Definition
Diabetes mellitus is a condition in which the pancreas no longer produces enough insulin or when cells stop responding to the insulin that is produced, so that glucose in the blood cannot be absorbed into the cells of the body. Symptoms include frequent urination, tiredness, excessive thirst, and hunger. The treatment includes changes in diet, oral medications, and in some cases, daily injections of insulin.
Description
Diabetes mellitus is a chronic disease which causes serious health complications including renal (kidney) failure, heart disease, stroke, and blindness. Approximately 14 million Americans (about 5% of the population) have diabetes. Unfortunately, as many as one-half of them are unaware that they have it.
Background
Every cell in the human body needs energy in order to function. The body's primary energy source is glucose, a simple sugar resulting from the digestion of foods containing carbohydrates (sugars and starches). Glucose from the digested food circulates in the blood as a ready energy source for any cells that need it. Insulin is a hormone or chemical produced by cells in the pancreas, an organ located behind the stomach. Insulin bonds to a receptor site on the outside of cell and acts like a key to open a doorway into the cell through which glucose can enter. Some of the glucose can be converted to concentrated energy sources like glycogen or fatty acids and saved for later use. When there is not enough insulin produced or when the doorway no longer recognizes the insulin key, glucose stays in the blood rather entering the cells.
The body will attempt to dilute the high level of glucose in the blood, a condition called hyperglycemia, by drawing water out of the cells and into the bloodstream in an effort to dilute the sugar and excrete it in the urine. It is not unusual for people with undiagnosed diabetes to be constantly thirsty, to drink large quantities of water, and to urinate frequently as their bodies try to get rid of the extra glucose. This creates high levels of glucose in the urine.
At the same time that the body is trying to get rid of glucose from the blood, the cells are starving for glucose and sending signals to the body to eat more food, thus making patients extremely hungry. To provide energy for the starving cells, the body also tries to convert fats and proteins to glucose. The breakdown of fats and proteins for energy causes acid compounds called ketones to form in the blood. Ketones will also be excreted in the urine. As ketones build up in the blood, a condition called ketoacidosis can occur. This condition can be life threatening if left untreated, leading to coma and death.
Types of diabetes mellitus
Type I diabetes, sometimes called juvenile diabetes, begins most commonly in childhood or adolescence. In this form of diabetes, the body produces little or no insulin. It is characterized by a sudden onset and occurs more frequently in populations descended from Northern European countries (Finland, Scotland, Scandinavia) than in those from Southern European countries, the Middle East, or Asia. In the United States, approximately 3 people in 1000 develop Type I diabetes. This form is also called insulin-dependent diabetes because people who develop this type need to have daily injections of insulin.
Brittle diabetics are a subgroup of Type I where patients have frequent and rapid swings of blood sugar levels between hyperglycemia (a condition where there is too much glucose or sugar in the blood) and hypoglycemia (a condition where there is abnormally low levels of glucose or sugar in the blood). These patients may require several injections of different types of insulin during the day to keep the blood sugar level within a fairly normal range.
The more common form of diabetes, Type II, occurs in approximately 3-5% of Americans under 50 years of age, and increases to 10-15% in those over 50. More than 90% of the diabetics in the United States are Type II diabetics. Sometimes called age-onset or adult-onset diabetes, this form of diabetes occurs most often in people who are overweight and who do not exercise. It is also more common in people of Native American, Hispanic, and African-American descent. People who have migrated to Western cultures from East India, Japan, and Australian Aboriginal cultures are also more likely to develop Type II diabetes than those who remain in their original countries.
Type II is considered a milder form of diabetes because of its slow onset (sometimes developing over the course of several years) and because it can usually be controlled with diet and oral medication. The consequences of uncontrolled and untreated Type II diabetes, however, are the just as serious as those for Type I. This form is also called noninsulin-dependent diabetes, a term that is somewhat misleading. Many people with Type II diabetes can control the condition with diet and oral medications, however, insulin injections are sometimes necessary if treatment with diet and oral medication is not working.
Another form of diabetes called gestational diabetes can develop during pregnancy and generally resolves after the baby is delivered. This diabetic condition develops during the second or third trimester of pregnancy in about 2% of pregnancies. The condition is usually treated by diet, however, insulin injections may be required. These women who have diabetes during pregnancy are at higher risk for developing Type II diabetes within 5-10 years.
Diabetes can also develop as a result of pancreatic disease, alcoholism, malnutrition, or other severe illnesses that stress the body.
Causes & symptoms
Causes
The causes of diabetes mellitus are unclear, however, there seem to be both hereditary (genetic factors passed on in families), and environmental factors involved. Research has shown that some people who develop diabetes have common genetic markers. In Type I diabetes, the immune system, the body's defense system against infection, is believed to be triggered by a virus or another microorganism to destroy the cells in the pancreas that produce insulin. In Type II diabetes, age, obesity, and family history of diabetes play a roll.
In Type II diabetes, the pancreas may produce enough insulin, however, cells have become resistant to the insulin produced and it may not work as effectively. Symptoms of Type II diabetes can begin so gradually that a person may not know that they have it. Early signs are tiredness, extreme thirst, and frequent urination. Other symptoms may include sudden weight loss, slow wound healing, urinary tract infections, gum disease, or blurred vision. It is not unusual for Type II diabetes to be detected while a patient is seeing a doctor about another health concern that is actually being caused by the yet undiagnosed diabetes.
Individuals who are at high risk of developing Type II diabetes mellitus include people who:
- Are obese (more than 20% above their ideal body weight)
- Have a relative with diabetes mellitus
- Belong to a high-risk ethnic population (African-American, Native American, Hispanic, or Native Hawaiian)
- Have been diagnosed with gestational diabetes or have delivered a baby weighing more than 9 lbs (4 kg)
- Have high blood pressure (140/90 mmHg or above)
- Have a high density lipoprotein cholesterol level less than or equal to 35 mg/dL and/or a triglyceride level greater than or equal to 250 mg/dL
- Have had impaired glucose tolerance or impaired fasting glucose on previous testing.
Several common medications can impair the body's use of insulin, causing a condition known as secondary diabetes. These medications include treatments for high blood pressure (furosemide, clonidine, and thiazide diuretics), drugs with hormonal activity (oral contraceptives, thyroid hormone, progestins, and glucocorticorids), and the anti-inflammation drug indomethacin. Several drugs that are used to treat mood disorders (such as anxiety and depression) can also impair glucose absorption. These drugs include haloperidol, lithium carbonate, phenothiazines, tricyclic antidepressants, and adrenergic agonists. Other medications that can cause diabetes symptoms include isoniazid, nicotinic acid, cimetidine, and heparin.
Symptoms
Symptoms of diabetes can develop suddenly (over days or weeks) in previously healthy children or adolescents, or can develop gradually (over several years) in overweight adults over the age of 40. The classic symptoms include feeling tired and sick, frequent urination, excessive thirst, excessive hunger, and weight loss.
Ketoacidosis, a condition due to starvation or uncontrolled diabetes, is common in Type I diabetes. Ketones are acid compounds which form in the blood when the body breaks down fats and proteins. Symptoms include abdominal pain, vomiting, rapid breathing, extreme tiredness, and drowsiness. Patients with ketoacidosis will also have a sweet breath odor. Left untreated, this condition can lead to coma and death.
With Type II diabetes, the condition may not become evident until the patient presents for medical treatment for some other condition. A patient may have heart disease, chronic infections of the gums and urinary tract, blurred vision, numbness in the feet and legs, or slow-healing wounds. Women may experience genital itching.
Diagnosis
Diabetes is suspected based on symptoms. Urine tests and blood tests can be used to confirm a diagnose of diabetes based on the amount of glucose in the urine and blood. Urine tests can also detect ketones and protein in the urine which may help diagnose diabetes and assess how well the kidneys are functioning. These tests can also be used to monitor the disease once the patient is on a standardized diet, oral medications, or insulin.
Urine tests
Clinistix and Diastix are paper strips or dipsticks that change color when dipped in urine. The test strip is compared to a chart which shows the amount of glucose in the urine based on the change in color. The level of glucose in the urine lags behind the level of glucose in the blood. Testing the urine with a test stick, paper strip, or tablet which changes color when sugar is present is not as accurate as blood testing, however it can give a fast and simple reading.
Ketones in the urine can be detected using similar types of dipstick tests (Acetest or Ketostix). Ketoacidosis can be a life-threatening situation in Type I diabetics, so having a quick and simple test to detect ketones can assist in establishing a diagnosis sooner.
Another dipstick test can determine the presence of protein or albumin in the urine. Protein in the urine can indicate problems with kidney function and can be used to track the development of renal failure. A more sensitive test for urine protein uses radioactively tagged chemicals to detect microalbuminuria, small amounts of protein in the urine, which may not show up on dipstick tests.
Blood tests
Fasting glucose test. Blood is drawn from a vein in the patient's arm after a period at least eight hours when the patient has not eaten, usually in the morning before breakfast. The red blood cells are separated from the sample and the amount of glucose is measured in the remaining plasma. A plasma level of 7.8 mmol/L (200 mg/L) or greater can indicate diabetes. The fasting glucose test is usually repeated on another day to confirm the results.
Postprandial glucose test. Blood is taken right after the patient has eaten a meal.
Oral glucose tolerance test. Blood samples are taken from a vein before and after a patient drinks a thick, sweet syrup of glucose and other sugars. In a non-diabetic, the level of glucose in the blood goes up immediately after the drink and then decreases gradually as insulin is used by the body to metabolize, or absorb, the sugar. In a diabetic, the glucose in the blood goes up and stays high after drinking the sweetened liquid. A plasma glucose level of 11.1 mmol/L (200 mg/dL) or higher at two hours after drinking the syrup and at one other point during the two-hour test period confirms the diagnosis of diabetes.
A diagnosis of diabetes is confirmed if there are symptoms of diabetes and a plasma glucose level of at least 11.1 mmol/L, a fasting plasma glucose level of at least 7 mmol/L; or a two-hour plasma glucose level of at least 11.1 mmol/L during an oral glucose tolerance test.
Home blood glucose monitoring kits are available so patients with diabetes can monitor their own levels. A small needle or lancet is used to prick the finger and a drop of blood is collected and analyzed by a monitoring device. Some patients may test their blood glucose levels several times during a day and use this information to adjust their doses of insulin.
Treatment
There is currently no cure for diabetes; the condition, however, can be managed so that patients can live a relatively normal life. Treatment of diabetes focuses on two goals: keeping blood glucose within normal range and preventing the development of long-term complications. Careful monitoring of diet, exercise, and blood glucose levels are as important as the use of insulin or oral medications in preventing complications of diabetes.
Dietary changes
Diet and moderate exercise are the first treatments implemented in diabetes. For many Type II diabetics, weight loss may be an important goal in helping them to control their diabetes. A well-balanced, nutritious diet provides approximately 50-60% of calories from carbohydrates, approximately 10-20% of calories from protein, and less than 30% of calories from fat. The number of calories required by an individual depends on their age, weight, and activity level. The calorie intake also needs to be distributed over the course of the entire day so surges of glucose entering the blood system are kept to a minimum.
Keeping track of the number of calories provided by different foods can become complicated, so patients are usually advised to consult a nutritionist or dietitian. An individualized, easy to manage diet plan can be set up for each patient. Both the American Diabetes Association and the American Dietetic Association recommend diets based on the use of food exchange lists. Each food exchange contains a known amount of calories in the form of protein, fat, or carbohydrate. A patient's diet plan will consist of a certain number of exchanges from each food category (meat or protein, fruits, breads and starches, vegetables, and fats) to be eaten at meal times and as snacks. Patients have flexibility in choosing which foods they eat as long as they stick with the number of exchanges prescribed.
For many Type II diabetics, weight loss is an important factor in controlling their condition. The food exchange system, along with a plan of moderate exercise, can help them lose excess weight and improve their overall health.
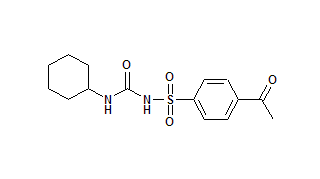
Oral medications
Oral medications are available to lower blood glucose in Type II diabetics. The drugs first prescribed for Type II diabetes are in a class of compounds called sulfonylureas and include tolbutamide, tolazamide, acetohexamide, and chlorpropamide. Newer drugs in the same class are now available and include glyburide, glimeperide, and glipizide. The way that these drugs work is not well understood, however, they seem to stimulate cells of the pancreas to produce more insulin. New medications that are available to treat diabetes include metformin, acarbose, and troglitizone. The choice of the right medication depends in part on the individual patient profile. All drugs have side effects which may make them inappropriate for particular patients. Some for example, may stimulate weight gain or cause stomach irritation, so they may not be the best treatment for someone who is already overweight or who also has stomach ulcers. While these medications are an important aspect of treatment for Type II diabetes, they are not a substitute for a well planned diet and moderate exercise. Oral medications are not effective for Type I diabetes, in which the patient produces little or no insulin.
Insulin
Patients with Type I diabetes need daily injections of insulin to help their bodies use glucose. The amount and type of insulin required depends on the height, weight, age, food intake, and activity level of the individual diabetic patient. Some patients with Type II diabetes may need to use insulin injections if their diabetes cannot be controlled with diet, exercise, and oral medication. Injections are given subcutaneously, that is, just under the skin, using a small needle and syringe. Injection sites can be anywhere on the body where there is looser skin, including the upper arm, abdomen, or upper thigh.
Purified human insulin is most commonly used, however, insulin from beef and pork sources are also available. Insulin may be given as an injection of a single dose of one type of insulin once a day. Different types of insulin can be mixed and given in one dose or split into two or more doses during a day. Patients who require multiple injections over the course of a day may be able to use an insulin pump which administers small doses of insulin on demand. The small battery-operated pump is worn outside the body and is connected to a needle which is inserted into the abdomen. Pumps can be programmed to inject small doses of insulin at various times during the day, or the patient may be able to adjust the insulin doses to coincide with meals and exercise.
Regular insulin is fast-acting and starts to work within 15-30 minutes, with its peak glucose-lowering effect about two hours after it is injected. Its effects last for about 4-6 hours. NPH (neutral protamine Hagedorn) and Lente insulin are intermediate-acting, starting to work within 1-3 hours and lasting up to 18-26 hours. Ultra-lente is a long-acting form of insulin which starts to work within 4-8 hours and lasts 28-36 hours.
Hypoglycemia, or low blood sugar, can be caused by too much insulin, too little food (or eating too late to coincide with the action of the insulin), alcohol consumption, or increased exercise. A patient with symptoms of hypoglycemia may be hungry, cranky, confused, and tired. The patient may become sweaty and shaky. Left untreated, the patient can lose consciousness or have a seizure. This condition is sometimes called an insulin reaction and should be treated by giving the patient something sweet to eat or drink like a candy, sugar cubes, juice, or another high sugar snack.
Surgery
Transplantation of a healthy pancreas into a diabetic patient is a successful treatment, however, this transplant is usually done only if a kidney transplant is performed at the same time. Although a pancreas transplant is possible, it is not clear if the potential benefits outweigh the risks of the surgery and drug therapy needed.
Alternative treatment
Since diabetes can be life-threatening if not properly managed, patients should not attempt to treat this condition without medicial supervision. A variety of alternative therapies can be helpful in managing the symptoms of diabetes and supporting patients with the disease. Acupuncture can help relieve the pain associated with diabetic neuropathy by stimulation of cetain points. A qualified practitioner should be consulted. Herbal remedies may also be helpful in managing diabetes. Although there is no herbal substitute for insulin, some herbs may help adjust blood sugar levels or manage other diabetic symptoms. Some options include:
- Fenugreek (Trigonella foenum-graecum) has been shown in some studies to reduce blood insulin and glucose levels while also lowering cholesterol.
- Bilberry (Vaccinium myrtillus) may lower blood glucose levels, as well as helping to maintain healthy blood vessels.
- Garlic (Allium sativum) may lower blood sugar and cholesterol levels.
- Onions (Allium cepa) may help lower blood glucose levels by freeing insulin to metabolize it.
- Cayenne pepper (Capsicum frutescens) can help relieve pain in the peripheral nerves (a type of diabetic neuropathy)
- Ginkgo (Gingko biloba) may maintain blood flow to the retina, helping to prevent diabetic retinopathy.
Any therapy that lowers stress levels can also be useful in treating diabetes by helping to reduce insulin requirements. Among the alternative treatments that aim to lower stress are hypnotherapy, biofeedback, and meditation.
Prognosis
Uncontrolled diabetes is a leading cause of blindness, end-stage renal disease, and limb amputations. It also doubles the risks of heart disease and increases the risk of stroke. Eye problems including cataracts, glaucoma, and diabetic retinopathy are also more common in diabetics.
Diabetic peripheral neuropathy is a condition where nerve endings, particularly in the legs and feet become less sensitive. Diabetic foot ulcers are a particular problem since the patient does not feel the pain of a blister, callous, or other minor injury. Poor blood circulation in the legs and feet contribute to delayed wound healing. The inability to sense pain along with the complications of delayed wound healing can result in minor injuries, blisters, or callouses becoming infected and difficult to treat. In cases of severe infection, the infected tissue begins to break down and rot away. The most serious consequence of this condition is the need for amputation of toes, feet, or legs due to severe infection.
Heart disease and kidney disease are common complications of diabetes. Long-term complications may include the need for kidney dialysis or a kidney transplant due to kidney failure.
Babies born to diabetic mothers have an increased risk of birth defects and distress at birth.
Prevention
Research continues on ways to prevent diabetes and to detect those at risk for developing diabetes. While the onset of Type I diabetes is unpredictable, the risk of developing Type II diabetes can be reduced by maintaining ideal weight and exercising regularly. The physical and emotional stress of surgery, illness, pregnancy, and alcoholism can increase the risks of diabetes, so maintaining a healthy lifestyle is critical to preventing the onset of Type II diabetes and preventing further complications of the disease.
Key Terms
- Cataracts
- A condition where the lens of the eye becomes cloudy.
- Diabetic peripheral neuropathy
- A condition where the sensitivity of nerves to pain, temperature, and pressure is dulled particularly in the legs and feet.
- Diabetic retinopathy
- A condition where the tiny blood vessels to the retina, the tissues that sense light at the back of the eye, are damaged, leading to blurred vision, sudden blindness, or black spots, lines, or flashing light in the field of vision.
- Glaucoma
- A condition where pressure within the eye causes damage to the optic nerve, which sends visual images to the brain.
- Hyperglycemia
- A condition where there is too much glucose or sugar in the blood.
- Hypoglycemia
- A condition where there is too little glucose or sugar in the blood.
- Insulin
- A hormone or chemical produced by the pancreas, insulin is needed by cells of the body in order to use glucose (sugar), the body's main source of energy.
- Ketoacidosis
- A condition due to starvation or uncontrolled Type I diabetes. Ketones are acid compounds that form in the blood when the body breaks down fats and proteins. Symptoms include abdominal pain, vomiting, rapid breathing, extreme tiredness, and drowsiness.
- Kidney dialysis
- A process where blood is filtered through a dialysis machine to remove waste products that would normally be removed by the kidneys. The filtered blood is then circulated back into the patient. This process is also called renal dialysis.
- Pancreas
- A gland located behind the stomach that produces insulin.
Further Reading
For Your Information
Books
- "Diabetes Mellitus." In Professional Guide to Diseases, 5th ed. Springhouse, PA: Springhouse Corporation, 1995.
- Foster, Daniel W. "Diabetes Mellitus." In Harrison's Principles of Internal Medicine, 14th ed., edited by Anthony S. Fauci, et al. New York: McGraw-Hill, 1998.
- Garber, Alan J. "Diabetes Mellitus." In Internal Medicine, edited by Jay H. Stein, et al. St. Louis: Mosby, 1998.
- Karam, John H. "Diabetes Mellitus & Hypoglycemia." In Current Medical Diagnosis & Treatment 1998, 37th ed., edited by L.M. Tierney, Jr., S.J. McPhee, and M.A. Papadakis. Stamford, CT: Appleton & Lange, 1998.
- Sherwin, Robert S. "Diabetes Mellitus." In Cecil Textbook of Medicine, 20th ed., edited by J. Claude Bennett and Fred Plum. Philadelphia, PA: W.B. Saunders Company, 1996.
- Smit, Charles Kent, John P. Sheehan, and Margaret M. Ulchaker. "Diabetes Mellitus." In Family Medicine, Principles and Practice, 5th ed., edited by Robert B. Taylor. New York: Springer-Verlag, 1998.
Periodicals
- "Trends in the Prevalence and Incidence of Self-Reported Diabetes Mellitus-United States, 1980-1994." Morbidity & Mortality Weekly Report 46 (1997): 1014-1018.
- "Updated Guidelines for the Diagnosis of Diabetes in the US." Drugs & Therapy Perspectives 10 (1997): 12-13.
Organizations
- American Diabetes Association. 1660 Duke Street, Alexandria, VA 22314. (703) 549-1500. Diabetes Information and Action Line (800) DIABETES. http://www.diabetes.org.
- American Dietetic Association. 430 North Michigan Avenue, Chicago, IL 60611. (312) 822-0330. http://www.eatright.org.
- Juvenile Diabetes Foundation International. 120 Wall Street, New York, NY 10005-4001. (212) 785-9595 or (800) JDF-CURE.
- National Diabetes Information Clearinghouse. 1 Information Way, Bethesda, MD 20892-3560. (301) 654-3327.
- National Institutes of Health. National Institute of Diabetes, Digestive and Kidney Diseases. 9000 Rockville Pike, Bethesda, MD 20892. (301) 496-3583. http://www.niddk.nih.gov.
Other
- Centers for Disease Control and Prevention Diabetes Home Page. http://www.cdc.gov/nccdphp/ddt/ddthome.htm.
- Insulin-Dependent Diabetes. National Institute of Diabetes and Digestive and Kidney Diseases. National Institutes of Health, NIH Publication No. 94-2098.
- Noninsulin-Dependent Diabetes. National Institute of Diabetes and Digestive and Kidney Diseases. National Institutes of Health, NIH Publication No. 92-241.
Gale Encyclopedia of Medicine. Gale Research, 1999.