The day after giving birth to her first child in 1999, Chicago native Missy Lavender realized that any physical exertion, including picking up her newborn, made her leak urine. Until her pregnancy, Missy had led an active life, jogging 2 miles a day and watching her diet. After her son's birth, however, Missy found herself struggling to deal with her new condition, known as stress urinary incontinence (SUI).
"At my first postpartum checkup, I was mortified and depressed," she says. "I told my doctor I was leaking. She told me to go home and do Kegels (pelvic exercises) for six months. I couldn't accept living like that." But live like that she did. At least at first. "I remember getting ready to go out with my husband one night. It really hit me when I had to figure out how to wear a huge pad in my little black pants," Missy says.
Women with SUI experience an involuntary loss of urine when increased abdominal pressure pushes on a weakened urethral sphincter, a ring of muscle that acts as a shutoff valve for your bladder. This increased pressure comes from the stuff of everyday life: exercising, coughing, laughing, sneezing, and lifting. The primary cause of SUI is damage done from giving birth vaginally. A recent study in the New England Journal of Medicine involving more than 15,000 women showed 21 percent of women who delivered babies vaginally had some incontinence. For women who had cesarean sections, that number was 16 percent. Sometimes, SUI goes away on its own; mostly it does not.
Unfortunately, only 1 in 12 women seek help for SUI when it first shows up, and only half ever seek treatment. That's because an air of secrecy and shame often surrounds SUI, says Nancy Muller, executive director of the National Association for Continence, an advocacy and education group based in Charleston, South Carolina. "Women with SUI can end up sacrificing their quality of life. They shun sexual intimacy and often lose the ability to explore new places and spaces," she says.
What's most unfortunate about the women who never seek help is that there are effective treatment options, says Diane Newman, co-director of the PENN Center for Continence and Pelvic Health in Philadelphia. Start with your family doctor or gynecologist. "These physicians can address SUI with you and, if necessary, help you find a urogynecologist or urologist," she says. These are specialists in urinary tract and pelvic floor disorders.
NEW TREATMENTS
THE TENSION-FREE VAGINAL TAPE SLING. An increasing number of surgeons are training in a procedure called tension-free vaginal tape sling (TVTS), says Dr. Basil Kocur, associate clinical professor of obstetrics and gynecology and a urogynecologist at St. Vincent's Hospital and Medical Center in New York City. It's the latest of dozens of surgical techniques used to treat SUI. The TVTS procedure has fewer complications and less recovery time than older types of surgery. "TV-P3 has revolutionized surgery for SUI," says Kocur.
The success rate for the procedure averages between 85 and 95 percent. Women shouldn't have the surgery until they're done having kids because pregnancy can undo the results, requiring yet another procedure afterward. KEGELS, WITH A TWIST. The exercises known as Kegels improve symptoms 50-80 percent of the time when performed properly. Therein lies the difficulty:. Research in the American Journal of Obstetrics and Gynecology shows that half of women do not perform Kegels properly.
In response to this, a company called DesChutes Medical Products created a pelvic muscle trainer called Myself. The small computerized trainer guides women through a daffy five-minute series of Kegels. A nonlatex vaginal sensor gives immediate feedback on whether you're performing the exercises properly.
In a small study, 36 percent of women using Myself had significantly fewer and smaller episodes of urine leakage and 44 percent considered themselves cured. For more information, visit www.deschutesmed.com or call 800/323-1363 to find a store that sells the device.
OLDER YET STILL HELPFUL TECHNIQUES
FLUID INTAKE MODIFICATION. For some women, modifying fluid intake can solve much of the problem. It varies from woman to woman--some may need to increase the amount they drink, while others may need to decrease or change the timing of when they drink. A doctor can help you figure out what's best for you.
ELECTRICAL STIMULATION, Doctors have used electricity to rebuild damaged muscles for years. The technique is also used for SUI. Probes deliver small shocks to the pelvic floor to help rebuild its strength. Research has been mixed on electrical stimulation for SUI: Some studies have found it helpful, others not. Still, it may be an option for women who want to avoid surgery.
Whatever treatment you choose, bear in mind that it may work wonderfully, it may work fairly well, or in rare cases, not at all. "I'm not 100 percent and I may never be," says Missy Lavender, who chose surgery after she had her second child. "But I'm better."
And what does better look like? Missy is back to jogging, back to swinging her kids up in the air, and back to enjoying life with her husband. Better is good.
IN THE PIPELINE
There has never been an approved medication for treating stress urinary incontinence (SUI)--those "gotta go" TV ads are for a drug that treats urge incontinence, a different condition. But that may soon change. Duloxetine, a drug in development by Eli Lilly and Company, has shown promise in early trials. In a 12-week study of 1,913 women aged 22 to 83, women who took the drug experienced a 52 percent reduction in SUI episodes. After a year, 80 percent of patients who used duloxetine had improved symptoms.
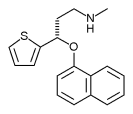
Duloxetine targets the nerves that control the urethral sphincter-the shutoff valve for your bladder. "I view the advent of duloxetine as exciting because it potentially staves off more invasive treatments," says Dr. Roger Dmochowski, professor of urology at Vanderbilt University in Nashville. "Also, using a pharmaceutical option to bolster other treatments and improve pelvic muscle tone makes sense." Eli Lilly and Company is hoping the drug will be available in late 2004 or early 2005 under the brand name Yentreve.
MORE ABOUT INCONTINENCE TREATMENTS, www.bhg.com/incontinence
COPYRIGHT 2004 Meredith Corporation