Bronchial hyperresponsiveness is one of the major clinical features of bronchial asthma. We previously reported that oral administration of a selective thromboxane synthetase inhibitor, OKY-046, reduced bronchial hyperresponsiveness to acetylcholine in asthmatic subjects. In this study, the effect of aerosol administration of OKY-046 on bronchial hyperresponsiveness was evaluated in ten inpatients with intrinsic asthma. Acetylcholine inhalation tests were performed before and after four days of inhalation of OKY-046 (100 mg/day). The provocative concentration of acetylcholine producing a 20 percent fall in forced expiratory volume in 1 s (PC20-[FEV.sub.1]) and that causing a 35 percent fall in respiratory conductance (PC35-Grs) were measured as indexes of bronchial responsiveness. There was a significant increase in PC20-[FEV.sub.1] (p<0.001) and PC35-Grs (p<0.02) after inhalation of OKY-046 from 0.79 (GSEM, 1.41) mg/ml and 0.96 (GSEM, 1.35) mg/ml to 1.20 (GSEM, 1.41) mg/ml and 1.74 (GSEM, 1.32) mg/ml, respectively. There was no significant difference in forced vital capacity (FVC), [FEV.sub.1], or respiratory resistance (Rrs) baseline values before and after inhalation of OKY-046. Platelet aggregation was not inhibited by the treatment in other five impatients. Thus, prophylactic administration of aerosol OKY-046 may be available for treatment of asthma by reduction of bronchial hyperresponsiveness. Further studies are needed to determine the optimum dose.
One of the major clinical features of bronchial asthma is the increased bronchial responsiveness to various specific and nonspecific stimuli. Thromboxane [A.sub.2], a metabolite of arachidonic acid, is a potent bronchoconstrictor.[1] We previously reported that oral administration of a selective thromboxane synthetase inhibitor, OKY-046 ([E]-3-(1-imidazolyl-methyl)-phenyl) 1-propenoic acid hydrochloride monohydrate),[2] reduced bronchial hyperresponsiveness to acetylcholine in patients with asthma,[3] and now a double-blinded clinical trial of oral OKY-046 for treatment of asthma is going on in Japan. However, systemic administration of OKY-046 inhibits thromboxane synthesis not only at the bronchopulmonary system, but also at the other systemic organs, especially circulating platelets.[4] Aerosol administration of antiasthmatic drugs, for example [[beta].sub.2]-adrenergic agonists and steroids, is widely used to avoid systemic side effects of oral administration of those. Therefore, if inhaled OKY-046 reduces bronchial hyperresponsiveness in asthmatic patients, it may be more useful for treatment of asthma than oral OKY-046. In this study, we examined the effects of inhaled OKY-046 on the bronchial hyperresponsiveness in patients with asthma.
SUBJECTS AND METHODS
The subjects were six men and four women with asthma admitted to the hospital, with a mean age of 59 years (range, 37 to 77 years). All showed an improvement of 15 percent or more in forced expiratory volume in 1 s ([FEV.sub.1]) after inhalation of 300 [mu]g of albuterol (salbutamol). They all had intrinsic asthma with no familial history of allergic diseases and no increased levels of specific IgE antibodies. The test was performed when their symptoms were mild and stable while they were having oral theophylline retard, oral and aerosol [[beta].sub.2]-stimulants, and mucolytic agents but not steriods. None had experienced viral infection for at least four weeks prior to the study. Six patients were nonsmokers and four patients were smokers who had stopped smoking at the time of hospital admission. Treatment with all medication was stopped at 9 PM the previous day to allow a washout time of 18 hours before the measurement of bronchial responsiveness at 3:00 PM on the test day. All the medication was maintained without any modification during the study period except for the test day.
Bronchial responsiveness was evaluated with acetylcholine. Acetylcholine chloride was dissolved in physiologic saline solution to make solutions of 0.04, 0.08, 0.16, 0.31, 0.63, 1.25, 2.5, 5, 10, and 20 mg/ml. Saline solution and acetylcholine were inhaled from a nebulizer (DeVilbiss 646, DeVilbiss Co, Somerset, Pa) operated by compressed air at 5 L/min. Saline solution was inhaled first for two minutes and [FEV.sub.1] (Autospiror HI-409, Chest Co, Ltd, Japan) and respiratory resistance (Rrs) (MZR-4000, Nihon Koden Co, Ltd, Japan) were measured. If the change in [FEV.sub.1] from the baseline after inhalation of saline solution was 10 percent or less, inhalation of acetylcholine was started. When inhaled saline solution caused a larger change in [FEV.sub.1], the test was stopped or postponed. Acetylcholine was inhaled for two minutes by tidal breathing with a nose clip, and this was followed immediately by measurements of [FEV.sub.1] and Rrs. It was given in increasing concentrations until a fall of 20 percent or more in [FEV.sub.1] and a fall of 35 percent or more in inverse respiratory resistance (Grs) were noted. The measured values were plotted on semilogarithmic graphic paper and the acetylcholine concentrations ([PC.sub.20]-[FEV.sub.1] and [PC.sub.35]-Grs) producing a 20 percent fall in [FEV.sub.1] and a 35 percent fall in Grs were calculated.
OKY-046 was dissolved in physiologic saline solution (12.5 mg/ml). Two milliliters of the OKY-046 solution was inhaled after albuterol inhalation by a jet nebulizer four times a day for three days and only the solution was administered in the morning, at noon, and at 3 PM on the fourth day (test day). Bronchial responsiveness was then measured at 3:30 PM.
A platelet aggregation test was performed before and after four days of inhalation of OKY-046 in five other subjects. Aggregation of platelets was measured photometrically (NKK HEMA TRACER 1, Nikoh Bioscience, Tokyo, Japan), according to the method of Boron.[5] Results were recorded as maximal light transmission, slope value, or both.[6] Some agonists induce platelet aggregation and secretion independent of thromboxane [A.sub.2] synthesis, but with adenosine-diphosphate (ADP) and low dose of collagen, thromboxane [A.sub.2] synthesis is required for secretion and second-wave aggregation. So we use ADP and low dose of collagen as agonists. Intake of drugs that can influence platelet function was prohibited for two weeks before the study and during the study.
Informed consent was obtained from all patients after the purpose of the test had been explained. No information on the test drug and its pharmacologic action was given to the patients or the technical staffs who performed the acetycholine inhalation test. [TABULAR DATA OMITTED]
Data Analysis
Acetylcholine PC20-[FEV.sub.1] and PC35-Grs values were expressed as geometric means with the geometric standard error of the mean (GSEM) expressed as a factor. Values for baeline FVC, [FEV.sub.1], and Rrs were reported as arithmetic means and standard errors of the mean (SEM).
Geometric mean PC20-[FEV.sub.1] and PC35-Grs values were compared by the paired t test. A p value of 0.05 was taken as significant.
RESULTS
Mean baseline values of FVC, [FEV.sub.1], and Rrs are shown before and after the administration of aerosol OKY-046 in Table 1. There was no significant difference in the FVC, [FEV.sub.1], or Rrs baseline values before and after inhalation of the drug.
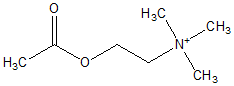
The PC20-[FEV.sub.1] and PC35-Grs values before and after four days of inhalation of OKY-046 are shown in Figure 1. There was a significant increase in PC20-[FEV.sub.1] (p<0.001) and PC35-Grs (p<0.02) after the administration from 0.79 (GSEM 1.41) mg/ml and 0.96 (GSEM 1.35) mg/ml to 1.20 (GSEM 1.41) mg/ml and 1.74 (GSEM 1.32) mg/ml.
Table 2 shows the results of ADP and low-dose collagen induced platelet aggregation study before and after four days of inhalation of OKY-046. The aggregability of platelets of five subjects was not affected by the inhalation.
There were no adverse effects, throat irritation, gastrointestinal symptoms, bleeding tendency, or skin eruptions, from inhaled OKY-046.
DISCUSSION
Thromboxane synthetase inhibitors have been found to suppress bronchoconstriction caused by various bronchoconstrictive agents (histamine, serotonin, acetylcholine, bradykinin, and prostaglandin [F.sub.2[alpha]]) in guinea pig tracheal strips.[7] A selective thromboxane synthetase inhibitor, OKY-046, has been shown to suppress airway anaphylaxis induced by antigen inhalation[8] and bronchoconstriction caused by leukotriene [C.sub.4], a component of slow-reacting substance of anaphylaxis[9,10] in guinea pigs in vivo.[11] Furthermore, Aizawa and coworkers[12] reported that OKY-046 inhibited the increase of airway responsiveness induced by ozone in dogs. From these animal experiments, thromboxane [A.sub.2] is thought to be involved in bronchial asthma, especially in bronchial hyperresponsiveness.
Clinically, we showed that bronchial hyperresponsiveness to acetylcholine was reduced by oral administration of OKY-046 (800 mg/day) in patients with bronchial asthma, whereas baseline pulmonary function was not altered.[3] It has been our hypothesis that a subthreshold dose of thromboxane [A.sub.2], which has no effect on bronchomotor tone per se, may be involved in bronchial hyperresponsiveness in asthma. We[13] recently demonstrated that bronchial responsiveness could be potentiated by a subthreshold dose of a thromboxane [A.sub.2] minetic, [STA.sub.2].[14] Consequently, inhibition of thromboxane [A.sub.2] is expected to be a useful method for control of asthma. In practice, oral OKY-046 (400 mg/day) has proved to have an excellent antiasthmatic effect by multicenter double-blinded clinical trials in Japan (the delegate, Terumasa Miyamoto).
However, systemic administration of OKY-046 inhibits thromboxane synthesis not only at the bronchopulmonary system, but also at the other systemic organs, especially circulating platelets.[4] The concentration of OKY-046 that gave a 50 percent inhibition ([IC.sub.50]) of thromboxane synthetase in rabbit platelets was 1.1 x [10.sup.-8] mol/L; the values for cyclooxygenase and prostaglandin [I.sub.2] synthetase were more than 1 x [10.sup.-4] mol/L and no inhibitory effect was seen at 1 x [10.sup.-3] communication from Arao Ujiie, Kissei Pharmaceutical Co Ltd). When given orally to healthy adults, 25 mg of OKY-046 suppressed the ability of blood platelets to synthesize thromboxane [A.sub.2] while with higher doses (200 to 400 mg) this suppression lasted for more than 12 hours and after the drug had disappeared from the blood.[4] Such an effect is unfavorable as a side effect, for example, systemic bleeding tendency. If aerosol administration of OKY-046 is as effective as systemic administration of the drug, it should be favorable. Practically, aerosol administration of antiasthmatic drugs, for example [[beta].sub.2]-adrenergic agonists and steroids, is widely used to avoid systemic side effects of oral administration of those. In our guinea pig experiment (unpublished data), inhalation of OKY-046 had strong inhibitory effect on the bronchoconstriction induced by both intravenous and aerosol administration of leukotriene [C.sub.4].
In our previous study,[3] single inhalation of OKY-046 (30 mg) failed in reducing bronchial hyperresponsiveness in asthmatic patients while four days of oral administration of the drug (800 mg/day) significantly inhibited bronchial hyperresponsiveness. We thought that lack of dose or duration of the administration might be responsible for the failure of inhaled OKY-046. This study was designed to examine whether or not four days of inhalation of OKY-046 (100 mg/day) can attenuate bronchial hyperresponsiveness in asthmatic subjects. In the results, four days' inhalation of OKY-046 significantly reduced bronchial hyperresponsiveness but did not improve baseline pulmonary functions. Since this study is not a placebo-controlled study, it might be claimed that placebo effect of OKY-046 inhalation and/or reproducibility of measurement of bronchial hyperresponsiveness could influence the results. All the subjects were used to receiving inhalation of drugs, because they were inpatients and had been given albuterol by a jet nebulizer four times a day for more than one month before the study. In addition, single inhalation of OKY-046 had no effect on bronchial hyperresponsiveness.[3] On the other hand, the acetylcholine provocation test has been recognized to have excellent reproducibility while histamine provocation reduces bronchial responsiveness not only to histamine but also to methacholine in asthmatic subjects.[15] Consequently, we consider that the attenuating effect of four days of inhalation of OKY-046 on bronchial hyperresponsiveness observed in this study is significant.
Systemic administration of OKY-046 strongly inhibits thromboxane [A.sub.2] synthesis at all systemic organs, especially circulating platelets.[4] This effect is unfavorable when the drug is given for treatment of asthma. We examined platelet aggregation before and after aerosol administration of OKY-046 to confirm that systemic side effects of the drug can be avoided by the inhalation. Aggregation of platelets induced by ADP or collagen was not suppressed by inhalation of OKY-046.
In conclusion, prophylactic administration of aerosol OKY-046 may be available for treatment of asthma because of inhibition of antigen-induced bronchoconstriction and reduction of bronchial hyperresponsiveness. However, the degree of the reduction investigated in this study is small compared with that noted with oral administration of the drug.[3] Further studies are needed to determine the optimum dose of inhaled OKY-046.
REFERENCES
[1] Svensson J, Strandberg K, Tuvemo T, Hamberg M. Thromboxane [A.sub.2]: effects on airway and vascular smooth muscle. Prostaglandins 1977; 14:425-36
[2] Naito J, Komatsu H, Ujiie A, Hamano A, Kubota T, Tsuboshima M. Effects of thromboxane synthetase inhibitors on aggregation of rabbit platelets. Eur J Pharmacol 1983; 91:41-8
[3] Fujimura M, Sasaki F, Nakaktsumi Y, Takahashi Y, Hifumi S, Taga K, et al. Effects of a thromboxane synthetase inhibitor (OKY-046) and a lipoxygenase inhibitor (AA-861) on bronchial responsiveness to acetylcholine in asthmatic subjects. Thorax 1986; 41:955-59
[4] Ito T, Ogawa K, Sakai K. Effects of a selective inhibitor of thromboxane synthetase in humans. Adv Prostaglandin Thromboxane Leukotriene Res 1983; 11:245-50
[5] Boron GVR. Aggregation of blood platelets by adenosien diphosphate and its reversal. Nature 1962; 194:927-29
[6] Jenkins CSP, Meyer D, Dreyfus MD, Larrieu MJ. Willebrand factors and ristocetin: mechanism of ristocetin-induced platelet aggregation. Br J Haematol 1974; 28:561-78
[7] Kitamura S, Ishihara Y, Takaaaku F. Effect of thromboxane synthetase inhibitors (OKY-046, OKY-1580) on the action of bronchoactive agents in guinea pig tracheal strips and on arachidonate metabolism in guinea pig lung lobes. Postaglandins Leukotrienes Med 1984; 14:341-50
[8] Fujimura M, Koshino K, Nishioka S, Matsuda T. Involvement of thromboxane [A.sub.2] in SRS-A mediated bronchoconstriction induced by aerosol antigen in the guinea pig. Kokyu 1984; 3:1066-71
[9] Murphy RC, Hammarstrom S, Samuelsson B. A slow reacting substance from murine mastocytoma cells. Proc Natl Acad Sci USA 1979; 76:4275-79
[10] Samuelsson B, Hammarstrom S. Nomenclature for leukotrienes. Prostaglandins 1980; 19:645-48
[11] Fujimura M, Miyake Y, Uotani K, Kanamori K, Matsuda T. Secondary release of thromboxane [A.sub.2] in aerosol leukotriene [C.sub.4]-induced bronchoconstriction in guinea pigs. Prostaglandins 1988; 35:427-37
[12] Aizawa H, Chung KF, Leikauf GD, Ueki I, Bethel RA, O'Byrne PM, et al. Significance of thromboxane generation in ozone-induced airway hyperresponsiveness in dogs. J Appl Physiol 1985; 59:1918-23
[13] Fujimura M, Saito M, Kurashima K, Miyake Y, Sakamoto S, Matuda T. Bronchoconstrictive properties and potentiating effect on bronchial responsiveness of inhaled thromboxane [A.sub.2] analogue ([STA.sub.2]) in guinea pig. J Asthma 1989; 26:237-42
[14] Katsura M, Miyamoto T, Hamaanaka N, Kondo K, Terada T, Ohgaki Y, et al. In vitro and in vivo effects of new powerful thromboxane antagonists (3-alkylamino pinane derivatives). Adv Prostaglandin Thromboxane Leukotriene Res 1983; 11:351-57
[15] Manning PJ, O'Byrne PM. Histamine Bronchoconstriction reduces airway responsiveness in asthmatic subjects. Am Rev Respir Dis 1988; 137:1323-25
COPYRIGHT 1990 American College of Chest Physicians
COPYRIGHT 2004 Gale Group