Editor:
Survival rates for cancer of the head of the pancreas are poor. Unresectable patients live about 6 months. (1) During the past few years I have been involved in the care of a patient with pancreatic cancer. The patient has had unexpectedly positive results. Knowing full well that anecdotes do not replace prospective trials, her treatment history and outcome may still be of interest to health care providers based on the fact that she has responded well in spite of an exceedingly poor prognosis and in light of the natural history of pancreatic cancer. Her case also provides insight into the potential benefits of using multiple modalities in the treatment of advanced cancers.
The Case
The 64 year-old white female presented to her family physician on March 15, 2001 with complaints of dizzy spells, stomach pain and a "swollen stomach." On April 30, 2001, a first CT scan revealed a 5.5 X 5.0 cm mass in the head of the pancreas. Two weeks later, a second CT scan confirmed a 5.6 cm mass on the head of the pancreas, characteristic of pancreatic cancer. Another 2 weeks later pathology of an endoscopic biopsy revealed adenocarcinoma of the head of the pancreas. The patient was told to "get her affairs in order within the next 3-4 weeks." No treatment was offered at that time.
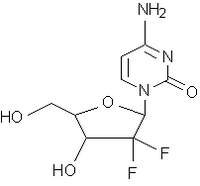
The patient and her husband traveled to another city for second opinion a few weeks later. She was offered 4 treatment options: 1) Gemcitabine; 2) 5FU+Leukovorin; 3) an experimental chemotherapeutic agent and 4) no treatment. By the beginning of July, 2001 another CT scan revealed lung and liver metastases in addition to the pancreatic mass. One day following this scan on July 6, 2001, the patient began a 6-week chemotherapy protocol with Gemzar. The doctor would not allow radiation therapy in addition to the chemotherapy. By August 6, 2001, the 4th chemotherapy treatment was administered. The chemotherapy regimen was ended after 4 weeks due to the intolerable side effects. Some of these side effects causing a poor quality of life included chills every 3-4 hours and body temperatures up to 103 degrees resulting in no quality of life. At this time another CT scan was taken and showed that the lesions were still present at approximately their initial sizes.
Two weeks after stopping the Gemzar, the patient began 5FU+Leukovorin. In addition to this chemotherapeutic regimen, the patient also underwent 27 "funnel" radiation treatments daily to treat the liver and lungs metastases. While receiving the chemotherapy and radiation treatments, the patient learned about the IAT in Freeport, Bahamas. On September 11, 2001, the chemotherapy and radiation was suspended. Four days later the patient began immunoaugmentive therapy at the IAT clinic in Freeport Bahamas. The therapy was comprised of administering sera containing naturally occurring proteins to trigger a reaction to kill tumor cells. The sera are made from human serum protein components (immuno-globulin serum antibodies and alpha 2 macro-globulin deblocking factor) derived from volunteer donors without neoplastic disease, and of tumor complement factor derived from human sera of people with malignancies.
After 1 month of IAT treatment, the patient started on a 12-week treatment comprised of one weekly intradermal injection of heat shock proteins linked to tumor antigen, one weekly intradermal injection of tumor antigen, and twice weekly subcutaneous injections of natural low-dose natural cytokines (collectively referred to as ITL immune therapy). At the same time the patient was started on ImmKine (250 mg capsules, 2 capsules 3X daily) and C-Statin (250 mg capsules, 2 capsules 3X daily). ImmKine is an immune stimulant isolated from bacterial cell walls that induces the production of interleukin 12. Interleukin 12 induces downstream production of anti-angiogenic cytokines. C-Statin is an angiogenesis inhibitor derived from the plant, Convolvulus arvensis, also known as Field bindweed.
On October 29, 2001 a CT scan showed a 2.0 cm mass in the head of the pancreas and resolution of the lung and liver metastases. In mid-January, 2002 the patient returned home from IAT and restarted the 5FU+Leucovorin treatments. Another CT scan performed one week after arriving home showed the pancreatic mass 2.5 cm.
On April 1, 2002 the patient started twice weekly intravenous infusions of 50 grams of vitamin C in 500 cc sterile water. By mid-May, a CT scan showed the pancreatic mass was reduced to less than 2.0 cm. No liver or lung lesions were visible. The vitamin C infusions were discontinued in August, 2002. The patient continued on daily immunoaugmentive therapy and supplements at home.
A CT scan in April, 2003 revealed a 1 cm pancreatic mass with an appearance consistent with a cyst.
Reference
1. Ginsberg GG. New developments in pancreatic cancer. Semin Gastrointest Dis 2000 Jul;11(3):162-7
John Clement, MD
Immunology Research Centre
East Atlantic Drive
Freeport, Grand Bahama
Bahamas
242-352-7455
Fax 242-352-3201
COPYRIGHT 2005 The Townsend Letter Group
COPYRIGHT 2005 Gale Group