The number of persons in the United States who were diagnosed with Alzheimer's disease in the year 2000 was 4.5 million. The prevalence of Alzheimer's disease increases with age, affecting 1 percent of patients 60 years of age, but rising to 30 percent of those 85 years of age. Cummings reviewed the management of this commonly encountered cause of dementia.
Alzheimer's disease is marked by a steady decline in cognitive function, accompanied by mood and behavior disturbances, especially as the disease progresses. Motor or sensory abnormalities, gait disturbances, and seizures typically do not occur, although these may appear in the later stages. Increasing evidence indicates that the accumulation of neurotoxic beta-amyloid peptide plays a central role in this debilitating disorder. The neurofibrillary tangles, inflammation, and oxidation effects that received attention early in the investigations of Alzheimer's disease appear to be secondary effects precipitated by deposition of this peptide.
The author notes that the initial work-up of a patient with suspected dementia should include screening measures for causes other than Alzheimer's disease. Thyroid function testing, vitamin 812 level, complete blood count, and a comprehensive metabolic panel (i.e., serum electrolytes, renal function, hepatic function) typically are included in the laboratory screen. The review author recommends a screening brain imaging study (computed tomography or magnetic resonance imaging) during the work-up as well.
Treatment of Alzheimer's disease has proved to be difficult. Options available to date have produced modest benefits in slowing the decline in cognitive function. Results of drug therapy trials typically have shown improvements of 2.5 to 3.5 points on a 70-point scale of cognitive function. This represents about a six-month reversal in the usual 7-point decrease in function that occurs annually in persons with Alzheimer's disease. Therapies specifically targeted to beta-amyloid peptide are under investigation, but none has been produced yet. Antioxidants, principally vitamin E, have not been shown to improve cognitive function in patients with Alzheimer's disease, but can delay progression to some clinical milestones (e.g., placement in a nursing home). Higher dosages of vitamin E supplementation (i.e., 2,000 IU daily) are advocated by some for patients with Alzheimer's disease. Although brain inflammation is evident in Alzheimer's disease, prospective trials of steroidal and nonsteroidal anti-inflammatory drugs have failed to show benefit. Hormone therapy in women with dementia initially was thought to be beneficial, but this was not borne out in prospective trials.
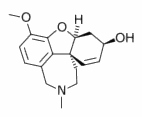
The mainstay of drug therapy for patients with Alzheimer's disease is cholinesterase inhibitors (see accompanying table) for patients with mild to moderate dysfunction. Tacrine is used rarely because of hepatoxicity. The other three agents (i.e., donepezil, galantamine, and rivastigmine) appear to be largely equivalent in efficacy. The nausea, vomiting, diarrhea, and other side effects that accompany these agents may be ameliorated by a slow titration of dosing and giving the medications with meals. The review author suggests waiting up to four weeks between dose escalations to decrease the adverse effects.
Memantine is a newer medication for the treatment of Alzheimer's disease that works by antagonizing the N-methyl-D-aspartate receptor. The U.S. Food and Drug Administration has approved memantine for treatment of moderate to severe Alzheimer's disease, and it may be used in combination with a cholinesterase inhibitor. The cognitive benefits seen with this agent have been modest as well. To date, no serious adverse effects from memantine are apparent.
Management of depression, agitation, and other neuropsychiatric symptoms often becomes necessary as Alzheimer's disease progresses, and the review article covers this area as well. Use of antidepressants and other psychotropic medications tends to follow usual guidelines, with the exception that tricyclic antidepressants usually are avoided, owing to their anticholinergic properties.
The author notes that caregivers of patients with Alzheimer's disease tend to report more physical and mental health problems than their peers. Referral of caregivers to community assistance organizations that deal with Alzheimer's disease may help decrease their burden.
Cummings JL. Alzheimer's disease. N Engl J Med July 1, 2004;351:56-67.
COPYRIGHT 2005 American Academy of Family Physicians
COPYRIGHT 2005 Gale Group