Gamma-hydroxybutyrate (GHB) is an illicitly marketed substance that has recently gained popularity among body builders and party attendees as a drug of abuse. GHB is a depressant that acts on the central nervous system. It is purported as a strength enhancer, euphoriant and aphrodisiac and is one of several agents reported as being used as a "date rape" drug. Because of its central nervous system depressant effects, GHB can be lethal when combined with alcohol or other depressants. Currently, there is no accepted medical use for GHB, and the U.S. Food and Drug Administration has prohibited its manufacture and sale. Clinicians should be familiar with the typical clinical presentation of GHB and its adverse effects. In addition, patients should be warned of its potential toxicity and be cautioned to avoid the use of GHB. (Am Fam Physician 2000;62:2478-82,2483.)
Gamma-hydroxybutyrate (GHB) is a depressant that acts on the central nervous system and has recently become a popular drug of abuse. GHB is distributed illegally as a purported strength enhancer, euphoriant and aphrodisiac.(1) Bodybuilders claim GHB helps metabolize fat and build muscle, and persons who attend nightclubs and parties (such as all-night "raves") use it as a euphoriant. There are new reports of GHB even being used as a "date rape" drug.(2)
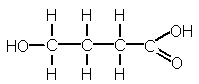
GHB is chemically related to gamma butyrolactone and 1,(4) butanediol. These products are often listed as "party drugs" on Internet Web sites, advertised in muscle-building magazines and sold in health food stores as dietary supplements. The U.S. Food and Drug Administration (FDA) recently issued a warning to the public about these products because they have been linked to at least 122 serious illnesses,(3) and as many as six deaths.(2) Nevertheless, GHB continues to be widely available through illicit sales, home manufacture and recipes that are easily obtainable on Internet Web sites.
Illustrative Case
A 50-year-old man was brought to the emergency department by paramedics after being found lying prone and unresponsive on his patio. The initiating event was not witnessed, but his girlfriend reported that he had recently been using cocaine and other drugs, including GHB. The patient had no response to deep pain and his pupils were 2 mm in diameter, with a sluggish light reflex. The patient's vital signs in the field were: blood pressure, 170/110 mm Hg; pulse, 70; and respirations, 20. He was given intravenous naloxone and dextrose 50 percent solution with no response.
On arrival at the emergency department, the patient remained unresponsive to voice or pain; his Glasgow Coma Scale score was 3. He was hypothermic with a rectal body temperature of 33.8[degrees]C (92.9[degrees]F), his pulse had decreased to 56, and his blood pressure had decreased to 142/96 mm Hg. Pupils, at this time, were 8 mm in diameter, with a sluggish light reflex bilaterally and he had no gag reflex. Bradycardia was noted on cardiac examination and bowel sounds were hypoactive. The remainder of the physical examination was unremarkable.
The patient was administered a repeat dose of naloxone, 2 mg intravenously, with the minimal response of a brief episode of tachypnea. The patient was then given lidocaine, 100 mg intravenously; succinylcholine, 100 mg intravenously; and pancuronium bromide, 15 mg intravenously, followed by endotracheal intubation. A nasogastric tube was placed. Stomach irrigation revealed a few pill fragments, and, subsequently, the patient was administered 100 g of charcoal.
A Foley catheter was placed with return of clear yellow urine, which was sent for a toxicology analysis with a blood sample that had been previously drawn. The patient remained comatose and was transported to the computed tomographic (CT) scanner.
Arterial blood gas measurements after intubation were as follows: pH, 7.41;
partial pressure of carbon dioxide (Pco2), 32 mm Hg; partial pressure of arterial oxygen (Pao2), 415 mm Hg; oxygen saturation, 98 percent on 100 percent oxygen by endotracheal tube. Laboratory results showed the following serum electrolyte levels: sodium, 142 mEq per L; potassium, 4.2 mEq per L; chloride, 104 mEq per L; and carbon dioxide content, 26 mEq per L. Anion gap was 12 mEq per L; blood urea nitrogen, 12 mg per dL (4.3 mmol per L); creatinine, 1.2 mg per dL (110 [micro]mol per L); and glucose, 83 mg per dL (4.6 mmol per L). The white blood cell count was 16,000 per mm3 (16.0 3 109 per L); hemoglobin, 14.5 g per dL (145 g per L); hematocrit, 44 percent (0.44); and a platelet count of 282,000 per mm3 (28.2 3 109 per L). Creatine kinase (CK) was 634 U per L with an isoenzyme MB fraction of 13.3 ng per mL. The CK-MB index was 2.1, a borderline value that is inconclusive for myocardial injury at the admitting hospital.
Comprehensive urine and serum drug screens revealed only the presence of cocaine and opiates. Subsequent urinalysis by gas chromatography revealed the presence of GHB. Serum ethanol level was zero.
The electrocardiogram revealed a normal sinus rhythm with left axis deviation and diffuse ST-segment depression. The CT scan of the head showed no evidence of acute changes, and a chest radiograph was negative.
The patient began to respond to verbal stimuli approximately two hours after arrival at the emergency department. During the next hour, the patient became increasingly alert and returned to his normal mental status.
The patient was admitted to the hospital and extubated on the day of admission. His hospital course, which included a psychiatric consultation, was uneventful, and the patient was discharged to a drug rehabilitation program.
Public Health
GHB is a relatively new drug of abuse, yet it has more than 30 common street names (Table 1). Case reports in the past decade have demonstrated its potential for severe morbidity and death.(1) Poison control centers have reported increasing numbers of GHB cases, most resulting in coma.(4) Between August of 1995 and September of 1996, poison control centers in New York and Texas received reports of 69 acute poisonings from GHB. In the past two years, at least six deaths have been attributed to GHB ingestion.(2)
With a little knowledge of chemistry, GHB can be easily synthesized from readily obtainable materials. The manufacturing of GHB can be a lucrative business, with an initial investment of $800 having a comparative street value of approximately $92,000.(2)
Until recently, possession of GHB was not illegal under federal law. Even though most states had made the possession of GHB a criminal offense, its use prevailed, especially in "rave" clubs and in the athletic underground.(5,6) On February 18, 2000, President Clinton signed the bill H.R. 2130 (the Hillory J. Farias and Samantha Reid Date-Rape Drug Prohibition Act of 2000), which made GHB a schedule-I drug.
History
GHB was first synthesized in 1960 as an alternative anesthetic to aid in surgery because of its ability to induce sleep and reversible coma. However, it had little analgesic effect, and onset of coma was often associated with seizure activity including tonic-clonic jerking movements of the limbs or face.(7,8)
In the late 1980s, GHB was marketed and sold in the health food industry as a "growth hormone stimulator" to help bodybuilders promote muscle mass and maintain weight, and as an over-the-counter sedative agent. In 1991, the drug was banned by the FDA after several reports of adverse reactions in individuals using nutritional and weight loss supplements containing GHB.(9) Despite the FDA ban, GHB continues to be manufactured and sold clandestinely.
Toxicity
GHB's growing reputation as a euphoriant has contributed to its popularity as a recreational drug. When actor River Phoenix collapsed and died outside the Viper Room in Los Angeles in October, 1993, rumor spread that he had died of an overdose of GHB. Although this rumor was never confirmed, it further stimulated street interest in the agent.(10)
Adverse effects related to GHB ingestion are highly variable among individuals (Table 2). Users will typically experiment with GHB dosing to obtain the desired effects. This variability among users combined with the inherent variability in street manufacturing, makes GHB a highly dangerous drug to consume.(2) Furthermore, the dosage-response curve for GHB is steep, and exceeding the intoxicating dose can result in severe adverse effects. Adverse effects typically occur within 15 minutes of ingestion of GHB.(7)
Treatment
The management of GHB ingestion is primarily supportive, particularly if there is no reason to suspect a combination toxic exposure (Table 3). Supportive management includes aspiration precautions and pulse oximetry. If concomitant ingestion is suspected, consideration should be given to gastric lavage and activated charcoal. In the case of isolated GHB ingestion, gastric lavage and activated charcoal are of limited value because the gastrointestinal absorption of GHB is rapid and small amounts of the drug are typically involved (generally 1.25 to 4 tablespoons).(10)
Without confirmatory evidence of GHB ingestion, the clinician must rule out other causes for the patient's altered mental status. Physicians should be aware of the possible co-ingestion of other drugs or alcohol and treat these accordingly.
In the presence of severe respiratory depression, hypoxia, or a combination toxic exposure, rapid sequence intubation is generally indicated for airway protection during lavage and during the treatment of hypoxia. However, a conservative approach to intubation is considered prudent, especially when the history of GHB ingestion is reliable. In one study,(11) only eight out of 25 patients with a Glasgow Coma Scale score of 3 required intubation.
Commonly used agents for reversal of coma have little or no use in the treatment of GHB ingestion. Further research is warranted before the use of these agents is recommended for GHB intoxication.
Despite the severity of altered mental status and the degree of support required to manage these patients, several case series have indicated that patients generally recover consciousness spontaneously.(1,11) Recovery of consciousness usually takes two to six hours and is followed by weaning and extubation in patients who required intubation. Patients who are extubated may be admitted to a regular hospital room and monitored. In selected cases, patients who are in stable condition and whose symptoms resolve may be discharged directly from the emergency department after a period of observation.
Patient Screening and Counseling
Although GHB use is reportedly highest among teenagers and young adults, its use cuts across all boundaries. The authors recommend that GHB use be discussed as part of the HEADSS (home life, education, activities, drugs, suicide, sex) assessment as well as the social history. When drug use is a concern, patients should be asked specifically about GHB use.
When GHB use is suspected or discovered, the patient should be counseled about the dangers of GHB use. As always, appropriate counseling and the consideration of referral to a rehabilitation program should be made. As with any other drug, the physician should inquire about multisubstance abuse.
Final Comment
GHB is a potentially dangerous drug, associated with coma and seizure-like activity. Currently, GHB has no accepted medical use, and the FDA prohibits its manufacture and sale. Physicians should be alerted to the adverse effects of GHB because abuse may become more widespread as reports of its euphoric effects increase experimentation. In addition, health care professionals must be aware that despite FDA intervention, this substance is still available to and used by bodybuilders and party attendees. As with any illicitly manufactured drug of abuse, the likelihood of adverse reactions is increased by the variance in purity and dosages taken. It is the physicians responsibility to educate the public about the dangers of this unusual recreational drug and report cases to poison control centers so that accurate statistical data may be collected regarding the prevalence of GHB use.
REFERENCES
(1.) Li J, Stokes SA, Woeckener A. A tale of novel intoxication: seven cases of gamma-hydroxybutyric acid overdose. Ann Emerg Med 1998;31:723-8.
(2.) Ropero-Miller JD, Goldberger BA. Recreational drugs. Current trends in the 90s. Clin Lab Med 1998;18:727-46.
(3.) U.S. Food and Drug Administration. Report serious adverse events associated with dietary supplements containing GBL, GHB, BD. Retrieved August 2000, from the World Wide Web: http://vm.cfsan. fda.gov/~dms/mwgblghb.html.
(4.) Li J, Stokes SA, Woeckener A. A tale of novel intoxication: a review of the effects of gamma-hydroxybutyric acid with recommendations for management. Ann Emerg Med 1998;31:729-36.
(5.) Viera AJ, Yates SW. Toxic ingestion of gamma-hydroxybutyric acid. South Med J 1999;92:404-5.
(6.) Suner S, Szlatenyi CS, Wang RY. Pediatric gamma hydroxybutyrate intoxication. Acad Emerg Med 1997;4:1041-5.
(7.) Galloway GP, Frederick SL, Staggers FE, Gonzales M, Stalcup SA, Smith DE. Gamma-hydroxybutyrate: an emerging drug of abuse that causes physical dependence. Addiction 1997;92:89-96.
(8.) Vickers M. Gammahydroxybutyric acid. Int Anesthesiol Clin 1969;7:75-89.
(9.) Ross TM. Gamma hydroxybutyrate overdose: two cases illustrate the unique aspects of this dangerous recreational drug. J Emerg Nurs 1995;21:374-6.
(10.) Marwick C. Coma-inducing drug GHB may be reclassified. JAMA 1997;277:1505-6.
(11.) Chin RL, Sporer KA, Cullison B, Dyer JE, Wu TD. Clinical course of gamma-hydroxybutyrate overdose. Ann Emerg Med 1998;31:716-22.
TED O'CONNELL, M.D., is chief resident in the family practice program at Santa Monica-UCLA Medical Center, Santa Monica, Calif. Dr. O'Connell received a medical degree from the University of California, Los Angeles, School of Medicine.
LILY KAYE, PHARM.D., is assistant clinical professor of medicine at the University of California, Los Angeles, School of Medicine, and director of pharmacology education and research at Santa Monica-UCLA Medical Center, Santa Monica, Calif. Dr. Kaye graduated from the University of Southern California School of Pharmacy, Los Angeles, Calif., where she also completed a residency in primary care.
JOHN J. PLOSAY III, M.D., is the associate director of emergency services at Santa Monica-UCLA Medical Center, Santa Monica, Calif. Dr. Plosay graduated from Pennsylvania State University, College of Medicine, Hershey, Pa. He served an internship at Allegheny General Hospital, Pittsburgh, Pa., and completed his residency in emergency medicine at Morristown Memorial Hospital, Morristown, N.J.
Address correspondence to Ted O'Connell M.D., Santa Monica-UCLA Family Practice Residency, 1920 Colorado Ave., Santa Monica, CA 90404 (e-mail: toconnel@mednet.ucla.edu). Reprints are not available from the authors.
COPYRIGHT 2000 American Academy of Family Physicians
COPYRIGHT 2001 Gale Group