We retrospectively reviewed 60 fractures of the tibial plafond treated by either an ankle-sparing diaphyseal-epiphyseal technique using the Ilizarov ring fixator or by an ankle-spanning technique using a monolateral articulated external fixator. The Ilizarov ring fixator was applied in 24 fractures and the monolateral articulated transarticular external fixator in 20. Both techniques were combined with limited open reduction and internal fixation of the articular surface if necessary. Between three and nine years after the injury, all patients returned for clinical and radiological assessment and evaluation of ankle function using the modified Mazur score. There were no significant differences between the two groups in terms of age, gender, mechanism of injury, type of fracture or length of follow-up.
The mean functional ankle score was 86 points for the Ilizarov group and 82 points for the articulated fixator group. The difference was not significant (p = 0.07). There were no significant differences between the groups with regard to the radiographic score and late complications. Patients treated with the Ilizarov ring fixator had significantly better ankle and subtalar movement.
We conclude that both techniques of external fixation are satisfactory methods of treatment for fractures of the tibial plafond, but that the total are of movement of the joint is preserved better without bridging the ankle.
Intra-articular fractures of the tibial plafond are difficult to treat1 and many options have been described for their management. Nonoperative measures such as closed reduction and casting, fixation by pins and plaster cast and calcaneal traction have yielded poor results.2 Open reduction and internal fixation (ORIF) with plates and screws is associated with a high rate of complications including wound breakdown, superficial or deep infection, osteomyelitis and occasionally amputation. External fixation (EF) with or without limited ORIF has therefore gained popularity.8-17 Various types of external fixation have been recommended in order to decrease the rate of complications compared with plating.16,18-20 Three techniques of EF have been described and all may be used in association with limited ORIF. Either a fixator to bridge the ankle and immobilise the joint7,8,12 or an articulated device to allow movement or a ring fixator which obtains purchase in the epiphyseal-metaphyseal junction by means of tensioned wires may be used. Favourable results have been claimed for each method.9-11,13,14,17,21-23
However, these studies have usually involved different types of fracture, treated by various external fixators and have focused on the details of treatment, complications and rates of healing. The effect of using joint-spanning and joint-sparing fixators on the eventual range of movement of the ankle has not been investigated.
We present the results of a non-randomised, retrospective study which attempted to analyse the mid-term functional outcome using two different techniques of EF in the treatment of intra-articular fractures of the tibial plafond. The early complications, revision operations and details of treatment were not addressed in this study.
Patients and Methods
After obtaining the approval of the Human Subjects Review Board of our hospitals, we retrospectively reviewed the radiographs and notes of 60 patients with AO/ASIF type-C1, type-C2 or type-C3 fractures of the tibial plafond24 seen between January 1991 and March 2000 and managed by one of us. One patient had died because of an abdominal injury and 15 could not be traced. These 16 patients were excluded from the study leaving 44 for analysis.
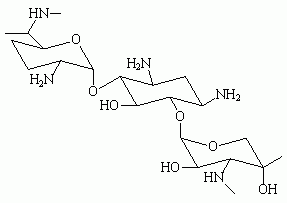
Group 1 consisted of 24 patients who had had fibular fixation and the diaphyseal-epiphyseal Ilizarov technique of EF (Hipokrat, Izmir, Turkey) without spanning the ankle (Fig. 1). Group II consisted of 20 patients, had had fibular fixation followed by placement of a medial spanning articulated external fixator (Orthofix, Verona, Italy) (Fig. 2).
There were no significant differences between the groups in terms of age, the mechanism of injury and the length of follow-up. The ratio of male to female patients was the same in both groups (Table I). In group I there were 18 men and six women with a mean age of 37.8 years (20 to 62) and in group II 15 men and five women, with a mean age of 40 years (22 to 58).
There were six open fractures (three grade I, two grade II and one grade III-A) in group I and six (two grade I, two grade II, two grade 1II-A) in group II, according to the grading system of Gustilo and Anderson.25 All the fractures were classified as AO/ASIF type C.24 There were four 43-C1, 16 43-C2 and four 43-C3 fractures in group I and four 43-C1, 12 43-C2 and four 43-C3 in group II. An associated fracture of the fibula was found in 22 patients in group I and 19 in group II. The mean soft-tissue score was 2.0 for the remaining 18 closed fractures in group I and 1.9 for the 14 closed in group II. Soft-tissue injury in the closed fractures was graded by the system of Tscherne and Rojczyk.26
The mechanism of injury included 26 motor-vehicle accidents and 18 falls from a height (Table I). Thirty patients had an isolated fracture of the tibial pilon. Fourteen had associated injuries including fractures of the shaft of the femur (two), of the tibia (two), of the humerus (three), of the distal radius (four), of the proximal humerus (one) and of the hip (one), two abdominal injuries and one closed-head injury.
The mean duration of follow-up in group I was 64 months (36 to 108) and in group II was 70 months (42 to 112).
All patients who had an open fracture had had debridement and irrigation followed by immediate stabilisation of the fracture on an emergency basis. The limbs with closed fractures were immobilised in either a splint or with calcaneal traction on a Bohler-Braun frame.
The definitive treatment for closed fractures was delayed for a mean of seven days (O to 14) because of other injuries and/or severe soft-tissue swelling. The associated fractures were also managed surgically in all patients.
Operative technique. Plain anteroposterior (AP) and lateral radiographs were taken and CT carried out before operation in all patients. The operations were performed with the patient supine on a radiolucent table, under fluoroscopic control. A pneumatic tourniquet was not used. All the fibular fractures were initially fixed using a one-third tubular plate (Synthes; Mathys Medical Ltd, Bettlach, Switzerland) through a standard incision just posterior to the fibula.
Reduction of the tibial plafond was accomplished by a closed technique if possible, but usually several small incisions were made to facilitate accurate reduction and fixation. The fragments were sometimes reduced by means of the joystick method. Major fragments were reduced and held temporarily by bone reduction forceps applied pereutaneously. The site of a metaphyseal-diaphyseal fracture was never exposed. The reduction of the articular surface was checked fluoroscopically and the joint was reconstructed using 3.5 or 4.0 mm interfragmentary screws and/or transosseous Kirschner or olive wires.
The Ilizarov frame was preconstructed with two rings for diaphyseal fixation and one for the epiphyseal region. The frame was first applied to the mid-diaphysis of the tibia using 1.8 mm. Between two and four wires were placed in the epiphyseal region and anchored to the distal ring. The distal ring was connected to the diaphyseal rings by three or four threaded rods. All simple and olive wires were appropriately tensioned. Reduction of the metaphysis to the diaphysis was obtained by using the frame as an indirect reduction device under fluoroscopic control before the frame was tightened.
The articulated external fixator was applied as has been described previously11 using 5 mm Schanz screws inserted into the neck of the talus and the tuberosity of the calcaneus. The proximal screws were placed free-hand into the medial side of the tibial diaphysis and the articulated ankle clamp anchored. The talus was aligned under the tibia. The ankle was distracted with the compression-distraction unit on the fixator and metaphyseal-diaphyseal reduction was evaluated fluoroscopically. The ball-joint of the fixator was locked. The articulated hinge was also locked with the ankle in the neutral position. Distraction was then decreased until the joint space appeared to be normal or slightly distracted on fluoroscopy.
Bone grafting was not undertaken in any patient. At the end of the procedure, all the pin sites and wires were examined for skin tenting and released if necessary. Patients with closed fractures were given 3 g of cefazolin per day for 48 hours (Cefamezin; Eczacibasi, Istanbul, Turkey). Those with open fractures received 3 g of cefazolin per day and 3 mg/kg per day of gentamicin (Garamycin; Schering-Plough, Istanbul, Turkey) for variable periods.
The limb was elevated after operation. Meticulous pin care with appropriate antiseptic agents was carried out twice per day. After the soft-tissue swelling had decreased, the patients were mobilised non-weight-bearing. Early movement was encouraged. The articulated ankle clamp was released as soon as tolerated by the patient, and active-assisted and passive movements instituted. The patients were not allowed full weight-bearing for at least three months, depending on the progress of healing.
Follow-up and assessment. Patients were seen weekly for the first month, biweekly until the end of the third month and then at intervals of one to three months. Union of the fracture was defined as a bridging callus on two orthogonal radiological views with no pain on standing and no tenderness to palpation. Frames were dynamised for one to two weeks before removal. Patients were then encouraged to be partially weight-bearing and to progress to full weight-bearing as tolerated.
At follow-up, clinical assessment was carried out by one of us (GO). Ankle and subtalar movement was measured. Clawing of the toes and the limb length were evaluated.
Osteomyelitis, nonunion, malunion, limb-length discrepancy, clawing of the toes, osteoarthritis and ankle arthrodesis were all seen as late sequelae. Rotational malunion was measured clinically in a sitting position with the knee and the ankle flexed to 90°. By means of a consistent radiological technique, standing anteroposterior and lateral radiographs of each tibia were made. The angulation of the fracture in the coronal and sagittal planes was measured using a template.27 Malunion was defined as an angular or rotational deformity >5° or a step-off of >2 mm in the articular surface.17,28 Shortening was calculated from the difference between the lengths of the tibiae on the AP radiographs. AP, lateral and mortise radiographs of each ankle were obtained for evaluation of the joint. Osteoarthritis of the ankle was graded on the basis of radiological evidence as grade O (no change), grade 1 (small spurs, cysts or osteophytes without narrowing of the joint space), grade 2 (plus mild narrowing of the joint space and irregularity of the subchondral bone with some sclerosis) or grade 3 (large osteophytes, severe narrowing of the joint space and subchondral collapse). The range of movement was measured by a goniometer with the patient seated and the knee bent for plantar flexion and dorsiflexion. Subtalar movement was recorded as described by McMaster.29 The movement in the contralateral ankle was measured and the difference recorded. Clinical assessment included the ankle score of Mazur, Schwark and Simon30 and modified by Teeny and Wiss.6
Statistical analysis. This was performed using SPSS 10.0 for Windows (SPSS Inc, Chicago, Illinois). Student's t-test was used to compare the mean clinical scores and the mean ankle and subtalar movement, and also to test the differences in age and length of follow-up between the two groups. The Mann-Whitney U test was used to assess osteoarthritis of the ankle. Chi-squared analysis was used to test the differences in gender, the mechanism of injury and the late complications between the two groups. The Spearman correlation coefficient was used to assess the relationship between joint movement and additional injuries. Statistical significance was set at a level of p = 0.05.
Results
Union of the fractures. All the fractures united. The patients in group I wore the fixator for a mean of 16.4 ± 2.4 weeks, and group II wore the articulated frame for 17.2 ± 2.9 weeks. The difference was not significant (p = 0.36).
Functional ankle score. The mean functional ankle scores were 86.8 ± 8 and 82.8 ± 6.5 points in group I and II, respectively.30 The difference was not statistically significant (p = 0.07).
Range of movement. In the modified Mazur system for scoring ankle function the range of movement of the ankle is recorded but not that of the subtalar joint. We therefore calculated the total are of ankle and subtalar movement in both groups in order to compare them separately from the functional ankle score. In group I the mean range of movement was 11.3 ± 7.2° of dorsiflexion (-5 to 25) and 33.5 ± 9.6° of plantar flexion (16 to 50) and in group II, 7.8 ± 5.2° of dorsiflexion (-5 to 15) and 24.8 ± 7.2 of plantar flexion (10 to 35), respectively.
The mean total are of ankle movement in the operated leg was 74.6% of that on the contralateral side in group I and 53.4% in group II. The total are of movement of the ankle had a weak or a negative correlation with additional injuries in both groups (r = -0.24, p = 0.027 for group I; r = -0.33, p = 0.032 for group II).
The mean subtalar movement was 14.8 ± 5.1° of inversion (5 to 25) and 8.2 ± 4.2° (0 to 15) of eversion in group I. The mean total are of movement was 52.2% of that on the normal side (23°/44°). In group II the mean inversion was 9.9 ± 3° (5 to 15) and eversion 6.1 ± 3.3° (O to 11). The mean total are was 34.7% of that on the normal side. The mean total are of subtalar movement was not associated with additional injuries in either group. The patients in group I had a better total are of ankle and subtalar movement than those in group II and the differences were statistically significant for both (P^sub ankle^ = 0.007, P^sub subtalar^ = 0.005).
Radiological score. In group I, six patients had no osteoarthritic changes in the ankle and were rated as grade 0, 13 as grade 1, three as grade 2 and two as grade 3.
In group II, two patients were rated as grade 0, 11 as grade 1, five as grade 2 and two as grade 3. The difference between the two groups was not statistically significant.
Late complications. Osteomyelitis was not seen in any patient in any group. Malunion was noted in five fractures (20%) in group I and in five (25%) in group II. The difference was not significant (p = 0.743). Three patients in each group had claw toes. Shortening of the leg was seen in six patients in group I and four in group II, ranging from 0.5 to 2 cm (p = 0.69). The differences were not significant. No patient had required an ankle arthrodesis.
Discussion
In addition to the soft-tissue injury, these fractures are usually associated with articular comminution, injury to cartilage and general disruption of the joint, all of which can lead to a poor outcome.
Several methods of treatment have been proposed for intra-articular fractures of the tibial plafond, including non-operative treatment, conventional ORIK, EF with limited ORIF and temporary EF with delayed ORIF.1,5,31,32 The non-operative treatment of these fractures yields consistently poor results.2,3,33 Despite early reports of successful treatment, the technique of conventional ORIF with bulky plates is associated with a high incidence of complications and the results have not been reproduced by others.1,3-6 Teeny and Wiss6 reported that 50% of their patients had major complications including wound breakdown, infection, failure of the implant, malunion and non-union. Techniques using EF minimise the risk of severe soft-tissue complications; a significant decrease in the rate of complications has been shown compared with patients treated with plates. 10-17,20,23-28 Surgery can be performed earlier. It avoids extensive soft-tissue dissection, uses limited-access approaches and allows the surgeon to operate early without compromising the soft tissues. However, it does little to reduce the depressed articular fragments. Limited open surgery may not provide adequate visualisation for anatomical reduction of the joint and it may be difficult to obtain adequate stability of small bone fragments.
Intra-articular fractures of the tibial plafond have been treated by EF, with or without limited ORIF since 1965.34 Scheck34 advocated limited open reduction and reconstruction of the surface of the joint and emphasised that minimal stripping of soft tissues should be carried out. Other authors have recorded promising functional results in patients who had been managed by EF combined with limited internal fixation.1,10-14,21-23 However, published studies have usually involved different types of fracture, with relatively limited follow-up and no control group, concentrating on details of treatment, rates of healing and complications.8,10,11,13,21-23,28 There is no evidence in the literature to indicate which type of EF is better for type-C fractures of the tibial plafond and only a few clinical trials have compared EF with ORIF.16,19,20,28,35 Blauth et al19 assessed the long-term results of one of three different methods of management for severe fractures of the tibial plafond. They found that the group which was converted from EF to plating after two weeks had the lowest rate of complications and the best outcome, but they had very limited numbers in their trial.
Wrysch et al,16 in a surgeon-randomised, prospective study, analysed the complications associated with ORIF as opposed to EF and limited internal fixation. At a minimum follow-up of two years, they concluded that EF was a satisfactory method of treatment and was associated with fewer complications. However, most of the patients treated by ORIF had their operations only five days after injury, suggesting that the high rate of complications encountered with this method of management may have been the result of surgical riming rather than technique.16 Watson et al20 analysed the results and complications associated with ORIF with respect to EF and limited internal fixation in type-C fractures. They concluded that both methods were satisfactory in only 60% of patients, but that EF had fewer bony and soft-tissue complications. They were not able to acquire the late radiographs in 60% of their patients and could not comment on the osteoarthritic changes and long-term outcome.
Anglen's study35 had slightly better results with ORIF, but his groups were not comparable since the most severe injuries were treated by EF.
Pugh et al28 studied the outcome using an ankle-spanning unilateral frame, an ankle-sparing ring hybrid fixator and conventional ORIF in fractures of the tibial plafond finding no significant difference in the rates of complications and union in the three groups. They concluded that EF offered advantages in the treatment of soft-tissue problems associated with these fractures, but that malunion was a complication. However, they did not attempt a long-term follow-up and they included type-A and type-B as well as type-C fractures.
The results of the two-staged procedure are promising.18,36,37 Temporary transarticular EF and reconstruction of the length of the fibula by internal fixation allow minimal compromise of the soft tissues. Secondary reconstruction of the articular surface and medial buttressing of the tibia can be performed by minimal invasive osteosynthesis.36,37 There are several disadvantages in the two-staged procedure. Reduction may be difficult two or three weeks after injury, and minimal invasive surgery does not offer adequate visualisation of every fragment with the limited exposure. The preliminary results of the two-staged procedure compare favourably with studies using EF alone. Both reported limited soft-tissue complications and satisfactory outcome.31,32
Cross-ankle fixators which completely immobilise the joint have been used for fractures of the tibial plafond and have not been detrimental to the joint.12 The trials that recommend the two-staged treatment for these injuries often use a cross-ankle fixator to immobilise the ankle for between two and four weeks after injury, forgoing the benefits of early movement.18,32,36,37 EF with limited ORIF has also been shown to result in some decreased ankle movement.3,9-11,13 Bourne et al3 found that 81% of their patients had some loss of movement after ORIF of a type-II or type-III fracture but we are not aware of studies of movement after treatment of type-C fractures of the plafond by either ankle-spanning or ankle-sparing external frames.
The total are of ankle and subtalar movement was decreased in our study as has been seen in other series managed using different protocols.3,6,9-11,13,22,23 Although the functional ankle score and the length of external fixation did not differ significantly, ankle and subtalar movements were better preserved in group I than in group II. This difference between ankle-sparing and ankle-spanning external fixators may be explained by the disturbance of normal ankle kinematics with articulated EF.38-40
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
1. Bone LB. Fractures of the tibial plafond: the pilon fracture. Orthop Clin North Am 1987:18.95-104.
2. Rüedi TP, Allgöwer M. The operative treatment of intra-articular fractures of the lower end of the tibia Clin Ortnop1979:138:105-10.
3. Bourne RB, Rorabeck CH, Macnab J. Intra-articular fractures of the distal tibia: the pilon fracture. J Trauma 1983:23:591-6.
4. Ovadia DN, Beals RK. Fractures of the tibial plafond. J Bone Joint Surg [Am] 1986; 68-A.543-51.
5. Brumback RJ, McGarvey WC. Fractures of the tibial plafond: evolving treatment concepts for the pilon fracture. Orthop Clin North Am 1995:26:273-85.
6. Teeny SM, Wiss DA. Open reduction and internal fixation of tibial plafond fractures: variables contributing to poor results and complications Clin Orthop 1993;292: 108-17.
7. Helfet DL, Koval K, Pappas J, Sanders RW, Dipasquale T. Intrarticular "pilon" fracture of the tibia. Clin Orthop 1994:298:221-8.
8. Murphy CP, D'Ambrosia R, Dabezies EJ. The small pin circular fixator for distal tibial pilon fractures with soft tissue compromise. Orthop 1991;3:283-90.
9. Barbieri R, Schenk R, Koval K, Aurori K, Aurori B. Hybrid external fixation in the treatment of tibial plafond fractures. CUn Orthop 1996;332:16-22.
10. Tornetta P 3rd, Weiner L, Bergman M, et al. Pilon fractures: treatment with combined internal and external fixation. J Orthop Trauma 1993:6:489-96.
11. Bonar SK, Marsh JL. Unilateral external fixation for severe pilon fractures. Foot Ankle 1993,14.57-64.
12. Bone L, Stegmann P, McNamara K, Seibel R. External fixation of severely comminuted and open tibial pilon fractures. CUn Orthop 1993:292:101-7.
13. Marsh JL, Bonar S, Nepola JV, DeCoster TA, Hurtwitz SR. Use of an articulated external fixator for fractures of the tibial plafond. J Bone Joint Surg/Am] 1995;77-A: 1498-509.
14. McDonald MG, Burgess RC, Bolano LE, Nicholls PJ. Ilizarov treatment of pilon fractures. CIm Orthop 1996:325:232-38.
15. Raikin S, Froimson MI. Combined limited internal fixation with circular frame external fixation of mtra-articular tibial fractures. Orthop 1999:22:1019-25.
16. Wyrsch B, McFerran MA, McAndrew M, et al. Operative treatment of fractures of the tibial plafond: a randomized, prospective study. J Bone Joint Surg [Am] 1996; 78-A:1646-57.
17. Marsh JL, Weigel DP, Dirschl DR. Tibial plafond fractures: how do these ankles function over time' J Bone Joint Surg [Am] 2003;85-A:287-95.
18. Haidukewych GJ. Temporary external fixation for the management of complex intra-and penarticular fractures of the lower extremity. J Orthop Trauma 2002;11: 678-85.
19. Blauth M, Bastian L, Kreftek C, Knop C, Evans S. Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma 2001,3:153-60.
20. Watson JT, Moed BR, Karges DE, Cramer KE. Treatment protocol based on severity of soft tissue injury. Clin Orthop 2000:375:78-90.
21. Saleh M, Shanahan MDG, Fern ED. Intra-articular fractures of the distal tibia: surgical management by limited internal fixation and articulated distraction, injury 1993, 24:37-40.
22. Aktuglu K, Ozsoy H, Yensel U. Treatment of displaced pilon fractures with circular external fixatorsof Ilizarov Foot Ankle lnt 1998:4:208-16.
23. Kücükkaya M, Kabukçuoglu Y, Tezer M, Armagan R, Kuzgun U. The treatment of tibial plafond fractures with external fixation: closed or limited open reduction technique. Acta Orthop Trauma Turc2001:35:425-30.
24. Murphy WM, Leu D. Fracture classification: biological significance. In: Rüedi TP, Murphy WM, eds AO principles of fracture management. Fourth ed. Stuttgart: Georg Thieme Verlag 2000:45-58.
25. Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones. J Bone Joint Surg IAm] 1976:58-A: 453-8.
26. Tscherne H, Rojczyk M. The treatment of closed fractures with soft tissue injuries. In Tscherne H, Gotzen L, eds Fractures with soft tissue injuries Berlin etc: Springer-Verlag, 1984:39-45.
27. Milner SA. A more accurate method of measurement of angulation after fractures of the tibia. J Bone Joint Surg [Br] 1997;79-6:972-4.
28. Pugh KJ, Wolinsky PR, McAndrew PM, Johnson KD. Tibial pilon fractures a comparison of treatment methods. J Trauma 1999:47:937-42.
29. McMaster M. Disability of the hindfoot after fracture of the tibial shaft. J Bone Joint Surg [Br] 1976:58-6:90-3.
30. Mazur JM, Schwartz E, Simon SR. Ankle arthrodesis: long-term follow-up with gait analysis. J Bone Joint Surg [Am] 1979;61-A:964-75.
31. Borrelli J Jr, EINs E. Pilon fractures: assessment and treatment Orthop Clin North Am 2002;33:231-45.
32. Sirkin M, Sanders R. The treatment of pilon fractures Orthop Clin North Am 2001:3291-102.
33. Ayeni JP. Pilon fractures of the tibia: a study based on 19 cases. Injury 1988;19: 109-14.
34. Scheck M. Treatment of comminuted distal tibial fractures by combined dual-pin fixation and limited open reduction. J Bone Joint Surg [Am] 1965;47-A:1537-53.
35. Anglen JO. Early outcome of hybrid external fixation for fracture of the distal tibia. J Orthop Trauma 1999:2:92-7.
36. Patterson MJ, Cole DJ. Two-staged delayed open reduction and internal fixation of severe pilon fractures. J Orthop Trauma 1999:2:85-91.
37. Sirkin M, Sanders R, DiPasquale T, Herscovici D Jr. A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma 1999:2:78-84.
38. Fitzpatrick DC, Marsh JL, Brown TD. Articulated external fixation of pilon fractures: the effects on ankle joint kinematics. J Orthop Trauma 1995:1:76-82.
39. Singh AK, Starkweather KD, Hollister AM, Jantana S, Lupichuck AG. Kinematics of the ankle: a hinge axis model Foot Ankle 1992,13:439-46.
40. Lundberg A, Svensson OK, Nemeth G, Selvik G. The axis of rotation of the ankle joint. J Bone Joint Surg [Br] 1989;71-8:94-9.
G. Okcu, K. Aktuglu
From Celai Bayar University, Manisa, Turkey and Ege University, Izmir, Turkey
* G. Okcu, MD, Consultant Orthopaedic Surgeon Department of Orthopaedics and Traumatology, Celai Bayar University, 45040 Manisa, Turkey.
* K. Aktuglu, MD, Consultant Orthopaedic Surgeon Department of Orthopaedics and Traumatology, Ege University, 35040 BornovaIzmir, Turkey.
Correspondence should be sent to Dr G. Okcu at Mithatpasa Cad Camyamac Apt, No 628/3 D3, 35280 Kucukyali, Izmir, Turkey.
©2004 British Editorial Society of Bone and Joint Surgery
doi:10.1302/0301-620X.86B6. 15077 $2.00
J Bone Joint Surg [Br] 2004;86-B:868-75.
Received 28 October 2003; Accepted after review 7 January 2004
Copyright British Editorial Society of Bone & Joint Surgery Aug 2004
Provided by ProQuest Information and Learning Company. All rights Reserved