Abstract
A case of lupus erythematosus (LE) and lichen planus (LP) overlap syndrome in a 71-year-old woman is presented. This disease displays characteristics of both LE and LP. The clinical, histologic, and immunopathologic features of this disorder are reviewed.
**********
Case Report
A 71-year-old woman presented to the Bellevue Hospital Medical Center Dermatology Clinic in May, 1999 with a 1-year history of an erythematous eruption on the face, scalp (Figure 1), trunk (Figure 2), and upper extremities. An initial biopsy specimen from the right shoulder was interpreted as a lichenoid dermatitis, and she was treated with multiple topical corticosteroids with moderate improvement. A repeat biopsy specimen from the scalp was obtained in December, 2000. Past medical history included a history of deep venous thrombosis, hypercholesterolemia, and hypertension. Medications included warfarin, simvastatin, and atenolol.
[FIGURE 1 OMITTED]
[FIGURE 2 OMITTED]
Physical examination revealed scattered erythematous scaly papules, and plaques were present on the lower lip, upper back, chest, and forearms. On the vertex of the scalp was an erythematous, atrophic plaque with follicular plugging. No oral lesions were noted.
Evaluation of laboratory data including antinuclear antibody, anti-histone antibody, anti-SS-A antibody, anti-SS-B antibody, lupus anticoagulant, and anti-DNA antibody were negative. C3 and C4 levels were normal. A comprehensive metabolic panel including liver function tests was normal.
Histopathologic examination revealed a superficial and deep perivascular and perifollicular infiltrate of lymphocytes with vacuolar alteration at the dermoepidermal junction (Figure 3). There was also epidermal atrophy, follicular plugging, and dermal mucin. A PAS stain revealed a thickened basement membrane.
Direct immunofluorescence revealed no abnormal deposits of IgG, C3, IgM, IgA, or fibrin in the epidermis; granular, intermittent deposits of C3(+2), broad to granular deposits of IgM(+/-), and broad deposits of fibrin (+3) in the basement membrane zone; and no abnormal deposits of IgG, C3, IgM, IgA, or fibrin in the vascular space.
Discussion
Lupus erythematosus (LE) and lichen planus (LP) may occur as an overlap syndrome which displays clinical, histologic, and/or immunopathologic characteristics of both disorders. Although LE and LP are not uncommon dermatoses, their coexistence or overlap is rare. Approximately 50 cases of LE/LP overlap syndrome have been reported(1). Previous case reports have described two heterogeneous groups of lesions. One type occurs primarily on the extremities as bluish red, atrophic plaques while another type occurs as verrucous papules and nodules on the upper extremities(2,3). Cutaneous lesions have also been described in other sites, including the face, trunk, mucosa, and nails. The diagnosis, however, is based primarily on the combined presence of clinical, histologic, and/or immunologic features of both diseases occurring at the same time. Of note, different lesions occurring in the same patient may be consistent with either LP or LE.
It is important to differentiate between LE and LP in order to make an accurate diagnosis of this overlap syndrome. Both diseases may display similar histologic and immunologic findings of colloid bodies and basement membrane changes. Colloid bodies are generally more numerous and are situated deeper in LP. Basement membrane cleft formation (Max-Joseph spaces) is seen in LP, while areas of basement membrane thickening are more commonly seen in LE. On direct immunofluorescence microscopy, both LE and LP may reveal deposits of immunoglobulins or linear fibrinogen at the basement membrane zone. Immunoglobulin and complement deposition forms a granular pattern along the basement membrane zone in LE (lupus band), while a linear fibrinogen band is often seen at the basement membrane zone in LP(1).
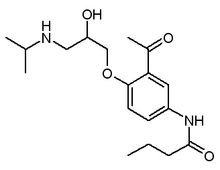
Possible etiologies of LE/LP overlap syndrome include autoimmune, viral, and genetic predisposition. Isoniazid, procainamide, and acebutolol have also been reported as inducing drugs(1). Conversion of cutaneous LE into systemic LE has been shown to occur more frequently in LE-overlap syndromes and has been reported to have an estimated frequency of at least 5-10%(4). Like LE, LE/LP overlap syndrome is associated with a chronic course. Treatment options include systemic retinoids as well as cyclosporin, which has been reported to be effective(5).
[FIGURE 3 OMITTED]
References
1. Inaloz HS, et al. Lupus erythematosus/lichen planus overlap syndrome with scarring alopecia. J Eur Acad Dermatol Venereol 2000; 15(2):171-4.
2. Ahmed AR, et al. Coexistence of lichen planus and systemic lupus erythematosus. J Am Acad Dermatol 1982; 7(4):478-83.
3. Nieboer C. Lupus erythematosus/lichen planus (LE/LP) overlap syndrome. J Am Acad Dermatol 1985; 13(2):297.
4. Jablonska S, Blaszczyk M. Lupus erythematosus. What's new? J Eur Acad Dermatol Venereol 2000; 15(2):103-5.
5. Grabbe S, Kolde G. Coexisting lichen planus and subacute cutaneous lupus erythematosus. Clin Exp Dermatol 1995; 20(3):249-54.
HANNA KIM MD (1), MIRIAM K POMERANZ MD (2)
1 BOSTON UNIVERSITY DEPARTMENT OF DERMATOLOGY, BOSTON, MASSACHUSETTS
2 NYU MEDICAL CENTER, NEW YORK, NEW YORK
ADDRESS FOR CORRESPONDENCE:
Hanna Kim MD
Boston University Department of Dermatology
609 Albany Street, Boston MA 02118
Phone: 617-638-5500
Fax: 617-638-5515
E-mail: hannakim7@hotmail.com
COPYRIGHT 2004 Journal of Drugs in Dermatology
COPYRIGHT 2004 Gale Group