Gentamicin-loaded sponges in infected total hip arthroplasty
Acta Orthopaedica February 2005
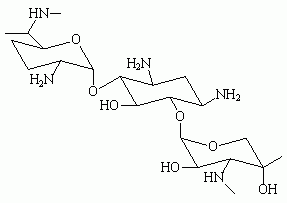
Although prosthesis removal may be recommended for postoperative infection after total hip arthroplasty, several other treatment strategies are available. For early-onset postoperative deep hip prosthesis infection, a combination of debridement, suction-irrigation drainage, and the administration of high-dose antibiotics generally is effective if the treatment is started within 24 to 36 hours of the onset of signs of infection. Treatment involving surgical debridement, irrigation, retention of the prosthesis, and application of several gentamicin-loaded sponges also has been used for acute postoperative total hip arthroplasty infection. Aminoglycosides, including gentamicin, however, have a narrow therapeutic range, and gentamicin is known to produce systemic adverse effects, including ototoxicity, nephrotoxicity, and worsening of neuromuscular disorders. The purpose of this prospective study was to assess whether local application of gentamicin has a significant systemic effect. (1)
Twelve patients aged 54 to 83 years at a hospital in the Netherlands who presented with an acutely infected primary total hip arthroplasty and in whom it was believed that the prosthesis could be retained were evaluated systematically. A surgical debridement was performed, and cultures were collected. Pulse lavage was performed, and several 10-cm by 10-cm by 0.5-cm sponges containing approximately 130 mg gentamicin were introduced into the wound before it was closed. The manufacturer recommends that a maximum of five sponges be used in cases of osseous infections. Serum gentamicin levels were measured on the first postoperative day and on each consecutive day until gentamicin levels no longer were measurable. Additionally, creatinine clearance was calculated. Common statistical procedures were used to analyze the findings.
Findings. Eight women (mean age 72 years) and four men (mean age 68 years) participated in the study. Two-thirds of the patients were classified as American Society of Anesthesiologists physical status category two, and the remaining third was classified as category three. Four or five gentamicin sponges were used in 11 patients (92%), six sponges were used in one patient. Serum levels of gentamicin no longer could be measured after a mean of two days (range 2 to 10 days). Toxic levels of gentamicin (range 2 mg/L to 13 mg/L) were found in seven of the 12 patients (58%) one to 10 days after surgery. Additionally, three patients experienced a significant, persistent drop in renal clearance of more than two standard deviations from the baseline 1 mL per minute preoperative level in each patient.
Clinical implications. The findings of this study revealed that the local use of gentamicin sponges resulted in toxic serum gentamicin levels. Perioperative nurses should understand that gentamicin is excreted via the kidneys; consequently, patients with impaired renal function are at risk for adverse effects. Additionally, nurses should be familiar with the manufacturer's recommendation regarding the number of sponges that can safely be used and ensure that information is readily communicated to the surgeon and other members of the surgical team.
Multimodal rehabititation after colonic resection
Acute Pain May 2005
After abdominal surgical procedures, pain and ileus may contribute to morbidity, prolong hospital stay, and retard convalescence. Indeed, it is assumed that postoperative pain extends the period of ileus, resulting in an increased hospital stay. Epidural analgesia combined with local anesthetics and opioids attenuates ileus and is known to be an effective analgesic method after abdominal surgery. Its effect on postoperative morbidity and hospital length of stay, however, remains controversial.
It has been demonstrated that a multimodal rehabilitation program, including thoracic epidural analgesia, early mobilization and oral nutrition, and a planned 48-hour postoperative stay is feasible during a median hospital stay of two days after elective colonic surgery. The purpose of this prospective study was to evaluate initial postoperative pain intensity and the association with recovery of gastrointestinal function and length of stay in patients undergoing colonic resection and a standardized multimodal rehabilitation program. (2)
Researchers studied patients at a university hospital in Denmark undergoing elective open colonic resection under general anesthesia combined with thoracic epidural analgesia (N = 110). Postoperatively, epidural anesthesia was maintained for 48 hours with bupivacaine 2.5 mg/mL and morphine 50 mcg/mL at 4 mL per hour. Pain was assessed 24 and 48 hours after surgery using a categorical scale (ie, 0 = no pain, 1 = slight pain, 2 = moderate pain, 3 = severe pain). Additionally, time to first postoperative defecation and length of stay were documented. Common statistical techniques Including Chi square, Mann-Whitney U test, and analysis of variance were used to analyze the findings.
Findings. Nineteen patients were excluded from the evaluation because of
* a change in the surgical procedure (n = 2),
* surgical morbidity (n = 6),
* medical factors (n = 4),
* psychosocial or other factors independent of pain (n = 5), or
* incomplete pain data (n = 2).
Of the remaining 91 patients, the median age was 71 years (range 59 to 78 years), and medium duration of surgery was 136 minutes (range 119 to 168 minutes). The median time to defecation was 24 hours, and the median length of stay was 48 hours. Gastrointestinal recovery and length of stay were not significantly different between patients with high pain scores (ie, 3 to 6) versus low pain scores (ie, 0 to 2) (P > .4 and P > .1, respectively).
Clinical implications. The results of this study revealed that effective, dynamic pain relief after colonic surgery generally is obtainable using a continuous thoracic epidural local anesthetic low dose opioid regimen and that the duration of ileus and hospital stay were not related to the intensity of postoperative pain. These results support the hypothesis that postoperative outcome is determined by multiple factors other than pain and pain relief, including preoperative patient information, early oral nutrition and mobilization, and a well-defined and supervised, post-operative, standardized, multimodal rehabilitative care program. Perioperative nurses should understand that this regimen potentially can reduce postoperative length of stay and morbidity after elective colon surgery.
Nocardial endophthalmitis after cataract surgery
American Journal of Ophthalmology May 2005
Postoperative endophthalmitis, especially nocardial endophthalmitis, is one of the most dreaded complications of intraocular surgery. Endophthalmitis refers to intraocular inflammation involving the vitreous and anterior chamber of the eye. Nocardia are aerobic, gram-positive, acid-fast filamentous bacteria; the mode of nocardial infection is normally by implantation or seeding of the organism from soil containing the bacteria. Nocardial endophthalmitis after cataract surgery is associated with a high morbidity and poor visual prognosis because
* it is rare;
* the diagnosis may be delayed due to lack of familiarity, and
* there is a lack of consensus about an appropriate treatment modality.
Consequently, prompt recognition of the clinical features of nocardial endophthalmitis after cataract surgery potentially may improve the prognosis of this disease. The objectives of this retrospective observational study were to analyze the clinical presentation, microbiological profile, and treatment outcomes in cases of nocardial endophthalmitis after cataract surgery. (3)
Researchers retrieved records from a computerized database of cataract procedures at an eye hospital in India between January 2000 and December 2003, and reviewed cases of culture-proven exogenous nocardial endophthalmitis after cataract surgery. The researchers assessed the
* demographic data,
* type of cataract surgery,
* interval from surgery to symptoms,
* comorbid systemic illness,
* visual acuity,
* detailed biomicroscopic examination,
* microbiological survey,
* details of treatment, and
* final visual and anatomic outcomes.
Infection was labeled "early" if symptoms of pain and decreased visual acuity occurred within six weeks of surgery and "late" if symptoms occurred more than six weeks after surgery. The outcome was evaluated in terms of anatomic and functional success. Anatomic success was defined as preservation of the globe, attached retina, best-corrected visual acuity of light perception or better, and no signs of active inflammation after three months. Functional success was defined as attached retina, with best-corrected visual acuity of 20/140 or better. Common statistical techniques, including the Wilcoxon two-sample rank sum test and the Fisher exact test, were used to analyze the data.
Findings. From records of 304,944 cataract surgeries performed during the study period, the researchers identified 196 cases of postoperative endophthalmitis, including 24 cases of nocardial endophthalmitis. Visual outcome was poor in the majority of patients. Final visual acuity of being able to detect only hand motions or worse was found in 19 out of 24 patients (79%), and 11 of 24 patients (46%) had no light perception. Initial visual acuity was significantly associated with the final visual outcome (P = .0026). The majority of patients (ie, 23 of 24) had early onset, and wound infection was noted in 11 of 24 patients (46%). Clinical features included scleral abscess, cotton ball exudates on the iris, and hypopyon.
Clinical implications. The results of this study suggest that nocardial endophthalmitis after cataract surgery is an aggressive disease with poor visual prognosis and that early diagnosis and treatment with good visual acuity at presentation may be associated with better visual outcomes. Given the devastating consequences of endophthalmitis, especially nocardial endophthalmitis, after cataract surgery, perioperative nurses must make every effort to maintain asepsis during these procedures.
Acute-onset endophthalmitis after cataract surgery
American Journal of Ophthalmology June 2005
Endophthalmitis, intraocular inflammation of the vitreous and anterior chamber of the eye, is a rare but serious complication of intraocular surgery that may result in severe vision loss. The increasing use of temporal clear corneal incisions and suture-less surgery raises controversy regarding the possible increased risk of postoperative endophthalmitis after cataract surgery. The objectives of this retrospective, observational study were to report the incidence, clinical settings, and visual acuity outcomes of acute-onset endophthalmitis after cataract surgery. (4)
Acute-onset endophthalmitis was defined as clinically diagnosed endophthalmitis occurring within six weeks after cataract surgery. Researchers reviewed the clinical records of all patients who were clinically diagnosed with endophthalmitis within six weeks after undergoing cataract surgery at a university-affiliated hospital in Miami between January 2000 and November 2004. The same OR protocol was used before all cataract procedures. The protocol included a preoperative prep using povidone-iodine solution to prepare the lids, lashes, and conjunctiva. Cataract surgeries that were combined with other procedures, including pars plana vitrectomy, trabeculectomy, or penetrating keratoplasty, were excluded from the study. Patients with delayed-onset endophthalmitis (ie, infection diagnosed more than six weeks after surgery) also were excluded. Common statistical methods were used to analyze the data.
Findings. The incidence of acute-onset endophthalmitis after cataract surgery was 0.04% (7 of 15,920) for cataract surgeries of all methods compared to 0.05% (6 of 11,462) for cataract surgeries using a temporal clear corneal approach to phacoemulsification, and 0.02% (1 of 1,458) for cataract surgery using other methods (no significant difference, P = .681). The mean duration from the day of cataract surgery to the day of diagnosis with endophthalmitis was 10 days (range one to 21 days). Five of the seven patients (71%) had relative immune compromise, including a patient with polymyalgia rheumatica who was taking immunosuppressive agents and four patients with diabetes mellitus. Additionally, four of the seven patients (57%) with acute-onset endophthalmitis experienced an intraoperative complication (ie, vitreous loss in three patients, iris prolapse in one patient); two of these patients had received topical placement of lidocaine 2% gel before povidone-iodine preparation. Of the six patients who had endophthalmitis after undergoing a temporal clear corneal approach to phacoemulsification, four achieved a final visual acuity of 20/25 or better, and two had a final visual acuity of being able to detect only hand motions or worse.
Clinical implications. The results of this study revealed that the incidence of acute-onset endophthalmitis after temporal clear corneal incision phacoemulsification is 0.05%. Potential risk factors for endophthalmitis may include intraoperative complications, relative immune compromise, application of 2% lidocaine gel before povidone-iodine preparation, and inferior incision location. Although the incidence of acute-onset endophthalmitis is low, perioperative nurses should familiarize themselves with the risks identified in this study and implement procedures to reduce them.
This information is intended for general use only. The clinical implications are specific to the abstracted article only. Individuals intending to put these findings into practice are strongly encouraged to review the original article to determine its applicability to their setting.
NOTES
(1.) A J Swieringa, N J A Tulp, "Toxic serum gentamicin levels after the use of gentamicin-loaded sponges in infected total hip arthroplasty," Acta Orthopaedica 76 (February 2005) 75-77.
(2.) M U Werner et al, "Postoperative pain and gastro-intestinal recovery after colonic resection with epidural analgesia and multimodal rehabilitation," Acute Pain 7 (May 2005) 5-11.
(3.) A Haripriya et al, "Nocardia endophthalmitis after cataract surgery: Clinicomicrobiological study, American Journal of Ophthalmology 139 (May 2005) 837-846.
(4.) J J Miller et al, "Acute-onset endophthalmitis after cataract surgery (2000-2004): Incidence, clinical settings, and visual outcomes after treatment," American Journal of Ophthalmology 139 (June 2005) 983-987.
GEORGE ALLEN
RN, PHD, CNOR, CIC
DIRECTOR OF INFECTION CONTROL
DOWNSTATE MEDICAL CENTER
BROOKLYN, NY
COPYRIGHT 2005 Association of Operating Room Nurses, Inc.
COPYRIGHT 2005 Gale Group