* EVIDENCE-BASED ANSWER
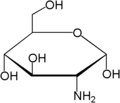
Glucosamine may provide some pain relief. Studies have shown varied results, ranging from glucosamine being superior or equivalent to other agents, to no difference between glucosamine and placebo. However, most of these studies have small sample sizes, short duration, and often other significant flaws. Meta-analyses of available studies suggest a trend toward benefit from glucosamine (strength of recommendation: B).
Glucosamine may help osteoarthritis pain, but it is premature to recommend it universally until better studies are done. Even if glucosamine is effective, this sector of the market is currently unregulated, and products may not contain the amount or kind of glucosamine material advertised on their labels.
* EVIDENCE SUMMARY
Multiple methodological flaws have characterized studies trying to answer this question over the past 30 to 35 years. The companies manufacturing glucosamine have funded most studies. The overwhelming proportion of positive but marginal results raises the possibility of a publication bias (the tendency to publish only positive or supportive results), and the funding sources for the positive studies make that bias plausible.
Identified flaws in the studies include small sample size, inconsistent diagnostic criteria, variable disease sites, differing routes of administration, inconsistent doses, compositions and forms of glucosamine, the brief durations of studies, and poorly defined endpoints. (1) Those problems account for the relatively low quality scores of the studies used in meta-analyses, particularly in earlier ones. Quality scores range from 12% to 52% of optimal and make any definitive conclusions suspect. (2)
The magnitude of the treatment effect is variable. Meta-analyses demonstrate aggregate treatment effects ranging from 0.36 to 1.02--where a small effect is 0.2, a moderate effect is 0.5, and a large effect is 0.8. (2)
When more recent, higher-quality studies are analyzed, trends toward benefit and the effect sizes for glucosamine diminish but remain at aggregate values ranging from 0.26 to 0.44. (2-4) Statistically significant differences exist in some subgroup analyses and secondary endpoints. (5) Typical trends suggest that glucosamine is superior to placebo for pain relief, and less effective but safer than nonsteroidal anti-inflammatory agents. (5)
Statements about safety are speculative given the brief duration of available trials, most of which lasted <10 weeks. (6) Reported adverse effects are few. Mild gastrointestinal, skin, and constitutional symptoms predominate, but seldom at rates much higher than placebo. (3-4) Pain relief may require as much as 4 to 6 weeks of therapy, and short studies may not demonstrate these benefits. The possibility of site-specific benefits or a difference in effect from a different dose or form is impossible to determine based on the current literature.
* RECOMMENDATIONS FROM OTHERS
The American College of Rheumatology Subcommittee on Osteoarthritis believes that it is too early to issue recommendations for use of glucosamine sulfate or chondroitin sulfate for treatment of osteoarthritis. (7)
The National Institutes of Health Glucosamine/Chondroitin Arthritis Intervention Trial (GAIT) began recruiting in May 2002. The design of this study is specifically directed at addressing the flaws of previous studies. This study will enroll 1588 patients at 13 study sites, and will use standardized products and doses with a single route of administration in a double-blinded, placebo-controlled fashion.
The GAIT study will measure change in joint space width (baseline to 2 years) and consists of 4 arms: glucosamine vs placebo, chondroitin vs placebo, glucosamine and chondroitin vs placebo, and celecoxib vs placebo. It is likely that the National Institute of Arthritis, Musculoskeletal and Skin Diseases, in collaboration with the National Center for Complementary and Alternative Medicine, will issue recommendations regarding the efficacy of glucosamine when the study is complete in 2005 or 2006. Updates are available at http://nccam.nih.gov/clinicaltrials/ glucosamine.htm.
David C. Miller, MD, MBA, FAAFP, Cabarrus
Family Medicine Residency, Concord, NC;
Julie Richardson, MLS, Wake Forest University School
of Medicine, Northwest Area Health Education Center,
Winston-Salem, NC
* CLINICAL COMMENTARY
Patients frequently ask me if glucosamine, in combination with chondroitin or methylsulfonylmethane (MSM), reduces or prevents arthritis pain. It appears that glucosamine is safe and offers some promise.
I think a 6-week trial in patients with osteoarthritis is reasonable, preferably using glucosamine--a type that complies with the United States Pharmacopia/National Formulary standards--500 mg orally 3 times daily, once it becomes widely available. In my experience, very few patients who give glucosamine an enthusiastic and adequate trial of therapy continue the course for more than a few months. Those who use it longer often acknowledge only modest relief but continue with the hope of preventing further joint degeneration and increased pain, another currently unsubstantiated expectation.
Russell W. Roberts, MD, Louisiana State University Health Sciences Center, Shreveport, La
REFERENCES
(1.) Deal CL, Moskowitz RW. Nutraceuticals as therapeutic agents in osteoarthritis. The role of glucosamine, chondroitin sulfate and collagen hydrolysate. Rheum Dis Clin North Am 1999; 25:379-395.
(2.) McAlindon TE, LaValley MP, Gulin JP, Felson DT. Glucosamine and chondroitin for treatment of osteoarthritis: a systematic quality assessment and meta-analysis. JAMA 2000; 283:1469-1475.
(3.) Barclay TS, Tsourounis C, McCart GM. Glucosamine. Ann Pharmacother 1998; 32:57-579.
(4.) Heyneman CA, Rhodes RS. Glucosamine for osteoarthritis: cure or conundrum? Ann Pharmacother 1998; 32:602-603.
(5.) Houpt JB, McMillan R, Wein C, Paget-Dellio SD. Effect of glucosamine hydrochloride in the treatment of pain of osteoarthritis of the knee. J Rheumatol 1999; 26:2423-2430.
(6.) Towheed TE, Anastassiades TP, Shea B, Houpt J, Welch V, Hochberg MC. Glucosamine therapy for treating osteoarthritis. Cochrane Database Syst Rev 2001; (1):CD002946.
(7.) Recommendations for the medical management of osteoarthritis of the hip and knee: 2000 update. American College of Rheumatology Subcommittee on 0steoarthritis Guidelines. Arthritis Rheum 2000; 43:1905-1915.
COPYRIGHT 2003 Dowden Health Media, Inc.
COPYRIGHT 2003 Gale Group