest tube.
Prior to doxycycline administration, the rabbits were anesthetized with ketamine hydrochloride, 35 mg/kg, and xylazine hydrochloride, 5 mg/kg IM. The thorax was prepared for aseptic surgery by shaving the right chest wall and then sterilizing it with alcohol. A 0.5-cm skin incision was made over the right anterior chest wall. The muscles in the fifth or sixth intercostal spaces were bluntly dissected to expose the parietal pleura. Then, a small chest tube (16F) connected to a three-way stopcock was inserted into the pleural space; all air was aspirated from the pleural space, and doxycycline solution, 10 mg/kg, was injected. The tube was secured in place with a purse-string suture and was attached to a Heimlich valve with a three-way stopcock inline between the chest tube and the valve. The rabbits were fitted with a special vest to which the chest tubes were attached. (5,6)
After the doxycycline was injected, the chest tube was flushed with a small amount of saline solution and closed via the stopcock for the following 2 h. Then the stopcock was opened, allowing the fluid to drain spontaneously and continuously through the Heimlich valve. In addition, the chest tube was aspirated twice daily. The chest tube was left in place for at least 3 days. If the amount of pleural fluid aspirated was > 1 mL, the chest tube was left in place for a maximum of 7 days. To remove the chest tube, the rabbits were lightly anesthetized with ketamine hydrochloride, 17 mg/kg, and xylazine hydrochloride, 2.5 mg/kg.
All rabbits received 150 mL of normal saline solution with 5% glucose subcutaneously immediately after surgery. All rabbits received buprenorphine hydrochloride, 0.05 mg/kg subcutaneously, immediately on awakening and 12 h later. Rabbits who appeared to have any distress over the following 36 h received additional analgesia at the same dose.
The rabbits were killed 28 days after the administration of intrapleural doxycycline by an injection of pentobarbital solution, 40 mg/kg, into the marginal ear vein. The thorax was then removed en bloc from the rabbit. Small incisions were made in the diaphragm to allow better access of the fixative (10% formalin) to the pleural cavities. Attempts were then made to expand the lungs by the injection of 60 mL of 10% formalin into a plastic catheter (6 mm) that had been inserted into the exposed trachea. After the trachea was closed with silk, the entire thorax was submerged in a 10% formalin solution for at least 48 h. (3,5,7-9) Each pleural cavity was exposed using the methodology that we previously described. (5,7-9)
The presence of pleural adhesions, hemothorax, residual effusion, and atelectasis were examined and recorded. The degree of gross adhesions was graded according to the following scheme: 0 = normal pleural space, 1 = one to three small adhesions in the pleural space, 2 = three or more scattered adhesions but lung easily separated from chest wall, 3 = generalized scattered adhesions with areas where the lung could be separated from the chest wall only with difficulty, and 4 = complete obliteration of the pleural space by adhesions. The presence of residual effusion and hemothorax were graded on a scale from 0 to 4 according to the amount of the hemithorax involved: 0 = no effusion or hemothorax, 1 = hemithorax involvement < 15%, 2 = hemithorax involvement from 15 to 33%, 3 = hemithorax involvement from 33 to 75%, and 4 = hemithorax involvement > 75%. The presence of atelectasis was also graded: 0 = no atelectasis, 1 = partial atelectasis, and 9, = complete atelectasis.
The adequacy of the pleurodesis was assessed according to the following criteria: poor, the presence of a score of [less than or equal to] 2 for adhesions, hemothorax or effusion score of 3 or 4, or complete atelectasis (one or more of these); acceptable, the presence of gross adhesion score of 3 or 4, hemothorax or effusion score of [less than or equal to] 2, and no or partial atelectasis; or excellent, the presence of both gross adhesion score of 4, and no hemothorax, pleural effusion, or atelectasis.
Samples of the visceral pleura and lung from each hemithorax were obtained from the anterior lower lobes and placed into 10% neutral buffered formalin. These tissue samples for histologic examination were processed routinely and stained with hematoxylin and eosin. The microscopic slides were evaluated blindly by one investigator (L.R.T.) for the presence of inflammation and fibrosis. The degree of microscopic inflammation and fibrosis was graded as follows: none (0), equivocal (1), mild (9,), moderate (3) or marked (4), as previously described. (5,7-9) The presence of atelectasis was graded similarly from 0 to 4 according to the intensity of the process.
Statistical Analysis
All continuously distributed data were expressed as mean [+ or -] SEM. The ordinal data were reported as the proportions falling within the different study groups. The ordinal data for the control and the steroids groups were compared through [chi square] analysis (SigmaStat; Jandel Scientific; San Rafael, CA). Differences in the treatment results were considered significant when p < 0.05.
RESULTS
All rabbits survived until the designated end point. None of the rabbits required more than one saline solution infusion or more than two doses of buprenorphine hydrochloride. One rabbit in the steroid-weekly group was eliminated from the statistical analysis due to the misplacement of the chest tube in the subcutaneous tissues rather than the pleural space.
The intrapleural injection of doxycycline, 10 mg/ kg, produced a significantly lower adhesion score ([chi square] = 20.5; p < 0.001) when the rabbits were administered triamcinolone (Fig 1). All 10 rabbits in the control group had adhesion scores of 4. In contrast, only four of the rabbits in the steroid-once group and two of the rabbits in the steroid-weekly group had adhesion scores of 4.
[FIGURE 1 OMITTED]
Weekly injection of the steroids appeared to decrease the incidence of atelectasis. Partial atelectasis was observed in three rabbits in the control group, in seven rabbits of the steroid-once group, but in no rabbits in the steroid-weekly group ([chi square] = 10.4; p = 0.005). No hemothoraces were noted in the control group or in the steroid-weekly group. However, small hemothoraces were noted in 4 of the 10 rabbits in the steroid-once group ([chi square] = 8.8; p = 0.06).
The pleurodesis scores were significantly better in the animals not receiving steroids (Fig 2). The pleurodesis score was considered excellent in 7 of the 10 control rabbits, in 2 of 10 rabbits in the steroid-once group, and in 2 of 9 rabbits in the steroid-weekly group ([chi square] = 16.2; p = 0.003). Four of nine rabbits in the steroid-weekly group had a poor pleurodesis, and these were the only rabbits with a poor pleurodesis.
[FIGURE 2 OMITTED]
There was a tendency for the degree of pleural fibrosis to be lower in the groups receiving corticosteroids ([chi square] = 9.2; p = 0.056; Fig 3). The same trend was seen for the degree of microscopic fibrosis as for the macroscopic adhesions; pleural fibrosis scores of 4 were observed in 9 of 10 rabbits in the control group, 5 of 10 rabbits in the steroid-once group, and 2 of 9 rabbits in the steroid-weekly group. There was no significant difference in the degree of pleural inflammation in the three groups.
[FIGURE 3 OMITTED]
When the lungs were examined microscopically, the degree of alveolar fibrosis, alveolar inflammation, and atelectasis were low, in general, and did not differ in the three groups. The alveolar fibrosis score was 0 in all but two rabbits in the steroid-weekly group, both of which had scores of 1. Only one rabbit, in the control group, had more than mild alveolar inflammation. Only one rabbit, in the steroid-once group, had more than mild alveolar atelectasis.
DISCUSSION
This study shows that the administration of triamcinolone, 0.8 mg/kg IM, 24 h before the intrapleural injection of doxycycline reduces the efficacy of the pleurodesis. Moreover, if the steroids are administered before and weekly after the intrapleural injection, the efficacy of the pleurodesis is even less.
The mechanisms responsible for the pleurodesis that follows intrapleural administration of a sclerosing agent are not completely understood. It is thought that the first event occurring after the intrapleural injection of a sclerosing agent is a pleural injury manifested by the denudation of the mesothelial cells (2) and the development of an exudative pleural effusion. (3,5,10) After this initial injury, several factors influence the subsequent process that results in either the development of a pleurodesis or restoration of the pleural space to its normal state. These include the degree of injury, the capacity of the mesothelial cells and fibroblasts to secrete collagen, and the relative balance between metalloproteinases, which degrade collagen, and their inhibitors. (9,11)
It has been suggested that the duration, extension, and intensity of the inflammatory process may influence the final results. This proposition is based on the fact that there is a dose-response effect with most agents; administration of a low dose of a tetracycline derivative, (7) tale slurry, (8) or mitoxantrone (12) does not produce a pleurodesis. This proposition is also supported by two observations in rabbits: (1) tale pleurodesis is inhibited if systemic corticosteroids are administered before and weekly after the intrapleural injection, (3) and (2) tale pleurodesis is inhibited if tumor necrosis factor-[alpha] blocking antibodies are administered concomitantly with tale. (4)
In this present study, the administration of corticosteroids decreased the number of pleural adhesions. Corticosteroids are known to inhibit the early phenomena of the inflammatory process, including the migration of leukocytes into the inflamed area, edema formation, fibrin deposition, capillary dilation, and phagocytic activity. (13) Also, it is known that the corticosteroids have significant effects on the latter manifestations of inflammation, such as proliferation of capillaries and fibroblasts, and deposition of collagen and cicatrization. (13) The present study suggests that the decrease in pleural adhesions and the lower pleurodesis scores in the groups that received steroids were due to both the early and the late effects of triamcinolone, since the rabbits that received the steroids both early and late had a greater reduction in the number of adhesions.
Xie et al (3) showed that steroids markedly decreased the initial inflammatory response after the intrapleural injection of tale slurry. The amount of pleural fluid and the pleural fluid total WBC count 6 h after tale injection were reduced by > 50% in the group receiving corticosteroids. Also, the degree of pleural inflammation was significantly reduced in the steroid group at 6 h after injection. (3) In this present study, we could not evaluate the early inflammatory process because the animals were not killed until 28 days. Unlike the study by Xie et al, (3) our results showed that the degree of pleural inflammation was not significantly decreased in the steroid group at 28 days. The explanation for the differences in the two studies is not known, but may be related to the fact that doxycycline produces injury over a very short time while tale remains in the pleural space and provides a continuous stimulus for inflammation. Indeed, the degree of inflammation (as assessed by the same investigator [L.R.T.]) was less in the doxycycline control group than in the tale control group at 9.8 days. (3)
The present study has important clinical implications. If the results in rabbits can be extrapolated to humans, the efficacy of pleurodesis with doxycycline and probably with other currently used agents will be diminished if the patient is receiving corticosteroids. Many patients undergoing pleurodesis are receiving corticosteroids, eg, those with secondary spontaneous pneumothorax due to COPD or interstitial fibrosis or those with malignant effusions who are receiving corticosteroids as part of their chemotherapeutic regimen. Efforts should be made to minimize the dose of steroids before pleurodesis is attempted. One must also question whether the efficacy of pleurodesis will be reduced if the patient is receiving nonsteroidal anti-inflammatory agents, or chemotherapeutic agents that produce neutropenia.
In conclusion, this study demonstrates that the administration of corticosteroids (triamcinolone, 0.8 mg/ kg) 24 h before the intrapleural injection of doxycycline, 10 mg/kg, reduces the pleural adhesions and the effectiveness of the pleurodesis in rabbits. If the corticosteroids are administered weekly thereafter, the effectiveness of the pleurodesis is reduced even more. If these results can be extrapolated to patients, then One should try to minimize the administration of exogenous corticosteroids before pleurodesis is attempted.
REFERENCES
(1) Light RW. Pleural diseases. 4th ed. Philadelphia, PA: Lippincott, Williams, and Wilkins, 2001
(2) Kennedy L, Harley LA, Sahn SA, et al. Talc slurry pleurodesis: pleural fluid and histologic analysis. Chest 1995; 107: 1707-1712
(3) Xie C, Teixeira LR, McGovern JP, et al. Systemic corticosteroids decrease the effectiveness of talc pleurodesis. Am J Respir Crit Care Med 1998; 157:1441-1444
(4) Cheng DS, Rogers J, Wheeler A, et al. The effects of intrapleural polyclonal anti-tumor necrosis factor alpha (TNF alpha) Fab fragments on pleurodesis in rabbits. Lung 2000; 178:19-30
(5) Wu W, Teixeira LR, Light RW. Doxycycline pleurodesis in rabbits: comparison of results with and without chest tubes. Chest 1998; 114:563-568
(6) Sasse SA, Causing LA, Mulligan ME, et al. Serial pleural fluid analysis using a new experimental model of empyema. Chest 1996; 109:1043-1048
(7) Light RW, Wang NS, Sassoon CHS, et al. Comparison of the effectiveness of tetracycline and minocycline as pleural sclerosing agents in rabbits. Chest 1994; 106:577-582
(8) Light RW, Wang NS, Sassoon CHS, et al. Talc slurry is an effective pleural sclerosant in rabbits. Chest 1995; 107:1702-1706
(9) Vargas FS, Teixeira LR, Silva LM, et al. Comparison of silver nitrate and tetracycline as pleural sclerosing agents in rabbits. Chest 1995; 108:1080-1083
(10) Sahn SA, Good JT. The effect of common sclerosing agents on the rabbit pleura space. Am Rev Respir Dis 1981; 124:65-67
(11) Marshall BC, Santana A, Xu QP, et al. Metalloproteinases and tissue inhibitor of metalloproteinases in mesothelial cells: cellular differentiation influences expression. J Clin Invest 1993:1792-1799
(12) Vargas FS, Teixeira LR, Antonangelo L, et al. Acute and chronic pleural changes after the intrapleural instillation of mitoxantrone in rabbits. Lung 1998; 176:227-236
(13) Goodman LS, Gilman A, Gilman AG. Goodman and Gilman's: the pharmacological basis of therapeutics. 8th ed. New York, NY: Pergamon Press, 1990; 1431-1462
* From the Division of Respiratory Diseases (Dr. Teixeira), Heart Institute (InCor), University of Sao Paulo Medical School, Sao Paulo, Brazil; Pulmonary Disease Division (Dr. Wu), University of California, Irvine, Irvine, CA; and Department of Medicine (Drs. Chang and Light), Saint Thomas Hospital and Vanderbilt University, Nashville, TN.
This work was supported by the Foundation to Support Research from the State of Sao Paulo, and National Board of Scientific and Technologic Development of Brazil.
Manuscript received March 8, 2001; revision accepted May 31, 2001.
Correspondence to: Richard W. Light, MD, FCCP, Director, Pulmonary Disease Program, Saint Thomas Hospital, PO Box 380, 4220 Harding Rd, Nashville, TN 37202; e-mail: flight98@ yahoo.com
COPYRIGHT 2002 American College of Chest Physicians
COPYRIGHT 2002 Gale Group