Abelcet
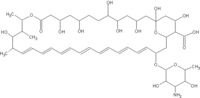
Amphotericin B (Fungilin®, Fungizone®, Abelcet®, AmBisome®, Fungisome®, Amphocil®, Amphotec®) is a polyene antimycotic drug, used intravenously in systemic fungal infections. It was originally extracted from Streptomyces nodosus fungi. Currently the drug is available as plain Amphotericin B, as cholesteryl sulfate complex, as lipid complex, and as liposomal formulation. The latter formulations have been developed to improve tolerability for the patient but may show considerable pharmacokinetic characteristics compared to plain Amphotericin B. more...
Uses
Oral preparations of amphotericin B are used to treat oral thrush; these are virtually nontoxic. The main i.v. use is in systemic fungal infections (e.g. in immunocompromised patients), and in visceral leishmaniasis. Aspergillosis, cryptococcus infections (e.g. meningitis) and candidiasis are treated with amphotericin B. It is also used empirically in febrile immunocompromised patients who do not respond to broad-spectrum antibiotics.
Method of action
As with other polyene antifungals, amphotericin B associates with ergosterol, a membrane chemical of fungi, forming a pore that leads to K+ leakage and fungal cell death. Recently, however, researchers found evidence that pore formation is not necessarily linked to cell death (i.e. Angewandte Chemie Int. Ed. Engl. 2004). The actual mechanism of action may be more complex and multi-faceted.
Side effects
Very often a most serious acute reaction after the infusion (1 to 3 hours later) is noted consisting of fever, shaking chills, hypotension, anorexia, nausea, vomiting, headache, dyspnea, and tachypnea. This reaction sometimes subsides with later applications of the drug and may in part be due to histamine liberation. An increase in prostaglandin-synthesis may also play a role. Often the most difficult decision has to be made, whether the fever is disease- or drug-related. In order to decrease the likelihood and severity of the symptoms, initial doses should be low and increased slowly. The liposomal preperation obviously has a lower incidence of the syndrome. Acetaminophen, pethidine, diphenhydramine and/or hydrocortisone have all be used to treat or prevent the syndrome, but the prophylactic use of these drugs should be limited.
Nephrotoxicity (kidney damage) is a major issue and can be severe and/or irreversible. It is much milder when amphotericin B is delivered in liposomes (AmBisome). Electrolyte imbalances (e.g. hypokalema and hypocalcemia) may also occur.
Increased liver enzymes and hepatotoxicity up to acute liver failure, several forms of anemia and other blood dyscrasias (leukopenia, thrombopenia), serious cardiac arrhythmias (including ventricular fibrillation), and cardiac failure have also been reported frequently. Skin reactions, including serious forms, are also possible.
Interactions
- Flucytosine : Toxicity of Flucytosine increased and vice versa
- Diuretics or Cisplatin : Increased renal toxicity and incrised risk of hypokalema
- Corticosterioids : Increased risk of hypokalema
- Cytostatic drugs : Increased risk of kidney damage, hypotension and bronchospasms.
- Other nephrotoxic drugs : Increased risk of serious renal damage. Monitor patients closely.
- Foscarnet, Ganciclovir, Tenofovir, Adefovir : Risk of hematological and renal side-effects of Amphotericin B increased.
- Transfusion of Leukocytes : Risk of pulmonal (lung) damage. Space intervalls between the application of Amphotericin B and the transfusion and monitor pulmonal function.
Read more at Wikipedia.org