After a 6-month priority review, the Food and Drug Administration last month approved duloxetine for managing pain associated with diabetic peripheral neuropathy, a symptom of nerve damage that affects up to 5 million Americans with diabetes.
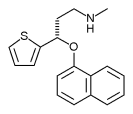
The development marks the first time a drug has been specifically approved for this indication. Duloxetine (Cymbalta) is a balanced potent inhibitor of serotonin and norepinephrine reuptake manufactured by Eli Lilly & Co. The FDA approved duloxetine in August as a treatment for major depression in adults.
In an interview, Dr. Russell K. Portenoy, chairman of the department of pain medicine and palliative care at Beth Israel Medical Center, New York, called duloxetine's approval "significant because diabetic painful polyneuropathy is a very prevalent, distressing, and challenging pain syndrome."
"But it's also significant because drugs that are useful for painful diabetic polyneuropathy will most likely be adopted [in the treatment of] neuropathic pains more generally. As a group, these syndromes are in need of advances in therapy," said Dr. Portenoy, who is not affiliated with Eli Lilly or any clinical trials of the drug.
Duloxetine's approval followed two randomized, 12-week, double-blind, placebo-controlled, fixed-dose studies in more than 1,000 nondepressed adults who had diabetic peripheral neuropathy for at least 6 months. Patients received doses of either 60 mg or 120 mg per day. On average, patients in the studies were aged 60 years, had diabetes for about 11 years, and had diabetic neuropathy for about 4 years.
Of patients treated with duloxetine in the two studies, 58% reported at least a 30% sustained reduction in pain. Only 34% of patients who took the placebo reported this degree of sustained pain reduction.
Dr. Amy S. Chappell, a neurologist at Eli Lilly's headquarters who helped conduct the trials, noted that although both doses were safe and effective in patients who participated in the studies, the 120-mg dose was not as well tolerated as the recommended dose of 60 mg per day.
Adverse effects such as nausea, sleepiness, dizziness, constipation, and dry mouth "are definitely dose related," Dr. Chappell told this newspaper. "That wasn't any surprise. However, the adverse effects are self-limited. They usually go away in 5-7 days after initiation of treatment, and they are mild to moderate. We had very few patients discontinue [the trials] because of nausea, for instance, which was our most common adverse event. So it is manageable."
Other drugs aimed at helping patients manage pain associated with diabetic neuropathy are awaiting FDA approval, including pregabalin (Lyrica), which is manufactured by Pfizer Inc. In the meantime, clinicians have been using a variety of other agents off label--including gabapentin, amitriptyline, and venlafaxine--in an effort to help relieve pain in this patient population. That strategy is likely to continue, Dr. Portenoy said.
"On the other hand, there is a high likelihood that there will be a group of patients that responds specifically to duloxetine, because there's that kind of variability seen in the population," he noted. "Having another drug with this kind of mechanism available to treat neuropathic pain is a bona fide advance."
"My expectation is that physicians will start using this drug to treat diabetic polyneuropathy quickly, that pain specialists will begin to use this drug for other types of neuropathic pain, and that this drug will be used in combination with other drugs by pain specialists for patients with challenging neuropathic pain syndromes," Dr. Portenoy said.
Duloxetine's exact mechanism of action remains unclear, but the drug is known to increase the availability of specific monoamines in the brain. "It is also known that monoaminergic pathways are involved in pain modulation," he explained. "It is speculated that this mechanism of action--which is responsible for the antidepressant effects--is also responsible for the analgesic effects."
Dr. Chappell noted that the highest rates of pain associated with diabetic peripheral neuropathy occur in people who have had diabetes for at least 25 years. Other risk factors include poorly controlled blood sugar levels, high blood pressure, obesity, and being over the age of 40. Symptoms can include sensations of burning, tingling, and numbness in the toes, feet, legs, hands, arms, and fingers.
BY DOUG BRUNK
San Diego Bureau
COPYRIGHT 2004 International Medical News Group
COPYRIGHT 2004 Gale Group