The members of the class of sedative-hypnotic drugs are remarkably similar in their pharmacological properties but vary considerably in their chemical structure. The method of classification arose primarily as an attempt to categorize the drugs according to the subjective and behavioral effects produced by them, that is, sedation and hypnosis.[1,2] The barbiturates are the prototype drug and constitute the principal member of the sedative-hypnotic class if the benzodiazepines are not included. The benzodiazepines are actually sedative-hypnotic drugs if actual pharmacological properties are used for classification, but the benzodiazepines are classified as tranquilizers.
The use of barbiturates and other sedative-hypnotic drugs declined (with a few exceptions) with the advent of the benzodiazepines in 1960. Benzodiazepines are similar to barbiturates in their sedative-hypnotic effects but have less lethal acute toxicity than barbiturates. The propensity to develop addiction, tolerance, and dependence with sedative-hypnotics is great, and although the benzodiazepines were initially considered to have less potential for abuse, they may be equal to the sedative-hypnotic drugs in these respects. [3,4]
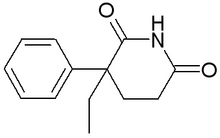
Other members of the sedative-hypnotic class are chloral hydrate, ethchlorvynol, glutethimide, meprobamate, methyprylon, paraldehyde, and triclofos. The pharmacological properties are more alike than distinct, and abuse of, addiction to, tolerance to, and dependence on all members of the class of sedative-hypnotic drugs develop readily and significantly.
PREVALENCE
The historical development of sedative-hypnotic drugs is repetitive. The introduction of one sedative-hypnotic drug for another has been heralded with optimism and claims for improved efficacy and low abuse potential. Unfortunately, the toxicities and potential for abuse, addiction, and development of tolerance and dependence has remained for each subsequent drug that became available for use. Only slight variations in efficacy and untoward effects have distinguished one drug from the other. In their essential features, the sedative-hypnotic drugs have remained the same.
In 1826 the bromides became the first sedatives after alcohol to be prescribed specifically for their sedative-hypnotic effects. Barbituric acid was next introduced in 1903, followed by chloral hydrate ("Mickey Finn") in 1932, meprobamate in 1955, and the benzodiazepines in 1961. The reasons for the failure of each class of drugs to treat only the target symptoms without the development of the adverse effects are inherent not only in the drugs themselves but in the target symptoms as well. The target symptoms, that is, anxiety, depression, and insomnia, are such that their nature lends to the development of abuse and addiction. To suppose that a drug will sedate and induce sleep without producing sedation and hypnosis as side effects is illogical. Furthermore, tolerance and dependence are regular accompaniments to frequent drug use and are natural adaptations of the nervous system to the presence of a foreign chemical,[4,5]
Only estimates through surveys are available for the approximate prevalence rates of use of the sedative-hypnotics. One survey conducted annually since 1975 has described nonmedical use of the sedative-hypnotic drugs among high school seniors.[3] The National Household Survey, performed nationally in the United States six times within a 13-year period (1972 to 1984), has provided additional information about the nonmedical use of drugs among persons living in households.[4] In 1984, the two surveys showed that 14% to 19% of high school seniors and young adults (18 to 25 years old) reported past nonmedical use of sedative-hypnotics. In both surveys these lifetime prevalence rates were generally below those for other major drug classes except heroin and opioid analgesics: alcohol (93% to 95%), tobacco cigarettes (70% to 77%), marijuana (59% to 64%), stimulants (18% to 28%)i cocaine (16% to 28%), and hallucinogens (15% to 21%). The high school survey showed decreases from 1981 to 1985 in nonmedical use, but the National Household Survey did not show this decrease.
A major shortcoming with these surveys is that they do not assess the medical use of the sedative-hypnotics. Because abuse and addiction can occur readily in the medical populations of sedative-hypnotic users, the distinction between medical and nonmedical use is not always sharp, and frequently the two overlap considerably. Any survey or assessment would need clear definitions for medical and nonmedical use, abuse, addiction, tolerance, and dependence. Unfortunately, those definitions are rarely applied in studies of prevalence rates.
Furthermore, certain populations are at higher risk than others for sedative-hypnotic use. The vulnerable populations include those suffering from anxiety, depression, and pain from chronic illness; the elderly; those already using or addicted to other such drugs as alcohol, stimulants cocaine), and, in fact, to any drug of abuse and addiction; and those who suffer from the target symptoms for which the sedative-hypnotic drugs are intended, such as insomnia, anxiety, and depression.[6-9]
PATTERNS OF USE
The barbiturates have been replaced largely by the benzodiazepines in the treatment of seizures and as preanesthetic agents. The more specific action with less lethal and less troublesome side effects when compared with barbiturates has increased the popularity of the benzodiazepines.
Phenobarbital is still used as an anticonvulsant for a variety of seizures. Proven efficacy, long duration of action, and low toxicity after acute and chronic administration have kept phenobarbital popular for many years in spite of other agents that have been developed. The short-acting and intermediate-acting barbiturates, such as secobarbital and pentobarbital, are used for induction of general anesthesia. Their relatively swift onset and short duration of action allow for general anesthesia that is rapid and easily reversible. Ease of titration and low acute toxicity in usual doses make them still useful.[10]
The best-validated human experimental approach for providing information about the abuse and addictive liability of drugs is to utilize placebo-controlled, double-blind methods to characterize subjective effects and behavioral reinforcing properties in human subjects. The abuse and addiction potential of a drug may be inferred from the ability of the drug to serve as a reinforcer, that is, to increase the probability of behavior that results in its administration, and to be able to produce pleasant subjective effects. The results of these studies are similar to those from the animal data for self-administration. The sedative-hypnotics, particularly the barbiturates and methaqualone, are frequently and distinctly self-administered in a pattern of use consistent with abuse, addiction tolerance, and dependence.[9,11]
Alcoholics often take sedative-hypnotics, as do opiate and cocaine addicts. Short-acting barbiturates such as pentobarbital ("yellow jackets") or secobarbital ("red devils") are preferred to long-acting agents such as phenobarbital. Other sedative-hypnotics commonly used by alcoholics are meprobamate, glutethimide, methyprylon, methaqualone, and the benzodiazepines. Paraldehyde and chloral hydrate are still around but have been replaced by the other drugs that do not have such noxious side effects. [12,13]
The patterns of use are many and varied but adhere to the general principles of use, abuse, and addiction of sedative-hypnotics overall. These patterns range from regular use for anxiety and insomnia to episodes of gross intoxication, to prolonged compulsive daily use of large quantities of the drug. For treatment of anxiety, insomnia, and seizures, the most common route of administration is oral. The sedative-hypnotics are also administered intravenously for anesthesia and for acute treatment of seizures.
For those who have developed dependence on the drugs, a preoccupation with acquisition and maintaining adequate supplies of the drug, compulsive use in spite of adverse consequences, and a recurrent pattern of relapse develop. A few inject the drug intravenously ("mainlining") and others inject the drug subcutaneously ("skin-popping"). Some users who develop tolerance may not show obvious intoxication in spite of frequent and heavy doses. The original contact with the drug is through a physician or "street" vendor.
In the patient with medical problems, the abuse may develop gradually over time, whereas use of the drug may accelerate rapidly when prescribing to the addict. Typically, a patient begins using the drug for insomnia or anxiety and progresses through increasing doses, whereas the addict requires high doses initially. Eventually, the drug becomes a major priority of the user's life. Frequently neither the patient nor the physician may recognize the existence of abuse and addiction. Both may interpret the anxiety, tremulousness, and insomnia that emerge when the drug is discontinued as a return of the symptoms for which the drug was initially prescribed, whereas these symptoms more likely represent dependence and withdrawal from the drug and may be protracted over weeks and months.[14-17]
A systematic and thorough evaluation of the causes of insomnia and anxiety are indicated when patients present with these complaints, keeping in mind that individuals who seek these drugs often want to use the drugs for their own sake, not to treat a specific problem. Furthermore, after administration over a period of only 2 to 3 weeks, the sedative-hypnotics begin to produce insomnia and anxiety by virtue of the development of tolerance and dependence. Because the withdrawal effects include frequent anxiety and insomnia as early manifestations of regular use of the sedative-hypnotics, increasing doses are required to offset the appearance of the signs and symptoms of withdrawal. For these reasons, and because of the risk of masking a serious underlying medical, surgical, or psychiatric condition by treating only the symptoms, only short courses of therapy with sedative-hypnotic drugs are recommended. [18-20]
PHARMACOLOGICAL EFFECTS
The members of the sedative-hypnotic class depress the activity of all excitable tissue, particularly nerve cells. This depressant effect is reversible and its action is transient on acute administration. The central nervous system is exquisitely sensitive to sedative-hypnotics in doses that produce little effect on skeletal, cardiac, or smooth muscle. In larger doses, as in acute intoxication, the drugs can suppress function in cardiovascular activity and in other peripheral organs.
The subjective effects are predictable and stereotypic in the nontolerant individual for a given member of the sedative-hypnotic class. Early drug effects are diminished attention and concentration, impaired recent or short-term memory, euphoria, decreased abstraction, reduced cognitive abilities, and a sensation of intoxication. As the blood level increases, the alertness is significantly compromised, mood is depressed, and intellectual function is severely limited. Loss of consciousness occurs in nontolerant individuals at blood levels considerably lower than those observed in tolerant individuals.
The objective effects are visible and measurable. Incoordination of motor movements occurs in gait, hand-eye tasks, saccadic eye pursuit, and truncal equilibrium with relatively low doses of drug, so that such skilled maneuvers as driving an automobile or motor performance under dangerous circumstances is risky. On examination, the physician may observe nystagmus, finger-to-nose and heel-to-shin ataxia, and incoordinated rapid alternating movements of the hands and tandem walking. Respirations are decreased in number and in depth, and blood pressure and pulse may be lowered, especially in higher doses. The tonus of the gastrointestinal musculature and the amplitude of rhythmic contractions are decreased.[21]
The effects from even a single dose, such as 200 mg of secobarbital, have been shown to interfere with performance of driving or flying for as long as 10 to 22 hours. These aftereffects may be prolonged considerably (ie, for days) following several successive doses. Many of the drugs will accumulate after repeated administrations, with increasing effects even after the development of tolerance in chronic use.[22,23] In some individuals, particularly those who are very young or who are elderly, a paradoxical excitement occurs in response to single low doses, especially in pain states.[24,25]
The effects from chronic use of the sedative-hypnotics are similar for all members of the class, and numerous studies have documented persistent symptoms and syndromes that accompany and follow chronic sedative-hypnotic use. The primary organ affected by the drugs is the central nervous system. The major brain functions altered by the drugs are mood, cognition, attention and concentration, insight and judgment, memory, and affect and emotional rapport in interpersonal relationships. Changes in personality that resemble significant personality disorders may develop in regular users of sedative-hypnotics. Characteristics of antisocial, histrionic, paranoid, and other personality traits can occur in chronic use of these drugs. [26]
Not all of the members of the sedative-hypnotics class have been so well studied as the barbiturates and benzodiazepines. The barbiturates act throughout the central nervous system by directly inhibiting neuronal function at polysynaptic and GABA-ergic sites. GABA (gamma-aminobutyric acid), an inhibitory neurotransmitter in the central nervous system, is ubiquitous and is found at both presynaptic and postsynaptic inhibitory neurons.[27]
TOLERANCE AND DEPENDENCE
Two major forms of tolerance, pharmacokinetic and pharmacodynamic, develop in response to the acute and chronic administration of barbiturates. Pharmacokinetic tolerance refers to the absorption, metabolism, and elimination for disposition of the drug. The sedative-hypnotic drugs are highly lipid-soluble, having a high lipid to water ratio. The nonionized form favors lipid solubility. In usual doses, the sedative-hypnotics are readily absorbed through the gastrointestinal tract into the systemic circulation. A redistribution stage occurs, particularly with the more lipid-soluble, short-acting sedative-hypnotics, which favors the rapid uptake by fat and muscle. In this redistribution the drug disappears from the bloodstream but is not transformed or eliminated from the body. When the equilibrium is in the direction of the blood compartment, the drug is slowly released back to the blood from tissue storage. This phenomenon of redistribution accounts in part for both the short duration of action and the persistence of the drug in the body, which can cause the long-lasting (weeks, months) subjective and behavioral effect.[28,29]
The barbiturates compete with other substrates that are metabolized by the cytochrome P-450. The barbiturates and other sedative-hypnotics combine with the cytochrome P-450 system to inhibit the biotransformation of those drugs that also combine with that system. More often, however, the barbiturates cause a marked increase in the microsomal enzyme system to accelerate the metabolism of other drugs including the sedative-hypnotics themselves. This drug-induced biotransformation of itself and other drugs is another source of tolerance and cross-tolerance. Various anesthetics, ethanol, and the sedative-hypnotic drugs are metabolized by and induce the microsomal enzymes to produce multidirectional cross-tolerance. Of concern is that excessive activation of these enzymes can cause dangerous exacerbations of porphyria in persons with intermittent porphyria. [30]
Pharmacodynamic tolerance is an adaptation that occurs at the receptor level. Usually for barbituates this is a cellular change that occurs at the membrane level. The cellular membrane becomes more ordered as tolerance develops. Pharmacodynamic tolerance develops both acutely and chronically in response to the single or repetitive administration of the sedative-hypnotic drugs. Acute tolerance appears to occur significantly earlier than does the induction of microsomal enzymes in response to a single dose of barbiturate. The acute tolerance develops without a change in blood level of drug. Continual administration of the drug over long periods will result in a gradual increase in pharmacodynamic tolerance only if the dose is increased. Otherwise, the degree of pharmacodynamic tolerance remains unchanged after reaching a peak in only a few days of drug administration. Tolerance to the effects on mood, sedation, and hypnosis occurs more readily and is greater than that to the anticonvulsant and lethal effects, so that the therapeutic index decreases with an increase in tolerance. The dose of barbiturate or other sedative-hypnotic may be increased sixfold as tolerance develops. Pharmacokinetic tolerance through stimulation of microsomal enzymes accounts for only twofold to threefold increase in the dose, whereas pharmacodynamic tolerance accounts for the remainder. [31]
Dependence on a drug is marked by the onset of predictable signs and symptoms of withdrawal brought about by cessation of its use. Administration of the drug during withdrawal will abort signs and symptoms of withdrawal. Drug use may be continued to offset the discomfort of withdrawal, particularly if the withdrawal is severe. Withdrawal from sedative-hypnotics is marked by anxiety and depression that can be especially severe. The cycle of increasing tolerance followed by a more severe dependence that allows further increases in drug use is often ended, however, by the escalation of the anxiety and depression.
The withdrawal syndrome contains a wide array of signs and symptoms. Anxiety and depression are rather constant. Others that occur less frequently can be clinically significant, and some are potentially dangerous. Tremors, partial and generalized seizures, delirium, often with visual hallucinations, and delusions, often paranoid, appear less commonly in the spectrum. The withdrawal syndrome from the sedative hypnotics is similar for all members of the class and differs only in severity and temporal onset in the signs and symptoms. The shorter acting drugs typically have a more severe, earlier, and abrupt onset of withdrawal. Conversely, the longer acting drugs have a milder, later, and more gradual onset of withdrawal. As a useful rule of thumb, the withdrawal syndrome for sedative-hypnotics is similar to that of alcohol, which can be used as the prototype for the sedative-hypnotic class of drugs. [29,32,33]
The presence of tolerance and dependence does not necessarily mean that addiction has occurred. Addiction can occur without visible tolerance and dependence. Drug-seeking behavior is the hallmark of addiction. Addiction is marked by preoccupation with acquisition, compulsive use, and relapse to use after efforts to abstain or cut down. Tolerance and dependence frequently develop in addiction because use is often regular and in increasing doses. Tolerance and dependence are expected adaptations of the body to the persistent presence of the drug but do not signal addictive use, as tolerance and dependence follow regular use of many drugs that are not used addictively. Tolerance and dependence are guides to the frequent use of a drug, but addiction may or may not be present. [31,34]
TREATMENT OF WITHDRAWAL
The treatment of withdrawal is necessary to avoid morbidity and even mortality from the adverse consequences. The sedative-hypnotic drugs, including alcohol and benzodiazepines, have cross-tolerance and dependence to one another so that any may be substituted for the other. A common approach is to calculate the dose equivalency for a drug with one frequently prescribed sedative-hypnotic, such as chlordiazepoxide, diazepam, or phenobarbital (Table 1). Long-acting sedative-hypnotics are often selected because patients do not build up tolerance quickly, thus avoiding secondary withdrawal. The time course for administration is determined by the drug for which the withdrawal is being treated. For short-acting drugs, 1 week to 10 days is usually sufficient, whereas for intermediate or long-acting drugs, 2 weeks may be necessary. [35-37]
It is important for the clinician and patient to agree upon a set schedule at the outset so that the physician will avoid attributing drug-seeking behavior for true withdrawal signs and symptoms. Precise calculation of dose equivalency may be a futile exercise because of the difficulty and unreliability of the drug-taking histories in many users. An adequate approach is to categorize the drug use into mild, moderate, and heavy, from which the substitute drug can be approximated. Caution is always urged in interpreting the difference between the signs and symptoms of withdrawal and drug-seeking behavior.
MULTIPLE DRUG USE AND ADDICTION
Next to advancing age, the largest risk factor for suicide is alcohol and drug use. The sedative-hypnotic drugs have pharmacological effects on mood and cognition that render the user vulnerable and liable to suicidal thinking and action. [38-41] The combinations of alcohol with drugs and drugs with drugs are becoming increasingly common and lethal. Fifty percent to 75% of alcoholics use sedative-hypnotics, as do a large number of cocaine addicts. Many of those addicted to sedative-hypnotics are also alcoholics. The need to identify, diagnose, and treat the addiction behind the multiple drug use is essential if lives are to be saved.[42-45]
Most physicians who prescribe drugs need to develop expertise in diagnosing and treating alcohol and drug addiction and dependence. The denial, minimization, and rationalization surrounding drug and alcohol use are shared by the addict and those who care for and treat the addict, that is, family, friends, and physicians. Until all of these participants honestly address the critical elements of drug-seeking behavior, little progress can be made. Effective treatment for sedative-hypnotic addiction exists, and referrals to those skilled in these areas should be made.
References
1 Gary NE, Tresnewsky O: Clinical aspects of drug intoxication: Barbiturates and a potpourri of other sedatives, hypnotics and tranquilizers. Heart Lung 1983; 12:122-127
2. Mendelson WB: The Use and Misuse of Sleeping Pills: A Clinical Guide. New York, Plenum Press, 1977
3. Johnston LD, O'Malley PM, Bachman JG: Drugs and American High School Students 1975-1983. DHHS publication No. (ADM) 85-1374. Government Printing Office, 1984
4. Miller JD, Cisin IH, Gardner-Keaton H, et al: National Survey on Drug Abuse: Main Findings 1982. DHHS publication No. (ADM) 83-1263. Government Printing Office, 1983
5. Fejer D, Smart R: The use of psychoactive drugs by adults. Can Psychiatr Assoc J 1973; 18:313-320
6. Allgulander C: Dependence on sedative and hypnotic drugs: A comparative clinical and social study. Acta Psychiatr Scand Suppl 1978; 270:1:102
7. Borkovec TD: Insomnia. J Consult Clin Psychol 1982; 50:880-895
8. Lader M: The use of hypnotics and anxiolytics in the elderly. Int Clin Psychopharmacol 1986; 1(4):273-283
9. Ator NA, Griffiths RR: Self-administration of barbiturates and benzodiazepines: A review. Pharmacol Biochem Behav 1987; 27(2):391-398
10. Roth T, Roehrs, Zovick R, Conway W: Pharmacological effects of sedatives, hypnotics, narcotic analgesics and alcohol during sleep. Med Clin North Am 1985; 69(6):1281-1282
11. Allgulander C: History and current states of sedation-hypnotic drug use and abuse. Acta Psychiatr Scand 1986; 73:465-478
12. Richter JA, Holman JR: Barbiturates: Their in-vivo effects and potential biochemical mechanisms. Prog Neurobiol 1982; 18:273-319
13. Sampson I: Barbiturates. Mt Sinai J Med 1983; 50:283-288
14. Diagnostic and Statistical Manual of Mental Disorders, ed 3. Washington, DC, American Psychiatric Association, 1987
15. Sellers EM: Addictive drugs: Disposition, tolerance and dependence interrelationships. Drug Metab Rev 1978; 8:5-11
16. Hawthorne JW, Zabora JR, D'Lugolf BC: Outpatient detoxification of patients addicted to sedative-hypnotics and anxiolytics. Drug Alcohol Depend 1982; 9:143-151
17. Wikler A: Review of research on sedative drug dependence at the addiction research center and University of Kentucky. In Thompson T, Unna KR (eds): Predicting Dependence Liability of Stimulant and Depressant Drugs. Baltimore, University Park Press, 1976, pp 147-163
18. Hartmann E: Long-term administration of psychotropic drugs: Effects on human sleep. In Williams RL, Karacan I (eds): Pharmacology of Sleep. New York, John Wiley & Sons, 1976, pp. 211-223
19. Linnoila M, Ervin CW. Brendle A: Efficacy and side effects of flunirazepam and pentobarbital in severely insomniac patients. J Clin Pharmacol 1982; 22:14-19
20. Mellenger GD, Balter MB, Uhlenhuth EH: Insomnia and its treatment: Prevalence and correlates. Arch Gen Psychiatry 1985; 42:225-232
21. Idestrom CM: Flicker fusion in chronic barbiturate usage: A quantitative study in the pathophysiology of drug addiction. Acta Psychiatrica et Neurologicia Scand 1954; (suppl 91):5-92
22. Fishman RH, Yanai J: Long lasting effects of early barbiturates on central nervous system and behavior. Neurosci Biobehav Rev 1983; 17(l):19-28
23. Okamoto M, Rao S, Walewski JL: Effect of dosing frequency on the development of physical dependence and tolerance to pentobarbital. J Pharmacol Exp Ther 1986; 238:1004-1008
24. Svensmark O, Buchthal F: Accumulation of phenobarbital in man. Epilepsia 1963; 4:199-206
25. Hay D, Milne RM, Gilleard CT: Hypnotic drugs, old people and their habits: A general practice study. Health Bull (Edinb) 1986; 44(4):218-222
26. Griffiths RR, Bigelow GE, Liehson I: Differential effects of diazepam and pentobarbital on mood and behavior. Arch Gen Psychiatry 1983; 40:865-873
27. Ho IK, Harris RA: Mechanism of action of barbiturates. Ann Rev Pharmacol Toxicol 1981; 21:83-1 11
28, Richter SA, Harris P, Hanford P: Similar development of tolerance to barbital-induced inhibition of avoidance behavior and loss of righting reflex in rats. Pharmacol Biochem Behav 1982; 16:467-471
29. Fraser HF, Wilker A, Essia CF, Isbell H: Degree of physical dependence induced by secobarbital or pentobarbital. JAMA 1958; 166:126-129
30. Breimer DD: Clinical pharmacokinetics of hypnotics. Clin Pharmacokinet 1977; 2:93-109
31. Miller NS, Dackis CA, Gold MS: The relationship of tolerance, dependence and addiction: A neurochemical approach. J Subst Abuse Treat 1987; 4:197-207
32. Wikler A: Diagnosis and treatment of drug dependence of the barbiturate type. Am J Psychiatry 1968; 125:758-765
33. Okamoto M: Barbiturate tolerance and physical dependence: Contribution of pharmacological factors. Natl Inst Drug Abuse Res Monogr Ser 1984; 54:333-347
34. Khanna JM, Mayer JM: An analysis of cross tolerance among ethanol, other general depressants and opioids. Subst Alcohol Actions Misuse 1982; 3(5):243-257
35. Perry DJ, Alexander B: Sedative/hypnotic dependence: Patient stabilization, tolerance testing, and withdrawal. Drug Intell Clin Pharm 1986; 20:532-537
36. Benzer D, Cushman P: Alcohol and benzodiazepines withdrawal syndromes. Alcohol Clin Exp Res 1980; 4:243-247
37. Reinberg A; Circadian rhythms in effects of hypnotics and sleep inducers. Int J Clin Pharmacol Res 1986; 6(l):33-44
38. Martin RL, Cloninger CR, Guze SB, Clayton PJ: Mortality in a follow-up of 500 psychiatric outpatients. II Cause-specific mortality. Arch Gen Psychiatry 1985; 42:58-66
39. Craig TJ, Lin SP: Medication use and mortality. Compr Psychiatry 1983; 24:183-192
40. Skegg K, Skegg DCG, Richards SM: Incidence of self-poisoning in patients prescribed psychotropic drugs. Br Med J 1983; 286:841 -845
41. Berger FM: Drugs and suicide in the United States. Clin Pharmacol Ther 1967; 8:219-223
42. Miller NS: A primer for the diagnosis and treatment of alcohol and drug addiction. Psychiatry Lett 1987; 5(7):30-37
43. Miller NS, Gold MS: The medical diagnosis of alcohol dependence. N J Med 1988; 84:873-879
44. Cooperstock R: Social Aspects of the Medical Use of Psychotropic Drugs. Toronto, Ont, Addiction Research Foundation of Ontario, 1974
45. Clare AW: Diazepam, alcohol and barbiturate abuse. Br Med J 1971; 4:340
(Tabular Data Omitted)
COPYRIGHT 1989 Dowden Health Media, Inc.
COPYRIGHT 2004 Gale Group