Rationale: Treatment guidelines for vitamin D monitoring and supplementation in cystic fibrosis (CF) have recently been developed and published by a consensus committee, but have not been prospectively tested. Objectives: To use these guidelines to determine the percentage of adults with CF requiring vitamin D repletion therapy and to evaluate the effectiveness of the currently recommended high-dose oral ergocalciferol repletion protocol. Methods: Prospective study of clinical outcomes after therapy with the recommended vitamin D repletion algorithm. Results: Of 134 adults with CF, 109 (81.3%) were found to have 25-hydroxyvitamin D (25-OHD) levels below the recommended 30 ng/ml. Sixty-six of these adults completed the recommended course of 400,000 IU of oral ergocalciferol over 2 months, and only five (8%) responded with correction of their serum 25-OHD to the goal of 30 ng/ml or greater (mean change, +0.3 ng/ml; from 18.8 to 19.1 ng/ml). In the 33 adults with CF who also completed the recommended second course of 800,000 IU of ergocalciferol over 2 months, none demonstrated correction of their deficiency (mean change, -1.2 ng/ml). Conclusion: The results of this study demonstrate that a majority of adults with CF have serum 25-OHD levels below 30 ng/ml, and the currently recommended ergocalciferol repletion regimen often does not fully correct vitamin D deficiency and may need to be revised to include even higher dosing of ergocalciferol. Further work is needed to establish the ideal 25-OHD level for maximizing calcium absorption and bone health in CF.
Keywords: bone growth; dietary supplements; 25-hydroxyvitamin D; osteoporosis
Survival has steadily improved in cystic fibrosis (CF) over the last few decades, with the median survival age now older than 33 years, and over 40% of all individuals with CF older than 18 years (1). With this increase in survival, there has also been growing recognition of health issues unique to the adult population with CF (2). One of these issues is bone health, because studies using dual-energy x-ray absorptiometry measurements of bone density have determined that, despite their young age, approximately 20 to 25% of adults with CF have osteoporosis and another 40% have osteopenia (3-5). The etiology of this bone disease is multifactorial, with contributors including fat malabsorption (resulting in vitamin D malabsorption and abnormal calcium metabolism) (6-8), glucocorticoid therapy (9, 10), poor nutritional status (11), inadequate gonadal hormones (10, 12), and elevated circulating cytokines (13). Recognition of this increased risk of osteoporosis in CF has led to greater efforts to optimize vitamin D status and calcium absorption (4, 14). The overall prevalence of vitamin D deficiency in adults with CF is strikingly high, with as many as 50 to 60% having 25-hydroxyvitamin D (25-OHD) levels below 20 ng/ml (5, 15). Data demonstrating that serum 25-OHD levels need to exceed 30 ng/ml to prevent a rise in serum parathyroid hormone (16) suggest that the prevalence of vitamin D deficiency in CF may be even higher.
Because of the growing concern about bone disease in CF, the U.S. Cystic Fibrosis Foundation (CFF) convened a panel of experts to develop consensus treatment guidelines to optimize CF bone health, and these recommendations were recently published (17). The guidelines contained several specific recommendations regarding vitamin D. First, greater attention to maintaining adequate serum 25-OHD levels should occur, with levels being checked annually in the late fall with the goal of maintaining serum 25-OHD between 30 and 60 ng/ml (75-150 nmol/L). Second, all individuals with CF who are older than 1 year should receive 800 IU/day of oral ergocalciferol (vitamin D^sub 2^). Failure of this supplementation to maintain serum 25-OHD levels above 30 ng/ml should lead to aggressive repletion with high-dose oral ergocalciferol. The guidelines recommended a stepped approach for repletion, with an initial regimen of 50,000 IU/week of oral ergocalciferol for 8 weeks. Failure of this regimen to raise serum 25-OHD to over 30 ng/ml should lead to a second course of oral ergocalciferol with 50,000 IU/twice weekly for 8 weeks. Persistence of serum 25-OHD levels below 30 ng/ml despite these supplemental regimens should result in consideration of alternative modes of therapy, such as calcitriol or phototherapy. This treatment protocol was developed on the basis of data in individuals without CF, but was recognized as a "first step" in addressing the clear need for more aggressive vitamin D therapy in individuals with CF. Conference leaders stated a need for CF-specific data in the future on which to determine optimal dosing recommendations.
The goals for our study were to determine the percentage of adults with CF who require the recommended vitamin D repletion therapy because of serum 25-OHD levels below 30 ng/ml, to evaluate for the first time the effectiveness of the recommended stepped-approach high-dose ergocalciferol repletion protocol, and to provide CF-specific data to aid in determining optimal dosing recommendations for the future. Some of the results of this study have previously been reported in abstract form (18).
METHODS
Study Population
A total of 134 adults between the ages of 19 and 64 were included in this study, all previously confirmed to have CF by sweat chloride measurements or genotyping. Participants were cared for in the Johns Hopkins Adult CF Program and had been routinely supplemented with 800 IU/day of oral ergocalciferol. Individuals with pancreatic insufficiency had been maintained on brand-name enzymes with doses between 1,000 and 2,500 lipase units/kg/meal. Adults with CF who had previously undergone lung transplantation or who were known to have cirrhotic liver disease were excluded. The 134 participants represented all of the adults with CF regularly seen at the Johns Hopkins Adult CF Program at the time of the study. This study was approved by the Johns Hopkins University School of Medicine Institutional Review Board.
Treatment Protocol
The treatment protocol is outlined in Figure 1. Participants had baseline serum 25-OHD levels determined and those with levels below 30 ng/ml received the recommended 50,000 IU/week of oral ergocalciferol for 8 weeks in addition to their regular multivitamin. At 2 to 4 weeks after completion of therapy, participants had repeat 25-OHD levels to determine therapeutic response. Those with 25-OHD levels still below 30 ng/ml received the recommended second course of oral ergocalciferol of 50,000 IU/twice weekly for 8 weeks. At the completion of the second course of ergocalciferol, subjects again had their serum 25-OHD levels determined.
Behavioral Interventions
To improve patient adherence to the prescribed regimen, a behavioral intervention program, which included initial meetings with a nutritionist and follow-up phone calls, was performed. For each participant, the initial serum 25-OHD result was reviewed, together with the potential risks of low vitamin D levels on bone health. Previous vitamin and enzyme compliance was evaluated and use of brand-name enzymes was verified. Participants were then provided with detailed instruction sheets describing the ergocalciferol supplementation regimen as well as importance of timing for follow-up levels. Participants were called during their 2-month ergocalciferol courses to ensure adherence to the regimen and reinforce need for follow-up levels.
Ergocalciferol Supplements
Ergocalciferol was administered in 50,000-IU gelatin capsules as either generic ergocalciferol (Pliva, Inc., East Hanover, NJ) or Drisdol (SanofiSynthelabo, Inc., New York, NY).
Measurement of Serum Vitamin D
Quantitative determination of serum 25-OHD was performed by a single Quest Diagnostics laboratory (Teterboro, NJ) using the Nichols Advantage 25-OHD Assay (Nichols Institute Diagnostics, San Clemente, CA). Post-treatment values were separately confirmed by Quest using DiaSorin 25-OHD radioimmunoassay kits (DiaSorin, Inc., Stillwater, MN) to ensure vitamin D^sub 2^ levels were not significantly underestimated (19).
Statistical Analysis
Unpaired t tests were used to compare mean values between subjects, and paired t tests were used to compare means within subjects. Proportions were compared using χ^sup 2^ testing. The 25-OHD levels were dichotomized to below 30 ng/ml (low) and 30 ng/ml or greater (normal). Bivariate analyses were performed to determine factors associated with low baseline 25-OHD levels and factors associated with therapeutic response in scrum 25-OHD of at least 4 ng/ml. Independent variables included the following: age, sex, body mass index (BMI), pancreatic insufficiency, FEV^sub 1^, presence of osteopenia/osteoporosis, and season in which levels were drawn. These analyses were performed using both χ^sup 2^ and logistic regression. Where applicable, data are presented as means ± SD. Statistical significance was set at p
RESULTS
Participant Demographics
The characteristics of the 134 participating adults with CF are summarized in Table 1. A full range in severity of lung disease was represented. As expected, approximately 50% of participants were ΔF508 homozygotes and 90% had pancreatic insufficiency. Classification as pancreatic insufficiency was based on the presence of two known pancreatic insufficiency mutations or clinical documentation of fat malabsorption requiring treatment with pancreatic enzyme supplementation. Of the 134 individuals, 112 had previously had their bone density evaluated by dualenergy x-ray absorptiometry scan. Using T-score thresholds of - 1 and -2.5 to define osteopenia and osteoporosis, 40% of individuals had normal bone density, 43.6% demonstrated osteopenia, and 17.4% demonstrated osteoporosis.
Initial 25-OHD Screening
Of the 134 individuals screened, 109 were found to have 25-OHD levels below the recommended 30 ng/ml (81.3 %; Figure 2). The mean 25-OHD level for the entire group was 21.5 ± 10.8 ng/ml, with a median level of 20.3 ng/ml. Table 2 summarizes results from the analysis of factors associated with those having baseline serum 25-OHD levels of 30 ng/ml or greater. In general, there was no clear predictor of those who would have satisfactory levels. Age, sex, BMI, and severity of lung disease were all not predictive of serum 25-OHD levels. Although those individuals with pancreatic sufficiency were approximately three times more likely to have an adequate serum 25-OHD level, vitamin D deficiency was present in 11 of the 17 pancreatic-sufficient patients (64.7%; odds ratio of adequate level, 2.8; p = 0.07). Although self-reported adherence to daily vitamin therapy was not predictive of baseline serum 25-OHD level, individuals who reported rarely taking vitamins tended to have the most severe deficiencies.
First Ergocalciferol Repletion Regimen
Of the 109 individuals with serum 25-OHD levels below 30 ng/ml, 90 were started on the recommended initial ergocalciferol regimen of 50,000 IU/week for 8 weeks. Of the 90, 66 (73%) completed the regimen as instructed and returned for reevaluation of serum 25-OHD. The remainder were unable to confirm adherence to the regimen or did not return for evaluation of 25-OHD levels in the appropriate time interval. Among those completing the initial ergocalciferol regimen, only 5 of 66 (8%) demonstrated correction of their serum 25-OHD to the goal level of 30 ng/ml or greater. The mean overall increase in 25-OHD for the treatment group was only 0.3 ± 8.2 ng/ml (from 18.8 to 19.1, p = 0.8; Figure 3).
Of the 19 patients who were found to be vitamin D deficient but were not treated, seven had moved and transferred care to another caregiver, seven did not make a follow-up visit during the period of the study, two underwent lung transplantation, two were pregnant, and one refused therapy. These individuals were almost identical in characteristics to both the group as a whole and to the 90 individuals with low vitamin D levels started on ergocalciferol (28.7 ± 10.5 years old; 58% female; 89% with pancreatic insufficiency; FEV^sub 1^, 65 ± 29% of predicted; and BMI, 23.4 ± 4.6).
The reasons for drop-out in the 24 individuals who either did not complete the ergocalciferol course or have follow-up serum values evaluated varied: 10 admitted to not taking the ergocalciferol as prescribed, eight did not return to have their serum 25-OHD level evaluated, three moved, and three underwent lung transplantation. These individuals were almost identical in characteristics to both the group as a whole and to the 66 individuals with low vitamin D levels that completed the ergocalciferol course (29.8 ± 8.4 years old; 58% female; 92% with pancreatic insufficiency; FEV^sub 1^, 68 ± 30% of predicted; and BMI, 23.9 ± 6.8).
A bivariate analysis was performed to identify factors associated with response to the ergocalciferol therapy. A response was defined as an increase in serum 25-OHD of 4 ng/ml or greater (half an SD of the group mean). Overall, there were no clear predictors of those who would respond to ergocalciferol replacement, with age, sex, severity of lung disease, and pancreatic sufficiency all failing to be predictive. The most suggestive factor was baseline BMI, with those in lower BMI categories having a tendency to have greater response (p = 0.052).
Second Ergocalciferol Repletion Regimen
Of the 66 individuals treated with the initial course of ergocalciferol, 61 failed to correct their serum 25-OHD to 30 ng/ml or greater and thus were eligible for the recommended higher dose second course of ergocalciferol (50,000 IU/twice weekly for 8 weeks). Of these 61 individuals, 49 were started on the second course, and 33 confirmed completion of the regimen as prescribed and returned for serum 25-OHD levels within 4 weeks. Strikingly, none of the 33 treated with the recommended higher dose second course of ergocalciferol corrected their serum 25-OHD to the goal level of 30 ng/ml or greater. The mean serum 25-OHD level after the second treatment course of ergocalciferol actually decreased slightly from 18.7 to 17.5 ng/ml (Figure 4).
Seasonal Variation
To determine if seasonal variation influenced the apparent lack of response to ergocalciferol supplementation, analysis was performed to determine both the presence of seasonal variation in serum 25-OHD levels and the effect of the season during which ergocalciferol supplementation was taken. As expected, a seasonal variation in serum 25-OHD levels was observed, with highest levels in both the baseline and treatment group occurring during the summer and fall months (Table 3). Analysis also revealed that individuals had a greater increase in their serum 25-OHD when treated during the late summer and early fall months, likely because of the additional contribution of sunlight-induced vitamin D production (Figure 5). The increase in serum 25-OHD after 8 weekly doses of 50,000 IU was 2.9 ± 7.3 ng/ml when completed in late summer or fall versus -0.5 ± 6.2 in the winter and -7.4 ± 8.7 in the spring (p = 0.02 by analysis of variance).
DISCUSSION
The recognition of the high prevalence of vitamin D deficiency in individuals with CF has led to increased efforts to develop strategies to optimize vitamin D and calcium metabolism. These efforts culminated in the 2005 publication of the guidelines from the CFF Consensus Conference on Bone Health in which detailed recommendations for screening and treatment of vitamin D deficiency were outlined (17). Conference leaders based treatment recommendations on experience in individuals without CF and stated that the recommendations may need to be revised as CF-specific data became available. The results of our study confirm the high prevalence of vitamin D deficiency in adults with CF and the need for greater attention to 25-OHD status, but most important, demonstrate that the current guidelines for repletion of vitamin D in CF may need to be modified.
The findings of this study are consistent with the many others, which have shown that the majority of adults with CF are vitamin D deficient. The exact prevalence depends on the threshold used to define "deficient." Studies using a threshold of less than 15 ng/ml estimate the prevalence of deficiency to be 30 to 40% (5,20). Using a threshold of less than 20 ng/ml results in approximately 50 to 60% being deficient (15). However, given that serum parathyroid hormone levels begin to rise with 25-OHD levels below 30 ng/ml, the target 25-OHD level to optimize calcium metabolism is likely more appropriately 30 ng/ml (16,17). Our study suggests that as many as 80% of adults with CF may have serum 25-OHD levels below 30 ng/ml. This estimate is supported by other investigators' results, because reevaluation of previously presented data using a threshold of 30 ng/ml suggests deficiency prevalence in this range (15).
The results from this study also reinforce the need for generalized screening of 25-OHD levels in CF because there were no clinical characteristics clearly predictive of 25-OHD status. Classically, it is believed that individuals with CF with poor nutrition and severe lung disease are most at risk for vitamin D deficiency. However, FEV^sub 1^, BMI, sex, and age all failed to predict vitamin D status. Although individuals with pancreatic-sufficient CF tended to have slightly better serum 25-OHD levels, 65% were still found to have inadequate levels.
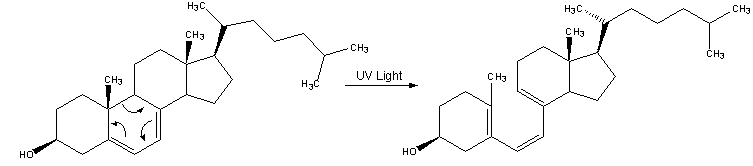
The most important source of vitamin D for all individuals is the sunlight-driven conversion in skin of 7-dehydrocholesterol to cholecalciferol (vitamin D^sub 3^). A minority of vitamin D comes from dietary intake (21). But individuals with pancreatic-insufficient CF have traditionally taken supplemental vitamin D in the form of ergocalciferol (vitamin D^sub 2^) to augment their dietary intake because of their difficulty with absorbing fat-soluble vitamins. It is known, however, that this difficulty with absorption also applies to ergocalciferol. Ergocalciferol malabsorption has been demonstrated in CF both by direct measurements (6, 8) and by the high prevalence of vitamin D deficiency even in those taking regular ergocalciferol supplementation.
At the CFF consensus conference, the results of studies describing efficient correction of vitamin D deficiency with ergocalciferol in individuals without CF were used to develop the recommended repletion guidelines, because no adequate studies in CF existed. These non-CF studies had determined that 50,000 IU of oral ergocalciferol once or twice weekly for several weeks significantly repleted 25-OHD levels in most patients who were deficient (22-24). The results of our study, however, suggest that this repletion regimen is strikingly ineffective in CF. Only 8% (5/66) of those treated with 50,000 IU/week of ergocalciferol for 8 weeks corrected their serum 25-OHD levels to 30 ng/ml or greater. The mean increase in serum 25-OHD level was only +0.3 ng/ml (18.8 to 19.1 ng/ml). No clinical characteristics predictive of response to the ergocalciferol regimen could be identified.
The study results also demonstrate that individuals failing to respond to the initial course of ergocalciferol repletion are unlikely to benefit from the currently recommended second course of ergocalciferol. None of the 33 individuals treated with the second course of ergocalciferol at 50,000 IU/twice weekly for 8 weeks corrected their serum 25-OHD levels to 30 ng/ml or greater. The mean change in serum 25-OHD level for the second treatment group was -1.2 ng/ml.
The reason for the failure of these high-dose oral ergocalciferol regimens to be effective in repleting 25-OHD in CF is likely multifactorial. The one pharmacokinetic study of ergocalciferol absorption in CF found that after a single 100,000-IU oral dose, subjects with CF absorbed only 45% of the vitamin D^sub 2^ that control subjects did (8). This malabsorption occurred even in the setting of taking an appropriate dose of pancreatic enzymes. The amount of malabsorption varied dramatically between participants with CF, with some individuals demonstrating virtually no absorption of vitamin D^sub 2^ despite the large dose. One potential reason for variable absorption of ergocalciferol is variability in the presence of bile and bile salts in individuals with CF (25). Bile is required for the absorption of ergocalciferol and deficiencies of bile and bile salts have been reported in CF (26).
Malabsorption alone may not be the only reason for failure to respond to ergocalciferol, however. The finding in our study that 65% of the adults with pancreatic-sufficient CF were vitamin D deficient suggests that there may be other contributing factors. Previous studies have noted that even after being absorbed in CF, vitamin D^sub 2^ does not efficiently raise serum 25-OHD levels (8). This may be because of a decreased rate of hydroxylation of vitamin D^sub 2^ or more rapid clearance of vitamin D^sub 2^ and 25-OHD (8).
On the basis of the results of this investigation, it is clear that new approaches will need to be identified, which effectively replete vitamin D in CF. One approach might be to try more frequently dosed or longer courses of high-dose ergocalciferol than those currently recommended. Some investigators treating 25-OHD deficiency caused by malabsorption have demonstrated efficacy of doses in the range of 35,000 to 50,000 IU/day of ergocalciferol for several months (27, 28). We have recently treated five adults with CF who had previously failed to respond to the recommended ergocalciferol protocol, with 50,000 IU of oral ergocalciferol daily for 30 days (total dose of 1.5 million IU of ergocalciferol over 30 days rather than the currently recommended 800,000 IU over 60 days). Four of the five increased their serum 25-OHD to over 30 ng/ml, suggesting that oral ergocalciferol might be effective in CF if high enough doses are used. Until fully studied in CF, this approach will require close monitoring to ensure hypervitaminosis D or hypercalcemia does not result. Alternatively, intramuscular ergocalciferol may be considered, although a previous study in CF failed to note a significant rise in serum 25-OHD levels 2 weeks after a single injection of 500,000 IU (29, 30).
Several studies have suggested that the more polar hydroxylated vitamin D preparations (25-OHD and 1,25-OHD) are better absorbed than ergocalciferol and may be a better supplement option (31, 32). Unfortunately, the only single-ingredient product containing 25-OHD was removed from the market by the manufacturer in 2001, leaving none currently available in the United States. Calcitriol (1,25-OHD) is the most readily available hydroxylated vitamin D preparation, and short-term studies in CF have suggested that it is absorbed and improves calcium homeostasis (33). The use of calcitriol would require a change in strategies for monitoring therapeutic response, because 25-OHD levels may not be corrected despite improvements in calcium homeostasis (33).
Last, natural or artificial sunlight exposure is an underused method for increasing vitamin D stores and bypassing absorption issues. Although results have varied between studies, a single exposure of the arms and face to ultraviolet light has been estimated to produce approximately 2,000 IU of vitamin D (28). Individuals with CF are at risk for decreased sunlight exposure because they are often counseled to be cautious while taking antibiotics, which make them sun-sensitive. The CFF Consensus Conference guidelines specifically identified natural or artificial ultraviolet light as an alternate source of vitamin D and encouraged exposure to sunlight for individuals with CF. The goal is two or three exposures/week to a quantity of sunlight that is 25% of the amount it would take to cause a mild pinkness to the skin (17).
In the long run, one key question that still needs to be answered is this: What is the ideal physiologic serum 25-OHD level for maximizing calcium absorption and bone health in individuals with CF? A serum 25-OHD goal of 30 ng/ml is based on data in individuals without CF, suggesting parathyroid hormone rises when 25-OHD falls below 30. However, further work is needed to determine if such a threshold exists in CF and to identify an appropriate goal level for serum 25-OHD.
In summary, the results of this study provide several important messages for caregivers of patients with CF. First, the majority of adults with CF have serum 25-OHD levels below the currently recommended 30 ng/ml, and routine screening is needed because there are no clinical characteristics, including pancreatic function, that are clearly predictive for 25-OHD status. Second, the currently recommended high-dose ergocalciferol repletion regimens for CF may not adequately correct vitamin D deficiency in many patients and may need to be revised to include even higher dosing of ergocalciferol. Third, further work is needed to establish the ideal physiologic serum 25-OHD level for maximizing calcium absorption and bone health in individuals with CF.
Conflict of Interest Statement: None of the authors have a financial relationship with a commercial entity that has an interest in the subject of this manuscript.
Acknowledgment: The authors thank Kathie Bukowski for her assistance in preparing this manuscript.
References
1. Cystic Fibrosis Foundation Patient Registry. 2003 annual data report. Bethesda, MD: Cystic Fibrosis Foundation; 2004.
2. Yankaskas JR, Marshall BC, Sufian B, Simon RH, Rodman D. Cystic fibrosis adult care: consensus conference report. Chest 2004;125:1S-39S.
3. Elkin SL, Fairney A, Burnett S, Kemp M, Kyd P, Burgess J, Compston JE, Hodson ME. Vertebral deformities and low bone mineral density in adults with cystic fibrosis: a cross-sectional study. Osteoporos Int 2001;12:366-372.
4. Donovan DS Jr, Papadopoulos A, Staron RB, Addesso V, Schulman L, McGregor C, Cosman F, Lindsay RL, Shane E. Bone mass and vitamin D deficiency in adults with advanced cystic fibrosis lung disease. Am J Respir Crit Care Med 1998;157:1892-1899.
5. Haworth CS, Selby PL, Webb AK, Dodd ME, Musson H, Niven RM, Economou G, Horrocks AW, Freemonl AJ, Mawer EB, et al. Low bone mineral density in adults with cystic fibrosis. Thorax 1999;54:961967.
6. Lo CW, Paris PW, Clemens TL, Nolan J, Holick MF. Vitamin D absorption in healthy subjects and in patients with intestinal malabsorption syndromes. Am J Clin Nutr 1985;42:644-649.
7. Aris RM, Lester GE, Dingman S, Ontjes DA. Altered calcium homcostasis in adults with cystic fibrosis. Osteoporos lnt 1999; 10:102-108.
8. Lark RK, Lester GE, Ontjes DA, Blackwood AD, Hollis BW, Hensler MM, Aris RM. Diminished and erratic absorption of ergocalciferol in adult cystic fibrosis patients. Am J Clin Nutr 2001;73:602-606.
9. Bhudhikanok GS, Lim J, Marcus R, Harkins A, Moss RB, Bachrach LK. Correlates of osteopenia in patients with cystic fibrosis. Pediatrics 1996; 97:103-111.
10. Conway SP, Morion AM, Oldroyd B, Truscott JG, White H, Smith AH, Haigh I. Osteoporosis and osteopenia in adults and adolescents with cystic fibrosis: prevalence and associated factors. Thorax 2000;55:798804.
11. Grey AB, Ames RW, Matthews RD, Reid IR. Bone mineral density and body composition in adult patients with cystic fibrosis. Thorax 1993;48:589-593.
12. Leifke E, Friemert M, Heilmann M, Puvogcl N, Smaczny C, von Zur MA, Brabant G. Sex steroids and body composition in men with cystic fibrosis. Eur J Endocrinol 2003; 148:551-557.
13. Aris RM, Stephens AR, Ontjes DA, Denenc BA, Lark RK, Hensler MB, Neuringer IP. Lester GE. Adverse alterations in bone metabolism are associated with lung infection in adults with cystic fibrosis. Am J Respir Crit Care Med 2000;162:1674-1678.
14. Hecker TM, Aris RM. Management of osteoporosis in adults with cystic fibrosis. Drugs 2004;64:133-147.
15. Ott SM, Aitken ML. Osteoporosis in patients with cystic fibrosis. Clin Chest Med 1998;19:555-567.
16. Chapuy MC, Preziosi P, Maamer M, Arnaud S, Galan P, Hercbcrg S, Meunier PJ. Prevalence of vitamin D insufficiency in an adult normal population. Osteoporos hit 1997;7:439-443.
17. Aris RM, Merkel PA, Bachrach LK, Borowitz DS, Boyle MP, Elkin SL, Guise TA, Hardin DS, Haworth CS, Holick MF, et al. Guide to bone health and disease in cystic fibrosis. J Clin Endocrinol Metab 2005;90: 1888-1896.
18. Boyle MP, Noschese ML, Watts SL, Davis ME, Lechtzin N. Prevalence of 25-hydroxyvitamin D deficiency in adults with CF and effect of high dose ergocalciferol supplementation [abstract]. Pedlatr Pulmonol 2003;S25;350:A473.
19. Holick MF, Chen TC, Ray R, Jamieson D, Lu Z, Mathieu J. Evaluation of precision and accuracy of Nichols Advantage 25-hydroxyvitamin D assay for 25(OH)D2 and 25(OH)D3: comparison of four methods with LC-mass spectrometry [abstract]. / Bone Miner Res 2004;19(Suppl 1);S343:585.
20. Flohr F, Lutz A, App EM, Matthys H, Reincke M. Bone mineral density and quantitative ultrasound in adults with cystic fibrosis. Eur J Endocrinol 2002;146:531-536.
21. Holick MF. Vitamin D: the underappreciated D-lightful hormone that is important for skeletal and cellular health. Curr Opin Endocrinol Diabetes 2002;8:87-98.
22. Adams JS, Kantorovich V, Wu C, Javanbakht M, Hollis BW. Resolution of vitamin D insufficiency in osteopenic patients results in rapid recovery of bone mineral density. J Clin Endocrinol Metab 1999;84:2729-2730.
23. Kantorovich V, Gacad MA, Seeger LL, Adams JS. Bone mineral density increases with vitamin D repletion in patients with coexistent vitamin D insufficiency and primary hyperparathyroidism. J Clin Endocrinol Metab 2000;85:3541-3543.
24. Malabanan A, Veronikis IE, Holick MF. Redefining vitamin D insufficiency. Lancet 1998;351:805-806.
25. Heubi JE, Hollis BW, Specker B, Tsang RC. Bone disease in chronic childhood cholestasis: vitamin D absorption and metabolism. Hepatology 1989;9:258-264.
26. Colombo C, Roda A, Roda E, Piceni Sereni L, Brega A, Fugazza R, Giunta A. Bile acid malabsorption in cystic fibrosis with and without pancreatic insufficiency. J Pediatr Gastroenterol Nutr 1984;3:556-562.
27. Charles P, Mosekilde L, Sondergard K, Jensen FT. Treatment with high-dose oral vitamin D2 in patients with jejunoileal bypass for morbid obesity: effects on calcium and magnesium metabolism, vitamin D metabolites, and faecal lag time. Scand J Gastroenterol 1984;19:10311038.
28. Vieth R. Vitamin D supplementation, 25-hydroxyvitamin D concentrations, and safety. Am J Clin Nutr 1999;69:842-856.
29. Ontjes DA, Lark RK, Lester GE, Hollis BW, Hensler MM, Aris RM. Vitamin D depletion and replacement in patients with cystic fibrosis. In: Norman AW, Bouillon R, Thomasset M, editors. Vitamin D endocrine system: structural, biological, genetic and clinical aspects. Riverside, CA: University of California, Printing and Reprographics; 2000, pp. 893-896.
30. Compston JE, Horton LW, Thompson RP. Treatment of osteomalacia associated with primary biliary cirrhosis with parenteral vitamin D2 or oral 25-hydroxyvitamin D3. Gut 1979;20:133-136.
31. Compston JE, Merrett AL, Hammett FG, Magill P. Comparison of the appearance of radiolabelled vitamin D3 and 25-hydroxy-vitamin D3 in the chylomicron fraction of plasma after oral administration in man. Clin Set (Lond) 1981;60:241-243.
32. Sitrin MD, Bengoa JM. Intestinal absorption of cholecalciferol and 25-hydroxycholecalciferol in chronic cholestatic liver disease. Am J Clin Nutr 1987;46:1011-1015.
33. Brown SA, Ontjes DA, Lester GE, Lark RK, Hensler MB, Blackwood AD, Caminiti MJ, Backlund DC, Aris RM. Short-term calcitriol administration improves calcium homeostasis in adults with cystic fibrosis. Osteoporos Int 2003;14:442-449.
Michael P. Boyle, Michelle L. Noschese, Sharon L. Watts, Marsha E. Davis, Shane E. Stenner, and Noah Lechtzin
Johns Hopkins Adult Cystic Fibrosis Program, Johns Hopkins Division of Pulmonary and Critical Medicine, Baltimore, Maryland
(Received in original form March 22, 2004; accepted in final form April 22, 2005)
Supported by grant BOYLE02AO from Cystic Fibrosis Foundation Therapeutics and National Institutes of Health grant M01-RR-00052.
Correspondence and requests for reprints should be addressed to Michael P. Boyle, M.D., Johns Hopkins Adult CF Program, 1830 East Monument Street, 5th floor, Baltimore, MD 21205. E-mail: mboyle@jhmi.edu
Am J Respir Crit Care Med Vol 172. pp 212-217, 2005
Originally Published in Press as DOI: 10.1164/rccm.200403-387OC on April 28, 2005
Internet address: www.atsjournals.org
Copyright American Thoracic Society Jul 15, 2005
Provided by ProQuest Information and Learning Company. All rights Reserved