Over the past ten years, a growing number of articles have been published about lung disorders due to several drugs. [1] Most of them were anecdotal and related to single cases. In some reports, bronchoalveolar lavage (BAL) cell findings were mentioned, but the course of alveolitis over time was not studied. Sometimes the criteria on which diagnosis was established also represented a puzzling problem.
We report herein on BAL cell data in a series of 19 patients on whom several findings seemed consistent with the diagnosis of drug-associated pneumonitis. We focused our work on the changes in alveolar cell profile at the time of hospital admission, changes observed over time in repeated lavages after drug treatment cessation, and the course of these changes after resumption of treatment with the drug implicated.
METHODS
Study Populations
Diagnosis of drug-associated pneumonitis was established by the following criteria. (1) Patients had been receiving drug treatment on a more or less long-term basis prior to the onset of lung disorders (Table 1). (2) New bilateral infiltrates appeared on chest roentgenogram. (3) There was no exposure to environmental agents known to be liable to induce lung disorders. (4) No other cause of interstitial pneumonitis was found after repeated clinical and biologic tests. Examination of sputum and BAL fluid detected no viral, fungal, bacterial, or a parasitic pathogens. (5) Congestive heart failure was excluded by clinical evaluation and persistence of infiltrates after forced diuresis. (6) Resolution of pneumonitis occurred after cessation of treatment with the suspected drug. When there were, among associated drugs, substances known to be liable to induce lung damage, the resolution of pneumonitis was observed after withdrawal of treatment with the drug implicated and despite continuation of treatment with the associated drugs (Table 1).
[TABLE DATA OMITTED]
We have carefully scrutinized the problem of the 24 associated drugs. In six patients (cases 3, 8, 9, 13, 15, and 19), only the implicated drug was being administered when the pneumonitis occurred. In a further six patients (cases 4, 5, 6, 7, 10, and 12), treatment with six associated drugs known as liable to induce lung adverse effects (cyclophosphamide, cytarabine [cytosine-arabinoside], bleomycin, hydrochlorothiazide, amiodarone, and vincristine) was not withdrawn, given the clinical condition of the patients. In another two patients (cases 1 and 2), treatment with four associated drugs (cisplatin, fluorouracil, doxorubicin, and etoposide) was stopped, although none of them has been reported so far to have caused pulmonary toxicity. In connection with administration of etoposide, we would only mention that two cases of bronchospasm without alveolitis have possibly been attributed to this drug; [2] likewise, it has been hypothesized [3] that etoposide could have an interaction with methotrexate metabolism and could favor occurrence of methotrexate pneumonitis. In case, 11, cyclophosphamide treatment was withheld: however, this cytotoxic drug has been incriminated as being at the origin of irreversible lung fibrosis, [4] fibrosis quite different from the pneumonitis found in our patient.
Our patients (ten men, nine women) had an average age of 53 [+ or -] 17.5 years. Eight had ever smoked; 11 were smokers (33.5 [+ or -] 15.7 packs/years). They had been treated for various illnesses (malignancies, vasculitides, cardiac diseases, hypertension, bacterial infections, depression, and rheumatoid arthritis) with one of 13 drugs.
At presentation, all patients were symptomatic and complained of dyspnea (15/19), cough (9/19), and mild fever (15/19). In all patients, chest roentgenograms showed bilateral interstitial and/or alveolar opacities in both lungs along with pleural effusion in one (case 17). Pulmonary function tests displayed decreased vital capacity (64 [+ or -] 22 percent predicted value) and [PaO.sub.2] (64 [+ or -] 17.6 mm Hg) in most of them; in seven patients, a marked hypoxia (<50 mm Hg) was present. Mean [FEV/.sub.1]/vital capacity ratio was normal (94 [+ or -] 20 percent predicted value) and mean KCO value was low (1.2 [+ or -] 0.75 mmol/min/kPa/L). Eight patients received corticosteroids and 11 did not.
All patients had BAL at the time of hospital admission. Eight underwent repeated BALs after drug withdrawal and resolution of their pneumonitis: in five patients, a third BAL was done after resumption of drug treatment (provocation test after informed consent).
Thirty-three volunteers acted as control subjects, comparable to patients as to sex and proportion of smokers (24 nonsmokers; nine smokers [40 [+ or -] 10 packs/years]). Their mean age was 30 [+ or -] 7 years.
Bronchoalveolar Lavage
Bronchoalveolar lavage was performed by the usual technique. [5] After fiberoptic examination, the bronchoscope (BF 10, Olympus) was wedged into a subsegment of the right middle lobe (showing opacities) and a total of 200 ml of sterile warm saline solution was instilled in four aliquots of 50 ml. The fluid was recovered by gentle aspiration in a siliconized flask kept at 4[degrees]C. The percentage of fluid recovered was always above 50 percent of fluid instilled. The lavage fluid was filtered through sterile surgical gauze, resuspended, and the total cell count was determined on an aliquot of fluid using a hemocytometer. A differential cell count was done on cytocentrifuge preparations prepared from uncentrifuged lavage fluid and stained with May-Grunwald-Giemsa stain. No morphologic evaluation of alveolar cells was done, as this was beyond the purpose of our study.
Phenotyping of Lymphocytes
Monoclonal antibodies used to identify CD4 and CD8 cell surface antigens on lymphocytes were OKT4 (helper/inducer T lymphocytes, Ortho Diagnostics, Raritan, NJ) and OKT8 (suppressor/cytotoxic T lymphocytes, Ortho). Cells obtained by BAL were washed twice in Hanks balanced salt soloution (Eurobio, Paris, France) and adjusted to a concentration of 2 X [10.sup.7] cells/ml. For each assay, 100 [microliter] of this cell suspension was placed into a 75 X 13-mm tubes, and 10 [microliter] of the monoclonal antibody at the proper dilution was added. Cells were incubated at 4[degrees]C for 30 minutes, washed three times in phosphate-buffered saline solution (pH 7.4) containing 0.1 percent sodium azide (PBS-azide). Ten microliters of fluorescein-conjugated goat anti-mouse IgG (Dynatech, Paris, France) was added. Cells were incubated for 30 minutes at 4[degrees]C, washed three times in PBS-azide, and subsequently resuspended in RPMI-1640 (Eurobio); they were then examined using a fluorescence microscope (Olympus BHB, Tokyo, Japan) equipped with phase-contrast optics. The percentage of fluorescein-labeled lymphocytes was calculated after counting a minimum of 200 lymphocytes per slide.
Statistical Analysis
Values from patients different from the 98 percent confidence interval of the mean were considered abnormal.
All results are expressed as mean [+ or -] standard deviation. Statistical comparisons between patients and controls were made using one-way analysis of variance and Student's t test for unpaired samples. Comparisons between values obtained in patients at the time of hospital admission and values observed after withdrawal of drug treatment were made using Student's test for paired samples. Correlations were tested by linear regression.
RESULTS
BAL CELL Abnormalities at Hospital Admission
Table 2 shows BAL cell individual data from our 19 patients. When compared with data from healthy subjects, total cell count was almost normal and macrophage count mean value was normal in absolute number and lower in proportion, given the increase in other cell types. When calculated in proportion as well as in absolute number, mean values of lymphocytes and neutrophils were found higher than those from controls, whereas the rise in eosinophil mean value was present in proportion, although it did not reach a statistical significance in absolute number. When analyzed individually, these values were high in all but one patient (case 1) for lymphocytes in ten of 19 for neutrophils, and seven of nine for eosinophils.
[TABLE DATA OMITTED]
Overall, in 16 patients whose lymphocytes were phenotyped, there was a significant increase in absolute number in CD4 and CD8 T lymphocytes, more pronounced in the latter. The percentage of CD8 T lymphocytes was raised and the percentage of CD4 T lymphocytes was lowered and the CD4/CD8 lymphocyte ratio was low: these changes were statistically significant. When individually analyzed, CD4 T lymphocyte count and CD8 T lymphocyte count were found significantly high in 10 of 16 and in 16 of 16 patients, respectively; the CD4/CD8 T lymphocyte ratio was low in 14 of 16 patients.
BAL Cell Changes after Cessation of Treatment with
the Incriminated Drug
Two to four months after withdrawal of treatment with the drug implicated, and when their pneumonitis had partially or totally resolved, eight patients underwent repeated BAL (Table 3). In this second BAL, total cell count mean value dropped from 548 [+ or -] 579 cells/[microliter] to 232 [+ or -] 231 cells/[microliter] in a nonsignificant way. An overall significant decrease (in absolute number and proportion) in lymphocyte and CD8 T lymphocyte populations was observed, whereas the increase in CD4 T lymphocyte percentage and in CD4/CD8 T lymphocyte ratio did not reach a significant difference when compard with values obtained at hospital admission. In half of the patients, lymphocyte percentages and CD8 T lymphocyte percentages returned to normal limits. At the same time, there was a rise in macrophage percentage and absolute number (p<0.001). Trivial changes occurred in neutrophil and eosinophil percentages and absolute numbers.
[TABLE DATA OMITTED]
Provocation Test Coupled with BAL
In five patients, two to four months after cessation of drug treatment, a second BAL was done and administration of the suspected drug was resumed for two to four weeks. Subsequently, a third lavage was performed. Changes in lymphocytes and their subsets are shown in Figure 1. In these patients, the percentage of lymphocytes fell significantly at the end of the drug withdrawal period and rose again when drug treatment was resumed. As for variations in lymphocyte subsets and ratio, they paralleled these lymphocyte changes, although only the variation in percentage of CD8 T lymphocyte between the one found at hospital admission and the figure obtained by the end of drug cessation period was statistically significant.
DISCUSSION
In this series of 19 cases, 13 drugs listed in Table 1 were likely to be responsible for pneumonitis.
In the literature, [6] pulmonary toxicity due to five of the 13 drugs incriminated (bleomycin, methotrexate, nitrofurnation, gold salts, and nilutamide) has already been mentioned in 26 BAL-investigated cases (Table 4). We present herein data about BAL from nine patients with pneumonitis associated with one of these five drugs; six of these nine cases have been published previously. [7-10]
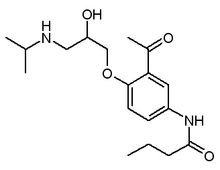
In the case of a further five drugs (accebutolol, [11] azathioprine, [12] propranolol, [13] minocycline, [14] and D-penicillamine [15]), their pulmonary toxicity was recognized many years ago, but no BAL cell data were available. Six instances of BAL data related to these five drugs are presented herein; four of them have been reported previously (cases 11, [16] 12, [17] 9, [18] and 13 [19]).
In four of these patients investigated by BAL, pneumonitis was associated with atenolol (case 14), clomipramine (case 17), and vincristine (cases 7 and 8): to the best of our knowledge, pulmonary toxicity due to these three drugs has never been indicated previously. Nevertheless, these drugs are chemically close to compounds (practolol, [20] imipramine, [21] and vinblastine [22]) whose harmful effects to the lungs have been known for several years.
Features of Alveolitis at Hospital Admission
In only one BAL (case 1), a neutrophil and eosinophil alveolitis was present as was the case for two BALs previously reported; [23] in nine other cases, [23,24] a pure neutrophil alveolitis was found.
In all remaining BALs (18 cases), lymphocyte alveolitis was observed, either pure (in six cases) or associated with neutrophils or eosinophils or with both cell types (Table 4). There was no correlation between the type of alveolitis and the nature of the drug implicated, since the same drug was responsible for different kinds of alveolitis. These results are very similar to those published by different workers.
[TABLE DATA OMITTED]
Moreover, the abnormalities in proportion of lymphocyte phenotypes were close to those observed by others, except two articles related to three cases of methotrexate lung [25] and one case of nitrofurantoin lung [26] in which the CD4/CD8 lymphocyte ratio was increased above 2.
The BAL cell profile described above seems to be very similar to that observed in hypersensitivity pneumonitis due to inhalation of organic dust [27] whose immunologic pathogenesis is well established. [28]
Outcome of Lymphocyte Alveolitis and
Provocation Test
In the four of eight patients who underwent repeated BALs two to four months after cessation of drug treatment, persistence in lymphocyte population abnormalities, although less marked that at the time of hospital admission, should be underlined and is evocative of similar findings in farmer's lung. [29] At that time, partial or total resolution of pneumonitis had occurred.
In five of these patients, the alveolar lymphocyte percentage fell significantly two to four months after treatment with the implicated drug was withdrawn and it rose significantly when drug administration had been resumed for two to four weeks (Fig 1). Such an alveolar lymphocyte course would seem to be an argument in favor of the diagnosis, as it is in hypersensitivity pneumonitis; [30] in these latter diseases, an early neutrophil alveolitis has been observed before alveolar lymphocytosis occurred. Presumably in our patients, neutrophil alveolitis has been overlooked because BAL was done several weeks after the time of drug treatment resumption. In connection with this, it should be pointed out that the provocation test procedure should be avoided with a few drugs, eg, methotrexate [6] and aspirin, [31] to avoid potentially dangerous pulmonary reactions.
Taken together, all these BAL cell data could be considered as being in favor of an immunologic hypersensitivity mechanism that would play a role in the pathogenesis of this lung disorder. Indeed, in our patients, the predominance of lymphocyte populations in BAL at the time of hospital admission, its reduction after withdrawal of drug treatment, and its rise after resumption of drug treatment emphasize the central role of lymphocytes in this iatrogenic disease. The similarities with what has been observed in extrinsic allergic alveolitis are an additional striking feature of drug-induced alveolitis, but they do not preclude intervention of other pathophysiologic factors.
In conclusion, lymphocyte population abnormalities in drug-associated pneumonitis are in no way diagnostic but, in some clinical settings, could represent a hinto diagnosis.
(*1) From the Department of Respiratory Medicine, Hospital Tenon, Paris, France.
(*2) Professor and Head, Department of Respiratory Medicine.
(*3) Assistant Chest Physician.
(*4) Consultant Thoracic Physician.
(*5) Resident.
(*6) Professor of Respiratory Medicine.
Manuscript received april 9; revision accepted June 12.
Reprint requests: Dr. Akoun, Hopital Tenon, 4 rue de la Chine, 75020 Paris, France
REFERENCES
[1] Cooper JAD, White DA, Matthay RA. Drug-induced pulmonary disease, I: cytotoxic drugs; II, noncytotoxic drugs. Am Rev Respir Dis 1986; 133:321-40, 488-505
[2] Tucci E, Pirtoli L. Etoposide-induced hypersensitivity reactions: report of two cases. Chemioterapia 1985; 4:460-62
[3] Zimmerman MS, Ruckdeschel JC, Hussain M. Chemotherapy-induced interstitial pneumonitis during treatment of small cell anaplastic lung cancer. J Clin Oncol 1984; 2:396-405
[4] Akoun G, Mayard C, Touboul JL. Diagnostic value of broncho-alveolar lavage (BAL) in drug induced interstitial pneumonitis. Respiration 1984; 46:71
[5] Godard P, Clot J, Jonquet O, Bosquet J, Michel FB. Lymphocyte subpopulations in bronchoalveolar lavages of patients with sarcoidosis and hypersensitivity. Chest 1981; 80:447-52
[6] Akoun GM, White JP, eds. Treatment-induced respiratory disorders. New York: Elsevier; 1989
[7] Akoun GM, Mayaud CM, Touboul JL, Denis MF, Milleron BJ, Perrot JY. Use of bronchoalveolar lavage in the evaluation of methotrexate lung disease. Thorax 1987; 42:652-55
[8] Akoun GM, Milleron B, El Gharbi N, Malka M. Le lavage bronchoalveolaire dans la pneumopathie a la nitrofurantoine. Sem Hop Paris 1985; 61:2443-46
[9] Akoun GM, Herman DP, Milleron BJ, Mayaud CM, Perrot JY. Bronchoalveolar T-cell subsets in gold lung: evidence for a hypersensitivity reaction. Ches 1985; 87:135-36
[10} Akoun GM, Liote H, Liote F, Gauthier-Rahman S, Kuntz D. Provocation test coupled with bronchoalveolar lavage in diagnosis of drug (nilutamide)-induced hypersensitivity pneumonitis. Chest 1990; 97:495-98
[11] Wood GM, Bolton RP, Muers MF, Losowsky MS. Pleurisy and pulmonary granuloma after treatment with acebutolol. Br Med J 1982; 285:936
[12] Rubin G, Baume P, Vanderber R. Azathioprine and acute restrictive lung disease. Aust NZ J Med 1972; 2:272-74
[13] Saed A. Sclerosing peritonitis and propranolol. Chest 1981; 79:361-62
[14] Ho D, Tashkin DP, Bein ME, Sharma O. Pulmonary infiltrates with eosinophilia associated with tetracycline. Chest 1979; 76:33-6
[15] Camus PH. Manifestations respiratoires associees aux traitements par la D-penicillamine. Rev Fr Mal Respir 1982; 10:7-20
[16] Akoun GM, Herman DP, Mayaud CM, Perrot JY. Acebutolol-induced hypersensitivity pneumonitis. Brit Med J 1983; 286:266-67
[17] Akoun G, Touboul JL, Mayaud C, Gauthier-Rahman S, El Gharbi N. Pneumopathie d'hypersensibilitie a l'acebutolol: donnees en faveur d'un mecanisme immunologique a mediation cellulaire. Rev Fr Allergol 1985; 25:85-6
[18] Akoun G, Mayaud C, Touboul JL, Gauthier-Rahman S, El Gharbi N. La pneumopathie d'hypersensibilite a l'azathioprine: Donnees en faveur d'un mecanisme immunologique. Therapie 1986; 41:73-5
[19] Akoun GM, Milleron BJ, Mayaud CM, Tholoniat D. Provocation test coupled with bronchoalveolar lavage in diagnosis of propranolol-induced hypersensitivity pneumonitis. Am Rev Respir Dis 1989; 139:247-49
[20] Dyer NH, Varley CC. Practolol-induced pleurisy and constrictive pericarditis. Brit Med J 1975; 2:443
[21] Wilson IC, Gambil JM, Sandifer MG. Loeffler's syndrome occurring during imipramine therapy. Am J Psychiatry 1963; 119:892-93
[22] Israel RH, Olson JP. Pulmonary edema associated with intravenous vinblastine. JAMA 1978; 240-1585
[23] White DA, Kris MG, Stover DE. Bronchoalveolar lavage cell populations in bleomycin lung toxicity. Thorax 1987; 42:551-52
[24] Baker G, Eadie M, Levi J, Doe W, Allen D. Cellular analysis of bronchoalveolar lavage from patients receiving combination chemotherapy which include bleomycin. Aust NZ J Med 1983; 13:556-57
[25] White DA, Rankin JA, Stover DE, Gellene RA, Gupta S. Methotrexate pneomonitis: bronchoalveolar lavage findings suggest an immunologic disorder. Am Rev Respir Dis 1989; 139:18-21
[26] Brutinel WM, Martin WJ II. Chronic nitrofurantoin reaction associated with T-lymphocyte alveolitis. Chest 1986; 89:150-52
[27] Leatherman JW, Michael AF, Kronenberg RS, Schwartz BS, Hoidal JR. Evaluation of cell-mediated immunity in the lung by monoclonal antibodies in hypersensitivity pneumonitis and asymptomatic pigeon breeders. Am Rev Respir Dis 1983; 127:62
[28] Pepys J. Hypersensitivity diseases of the lungs due to fungi and organic dusts. New York: Karger; 1969
[29] Cormier Y, Belanger J, Laviolette M. Prognostic significance of lavage lymphocytosis in farmer's lung [abstract]. Am Rev Respir Dis 1986; 133:A241
[30] Fournier E, Tonnel AB, Gosset PH, Wallaert B, Amaisen JC, Voisin C. Early neutrophil alveolitis after antigen inhalation in hypersensitivity pneumonitis. Chest 1985; 88:563-66
[31] Laurent K, de Jonghe M, flemale A, Kimbimbi P, Defrance P, Gillard C. Un nouveau cas de pneumopathie d'hypersensibilite a la salazopyrine. Rev Pneumol Clin 1985; 41:340-43
[32] Court-Fortune I, Fournel P, Vergnon JM, Emonot A. Pneumopathie interstitielle aux sels d'or: interet de l'etude du lavage bronchoalveolaire (LBA). Rev Mal Respir 1988; supply 1:R138
[33] Ettensolm DB, Roberts NJ, Condemi JJ. Bronchoalveolar lavage in gold lung. Chest 1984; 85:569-70
[34] Hauteville D, Vinti H. Simon ALM, Modica C, Abgrall J, Alin R. Les pneumopathies aux sels d'or. Bordeaux Med 1983; 16:457-60
[35] Vivet P, Ameille J, Capron F, Leclerc P, Dessirier JL, Rochemaure J. Pneumopathie interstitielle diffuse au cours d'un traitement par les sels d'or. Ann Med Int 1984; 135;54-8
[36] Costabel U, Schmitz-Schumann M, Matthys H. Bronchoalveolar T-cell subsets in gold lung: evidence for a hypersensitivity reaction. Chest 1985; 87:135-36
[36] Evans RB, Ettensohn DB, Fawaz-Estrup F, Lally EV, Kaplan SR. Gold lung: recent developments in pathogenesis, diagnosis and therapy. Semin Arthritis Rheum 1987; 16:196-205
[38] Ode P, Guy C, Rousset H, Ollagnier M, Guerin JC. Pneumopathie interstitielle d'origine medicamenteuse: la nilutamide (Anandron R). Rev Mal Respir 1988; suppl 1:R137
[39] Seigneur J, Trechot PF, Hubert J, Lamy P. Pulmonary complications of hormone treatment in prostate carcinoma. Chest 1988; 93:1106
[40] Breton JL, Garnier G, Toulouse J, Depierre A. Bronchoalveolar lavage and gold salt-induced pneumonitis. Chest 1985; 87:410
COPYRIGHT 1991 American College of Chest Physicians
COPYRIGHT 2004 Gale Group