With the aging of the population, the number of diagnostic and interventional procedures in cardiac catheterization laboratories and radiology departments has steadily increased. (1) Use of contrast material during angiographic procedures may lead to acute renal insufficiency, prolonged hospital stays, and even death. (2-4) Strategies to prevent the effects of contrast nephrotoxicity have met with limited or no success. These strategies include the use of theophylline, furosemide, mannitol, low-dose dopamine, adenosine, calcium antagonists, atrial natriuretic peptide, and inhibitors of oxygen-free radicals. (5-11)
To date, hydration with 0.45% sodium chloride solution before angiographic procedures has been the most effective approach. (7,9) Two agents, acetylcysteine and fenoldopam, have recently shown promise in reducing the potential for contrast-induced nephrotoxic effects. (12-16) In this article, we describe these effects, which patients are at greatest risk for them, and current measures to prevent their occurrence. We also discuss the indications, actions, and adverse effects of acetylcysteine and fenoldopam and the nursing considerations for patients given these agents to prevent contrast-induced renal complications.
Pathogenesis of Contrast--Induced Nephrotoxic Effects
Contrast-induced nephrotoxic effects are generally defined as an increase greater than 0.5 mg/dL (44 [micro]mol/L) in the serum level of creatinine that occurs within 48 hours after injection of contrast material. (5) Patients with elevated levels of creatinine have an increased risk for contrast-induced nephrotoxic effects after angiographic procedures. For example, 30% of patients with baseline creatinine levels of 1.5 mg/dL (133 [micro]mol/L), in women, and 2.0 mg/dL (177 [micro]mol/L), in men, experienced nephrotoxic effects after angiography, (5) whereas only 2% of patients with baseline levels less than 1.5 mg/dL (133 [micro]mol/L) did. (3,4) The creatinine level usually peaks 4 to 5 days after administration of contrast material and returns to baseline within 5 days of the peak effect. (7) The renal dysfunction can persist for up to 3 weeks after the procedure. (8)
Besides serum creatinine, other measures used to determine renal function include glomerular filtration rate (GFR) and creatinine clearance. (9,17) GFR, which decreases as serum levels of creatinine increase, is normally about 120 mL/min in men and 95 mL/mm in women. (9) The rate is directly affected by patients' age, muscle mass, protein intake, and sex. Although the serum level of creatinine is generally an adequate measure of GER, it may not be an accurate indication in older patients, women, or patients with markedly reduced muscle mass. (9,17) In these patients, relatively small increases in serum level of creatinine may actually reflect marked reductions in GFR. (9) Alternatively, creatinine clearance can be used to determine GFR. However, this calculation requires collecting a 24-hour urine sample, a step that has some drawbacks in the acute care setting. Normal creatinine clearance is 85 to 135 mL/min (1.422.25 mL/s). A creatinine clearance less than 40 mL/min (<0.67 mL/s) indicates marked renal dysfu nction. (9)
Although reversible in most cases, contrast-induced nephrotoxic effects are the third leading cause of acute renal failure in hospitalized patients.9 Patients who have an increase in serum level of creatinine greater than 5 mg/dL (>442 [micro]mol/L) may require dialysis. (7,11) Repeated nephrotoxic injury (eg, a prolonged hypotensive event or multiple administrations of contrast material) increases the potential for contrast-induced nephrotoxic effects. (6,8) In-hospital mortality related to renal injury is directly proportional to increases in serum level of creatinine for all causes of renal failure. The mortality rate ranges from 3.8% when the increase is between 0.5 mg/dL (44 [micro]mol/L) and 0.9 mg/dL (80 [micro]mol/L) to as much as 64% when the increase is more than 3 mg/dL (265 [micro]mol/L). (6,8)
Two vasoactive substances, prostacyclin and endothelin, are directly implicated in contrastinduced nephrotoxic effects." (6,7) Contrast media stimulate the reninangiotensin cascade, leading to a block in the renal synthesis of the vasodilator prostacyclin. (6,7,12,18) Endothelin, an endogenous vasoconstrictor produced in endothelial cells, is secreted as a direct result of the administration of contrast media. Blood levels of endothelin are lower when low molecular weight media and/or lesser amounts of regular media are administered. (7) Levels of endothelin at baseline and after procedures that require contrast material are higher in patients who have preexisting renal insufficiency. (7)
In a study (2) of 3695 patients who underwent coronary interventional procedures requiring administration of contrast material, the incidence of acute renal failure was 144.6 per 1000 cases (14.4%), and in 7.7 per 1000 cases (0.77%), dialysis was required. No patient with a creatinine clearance less than 47 mL/min (<0.78 mL/s) required dialysis. Of those patients who received 100 mL or less of contrast material, none required dialysis. The in-hospital mortality of the patients who needed dialysis was 35.7%, with a 2-year survival rate of 18.8%. McCullough et a1 (2) stated that despite the overall low necessity for dialysis in patients given contrast material (<1%), dialysis was associated with a relatively high mortality rate.
In a study (3) of 439 patients undergoing coronary angiography who had preexisting chronic renal insufficiency, defined as a baseline serum creatinine level of 1.8 mg/dL or greater ([greater than or equal to]159 [micro]mol/L), 161 patients (37%) had an increase of 25% or more in the serum level of creatinine within 48 hours of the procedure, and 31 (7.1%) required hemodialysis. The in-hospital mortality rate was 22.6%. Four patients remained on long-term dialysis after discharge from the hospital. At the end of 1 year, 17 patients survived, 3 of whom still required long-term dialysis. (3)
Contrast Media
Both forms of contrast media (ionic, high molecular weight and nonionic, low molecular weight) induce osmotic diuresis by inhibiting sodium and water reabsorption and are excreted unchanged in the urine." In high-risk patients, the prevalence of contrast-induced nephrotoxic effects is greater with ionic media than with nonionic media." Nonionic media are preferred, however, for all patients undergoing radiological procedures because of the lower risk of adverse drug reactions. These reactions include nausea and vomiting, a sensation of burning at the intravenous or intra-arterial site, and allergic reactions such as itching, urticaria, hemodynamic instability, bronchospasm, and cardiopulmonary arrest. (18)
The greater the volume of contrast medium administered, the greater is the risk for nephrotoxic effects. (5) Recommended volume limits vary with the procedure and range from 100 mL for excretory urography to 250 mL for arteriography of the aorta and major branches (volumes given are for adults only). (20) Administration of a second dose of contrast medium within 48 hours, whether ionic or not, also adds considerably to the risk. (5-9)
Pathophysiology of Contrast-Induced Nephrotoxic Effects
After administration of contrast material, renal vasodilatation occurs, which can persist up to 20 minutes, and then vasoconstriction, which can persist up to 2 hours (6,7) (Figure). The vasoconstriction primarily affects the renal medulla, which normally receives only 10% to 20% of renal blood flow; the remaining blood flow is preferentially to the cortex. (6,7) Even mild alterations in blood flow and pressure can cause medullary ischemia. The medulla also contains the loop of Henle, where oxygen-demanding active transport of sodium occurs. Oxygen consumption increases with the administration of contrast material, especially in medullary cells, further contributing to an imbalance in oxygen supply and demand. (10)
The restricted renal blood flow results in reduced availability of nitric oxide. Normal nitric oxide levels contribute to vasodilatation and enhanced oxygen supply to the tissues (10); thus, nitric oxide is necessary for the maintenance of renal blood flow after any prolonged ischemia. Without nitric oxide, GFR and the renal excretion of sodium and water are impaired, and the ischemia becomes self-perpetuating, further contributing to acute tubular necrosis. (12,21)
Katholi et a1 (22) determined that administration of contrast material can cause direct toxic injury of the kidneys because of the release of oxygen-free radicals. The release of free radicals can both cause and perpetuate contrast-induced nephrotoxic effects. (7,22,23) Free radicals are unbound electrons produced by oxidation; they are generated at sites of local ischemia/reperfusion, principally in the heart, lungs, brain, and kidneys. (21,22) The principal reactive oxygen radicals implicated in contrast-induced nephrotoxic effects are hydroxyl ion, superoxide, and hydrogen peroxide. In sufficient quantities, oxygen-free radicals upset the structural and functional stability of molecules involved in metabolic processes and contribute to the destruction of cell membranes and the breakdown of intracellular proteins and DNA. For example, glutathione, a protein that plays a key role as a natural antioxidant, is rapidly depleted in areas where excessive amounts of tissue destruction occur, further contributing t o oxidative damage. (7,22-24)
Depending on the degree of injury to the kidney, contrast-induced nephrotoxic effects are a combination of direct toxic damage, increased renal vascular resistance, renal ischemia and tissue necrosis, decreased GFR, increased levels of serum creatinine, and decreased creatinine clearance. (7,21,25,26) Evidence of acute renal insufficiency occurs within 24 to 48 hours after administration of contrast material. (7,9,10) Levels of uric acid and nitric acid increase, and sludging of erythrocytes occurs in the kidneys. (6,7,23) In most cases, but not all, oliguria occurs (urinary output <400 mL/24 h). (8) Urinalysis reveals renal tubular epithelial cells, granular casts, and decreased sodium excretion. (9)
Risk Factors and Prevention Strategies
The greatest risk factor for contrast-induced nephrotoxic effects (Table) is preexisting renal insufficiency (defined as serum creatinine level >1.5 mg/dL [>135 [micro]mol/L]). (6,7) Diabetes mellitus, particularly in patients with renal insufficiency, is the second leading risk factor. (4-9) In patients with diabetes, even mild renal insufficiency leads to a marked reduction in renal blood flow, particularly to the renal medulla, and altered responses to vasoactive substances. (67) Use of met-formin is often discontinued 2 days before any procedure that requires contrast material and is restarted only when creatinine levels reach 1.5 mg/dL (135 [micro]mol/L) or less after the procedure. Metformin, a common diabetes medication, is associated with an increased risk for lactic acidosis in patients with preexisting renal insufficiency. (27)
Volume depletion due to prolonged periods in which patients are given nothing by mouth, use of loop diuretics, and loss of fluid during the radiological procedure increase the risk for contrast-induced nephro-toxic effects. For this reason, diuretics are usually withheld the day of the procedure. Many angiographic procedures are long, requiring considerable amounts of contrast material, so monitoring of patients and fluid replacement are critical. (5-10)
Currently, the most effective preventive measure is intravenous infusion of 0.45% sodium chloride solution before the radiological procedure. (7,9) The recommended rate is 1 mL per kilogram of body weight administered for 8 to 12 hours before the procedure and continued for 4 hours after the procedure, unless the patient is nauseated. If nausea occurs, the solution may be infused for a longer period. (7) Hydration with 0.45% sodium chloride solution before the radiological procedure increases renal levels of prostaglandin, which in turn may increase medullary blood flow. (7) If a patient has overt congestive heart failure, the rate of administration of the solution may be decreased. For outpatients, intravenous fluids are started at the aforementioned rate as soon as possible and are continued for 4 hours after the procedure.
Other groups at risk include the elderly; patients with New York Heart Association class III or IV congestive heart failure; patients with multiple myeloma, preexisting hypertension, or acute liver failure (5-9); and patients taking certain medications. Angiotensin-converting enzyme inhibitors and nonsteroidal anti-inflammatory drugs have been implicated in contrast-induced nephrotoxic effects. Even though they block the vasoconstricting effect of angiotensin II, angiotensin-converting enzyme inhibitors may actually decrease blood pressure and blood flow to the kidneys in certain at-risk patients. (59) Dosing and administration of nephrotoxic agents such as aminoglycosides should be used with extreme caution in patients who require contrast material who have evidence of renal insufficiency. (6,7,13,28)
Finally, any patient with more than a single risk factor is at greater overall risk for contrast-induced nephrotoxic effects. (5-7,9,28,29) With the increase in the number of older patients and the associated increases in comorbid conditions, this increase in risk is not unusual in any acute care setting.
Acetylcysteine
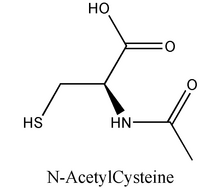
Acetylcysteine is an N-acetyl derivative of the amino acid L-cysteine. Under the more commonly known trade names Mucomyst and Mucosil, acetylcysteine has long been used as a mucolytic agent in patients with pulmonary disease because of its ability to enhance the breakup of mucoproteins in respiratory secretions. The greater the concentration of mucoproteins, the greater is the viscosity of sputum. (27,30)
Mechanism of Action
Acetylcysteine can act as an antioxidant or as a scavenger of free oxygen radicals (25) in situations in which ischemic and/or toxic damage to vital organs has occurred. As occurs in contrast-induced nephrotoxic effects, ischemia-reperfusion injury results in cell damage; antioxidants play a crucial role in preventing or resolving the damage. (12) Antioxidants prevent the bonding of oxygen free radicals with other unbound radicals and thus reduce cell damage. (12)
Acetylcysteine forms a sulfhydryl compound to enhance and complete oxidation through normal pathways. The oxidation in turn replenishes glutathione and sulfhydryl stores and results in a reduction in the formation of oxygen-free radicals, leading to repair of cellular functions. (13) Additionally, acetylcysteine may combine with nitric oxide to form S-nitrosothiol, a powerful vasodilator, which improves blood flow to the kidneys and limits the cellular stress response. (13,23)
Other uses for acetylcysteine include treatment of acetaminophen overdose, hepatorenal syndrome, and toxic effects due to cisplatin (a chemotherapy agent). In all cases, acetylcysteine works directly in the liver or kidneys to limit the damage to those organs through the drug's scavenging and vasodilatory effects. (12,13,21,31,32)
Use in Preventing Contrast--Induced Rephrotoxic Effects
With the rationale that oxygen-free radicals and impaired nitric oxide function are implicated in the pathogenesis of contrast-induced nephrotoxic effects, Salom et al (21) and DiMari et al (12) studied the effects of acetylcysteine in animals with artificially induced cessation of renal blood flow. In both studies, animals given acetylcysteine before the cessation of renal blood flow had preserved renal blood flow and function and no permanent renal tissue damage after the procedure. Animals in the control groups all had permanent tissue damage and renal failure.
Tepel et al (13) studied the effects of prophylactic acetylcysteine in humans to determine if its antioxidant properties could limit the adverse effects of contrast material on renal function. Patients were randomly assigned to receive either a placebo or 600 mg of acetylcysteine twice daily both the day before and the day of injection of contrast medium. The 83 patients in the study had a baseline serum level of creatinine greater than 1.2 mg/dL (>106 [micro]mol/L) or a creatinine clearance less than 50 mL/min (<0.83 mL/s) and included patients with and without diabetes mellitus. All of the patients had intravenous hydration with 0.45% sodium chloride solution at a rate of 1 mL/kg per hour and were given low molecular weight contrast material at a standard dose of 75 mL. Overall, 10 (12%) of the 83 patients had an increase of 0.5 mg/dL or more ([greater than or equal to]44[micro]mol/L) in serum creatinine level 48 hours after administration of contrast material, 1 of the 41 patients given acetylcysteine and 9 of the 42 patients given the placebo. Thus, an increase in serum level of creatinine occurred in 2% of the patients given acetylcysteine and in 21% of those given the placebo.
In the Acetylcysteine to Prevent Angiography-Related Renal Tissue Injury trial, (14) 54 patients with "stable" chronic renal failure, defined as creatinine clearance less than 50 mL/min (<0.83 mL/s) or serum creatinine level of 1.4 mg/dL or greater ([greater than or equal to]124 [micro]mol/L) were randomized to receive either 4 doses of 600 mg of acetylcysteine or a placebo. One dose was given before the scheduled cardiac catheterization; the other 3, after the procedure. Contrast-induced nephrotoxic effects were defined as an increase of 0.5 mg/dL or greater ([greater than or equal to] 44 [micro]mol/L) in serum creatinine level or a greater than 25% increase over baseline 48 hours after the catheterization. Of the 54 patients in the study, a total of 15 patients had contrast-induced nephrotoxic effects, 13 (45%) in the group given a placebo and 2 (8%) in the group given acetylcystiene. (14)
Dosing and nursing Considerations
On the basis of these data, acetylcysteine may be given to patients at high risk for contrast-induced nephrotoxic effects: those who have a baseline serum creatinine level of 2.0 mg/dL or greater ([greater than or equal to]177 [micro]mol/L), in men, or 1.5 mg/dL or greater ([greater than or equal to]133 [micro]mol/L), in women, or creatinine clearance less than 40 mL/min (<0.67 mL/s). The current recommended dose is 600 mg orally given twice a day (in the morning and the evening) the day before and the day of a radiological procedure that requires administration of contrast material. (13) Usually, 3 mL of the 20% solution is diluted in 2 to 4 oz (60-120 mL) of a soda of choice to mask the unpleasant odor and taste. (14) The drug can be diluted in water if it is being administered through a nasogastric tube. In order to further mask the odor and taste of the drug, the container can be covered with a lid and patients can be encouraged to drink the medication through a straw. (14) Ice can also be added. Even wit h these measures, patients who have nausea may be unable to tolerate the drug. An alternative method, which has recently been made available, is use of a capsule (600 mg of acetylcysteine per capsule), a form that is much more acceptable to patients.
Fenoldopam
Fenoldopam mesylate (Corlopam) is a benzazepine derivative that acts specifically on the dopamine type 1 receptors located in the mesentery, coronary and peripheral arteries, renal tubules, and renal vasculature. It does not appear to affect the type 2 dopamine receptors; thus, it is considered a "pure" dopamine 1 agonist. (33,34) It is approved by the Food and Drug Administration for short-term (48 hours) use in severe hypertension when rapid, quickly reversible lowering of the blood pressure is necessary. Its antihypertensive effect results in peripheral vasodilatation; renal blood flow is preserved and actually improved by the decrease in renal vascular resistance. (35,36)
Mechanism of Action
Fenoldopam is a catecholamine structurally related to both dobutamine and dopamine but with key differences. Whereas dopamine, particularly when infused at higher doses (ie, >2 [micro]g/kg per minute), can cause shunting of blood away from the kidneys and elevation of renal vascular resistance, (33,35-37) fenoldopam dilates renal afferent and efferent arterioles and increases renal blood flow in both the medulla and the cortex. This action is dose dependent, achieved at doses less than those typically needed to cause peripheral vasodilatation and decrease blood pressure in patients with hypertension. (38) In one trial, (35) renal blood flow was increased by up to 75% when the highest recommended infusion dose of fenoldopam was administered (0.5 [micro]g/kg per minute).
GFR is increased in normotensive and hypertensive patients, whether they have renal insufficiency or not. (34,37,38) In addition, contrast material is actually cleared more rapidly by the nephron in patients receiving fenoldopam. (36) The activity of angiotensin-converting enzyme and the synthesis of renal prostaglandin are unaffected by fenoldopam. (34)
Use in Preventing Contrast-Induced Nephrotoxic0 Effects
By maintaining and/or improving blood flow to the kidneys via its rapid-acting and selective vasodilatory effects, fenoldopam limits the potential for renal impairment associated with administration of contrast material in patients at high risk for nephrotoxic effects. Several studies support its use for this purpose. (33,35,37) The defining criteria for administration are the same as those for acetylcysteine. However, because of its direct effect on the renal vasculature, fenoldopam maybe used in normotensive patients with diabetes who have preexisting renal insufficiency.
In a randomized, double-blind, placebo-controlled, crossover study, Mathur et al (38) administered increasing doses of fenoldopam, from 0.03 to 0.3 [micro]g/kg per minute, or a placebo to 14 randomized normotensive men. At the lowest dose of fenoldopam, renal blood flow was increased but GFR was unchanged. At a dose of 0.1 [micro]g/kg per minute, systolic blood pressure was unchanged, diastolic pressure and heart rate showed minimal changes, and renal blood flow and GFR were preserved. At a dose of 0.3 [micro]g/kg per minute, renal blood flow and GFR were still maintained, but slightly more evident changes in heart rate and diastolic pressure occurred.
Tumlin et al (15) and Chamsuddin et al (16) reported the beneficial effect of fenoldopam in preventing or ameliorating contrast-induced nephrotoxic effects. In the study by Tumlin et al, 45 patients undergoing coronary or peripheral angiography who had evidence of mild to moderate renal insufficiency (serum level of creatinine 2.0-5.0 mg/dL [177-442 [micro]mol/L]) were randomized to receive 0.45% sodium chloride solution alone or in conjunction with fenoldopam at a dose of 0.1 [micro]g/kg per minute. The fenoldopam was infused for 1 hour before the angiographic procedure and was continued for 4 hours after the procedure. At 48 hours after the procedure, 41% of the control group and 21% of the fenoldopam group had nephrotoxic effects. The prevalence was even higher in patients with diabetes: 64% and 33%, respectively. Peak serum creatinine levels at 72 hours were significantly higher in the control group, 3.6 [+ or -] 1.0 mg/dL (328 [+ or -] 88 [micro]mol/L), than in the fenoldopam group, 2.8 [+ or -] 0.35 mg/ dL (248 [+ or -] 31 [micro]mol/L).
To determine the direct effect of fenoldopam on renal function, Chamsuddin et al (16) retrospectively reviewed 28 cases in which patients at high risk for nephrotoxic effects had complex radiological procedures requiring large doses of contrast material. Fenoldopam was started at a rate of 0.1 [micro]g/kg per minute 2 hours before the radiological procedure, increased incrementally in selected cases to 0.5 [micro]g/kg per minute, and continued for at least 4 hours after the procedure. Mean serum creatinine before the procedure was 2.55 mg/dL (225 [micro]mol/L; range 1.6-5.0 mg/dL [141-442 [micro]mol/L]). A total of 16 patients (57%) had a decrease in mean serum creatinine at 24 hours to 2.0 mg/dL (177 [micro]mol/L; range 1.4-5.0 mg/dL [124-442 [micro]mol/L]), 9 (32%) had no change, and 3 (11%) had an increase in serum level of creatinine. In the 3 patients who had an increase in serum level of creatinine, the increase was attributed to events not related to contrast material in 2 patients.
Dosing and nursing Considerations
On the basis of the data reported by Mathur et al, (38) administration of fenoldopam is begun at a rate of 0.1 [micro]g/kg per minute. The lowest recommended dose is 0.05 [micro]g/kg per minute. In patients with preexisting hypertension, the dose can be titrated to 0.5 [micro]g/kg per minute as long as blood pressure parameters are maintained. (16) The medication is infused continuously for 60 to 90 minutes before the injection of contrast material and is continued for 4 hours after the injection if no adverse reactions occur. (7)
Because of its antihypertensive effects, fenoldopam should be used cautiously in conjunction with other antihypertensive agents and/or [beta]-blockers. Hypokalemia should be corrected before administration of fenoldopam is started. Caution should be used in patients with glaucoma or increased intraocular pressure because the drug may aggravate these conditions. (39) Fenoldopam is a sulfite derivative; it should not be used in patients with known sulfite sensitivity. It is not recommended for nursing mothers. In studies in animals, the drug crossed the placental boundary. Fenoldopam does not cross the blood-brain barrier, however, or have a direct effect on the central nervous system. (34)
Nursing considerations are directly related to the vasodilatory effects of fenoldopam. Hypotension can occur within the first 5 minutes of its administration. Blood pressure should be measured 5 minutes after the infusion is started and then every 15 minutes if titrating, or if the patient's condition becomes unstable, and every 30 minutes if the patient remains normotensive and in stable condition. If blood pressure decreases markedly, the infusion should be stopped, a physician should be notified, and measures to support blood pressure (eg, placement in modified Trendelenburg position, rapid infusion of isotonic sodium chloride solution, frequent monitoring of vital signs) should be instituted. (40) The half-life of fenoldopam is 5 minutes, so any adverse effects should be transitory. (39)
Fenoldopam can cause both natriuresis and diuresis. The development of potassium levels less than 3 mEq/L within 6 hours of administration have been reported. (39) Therefore, potassium replacement may be necessary. Monitoring the levels of potassium and other electrolytes and the serum levels of creatinine and urea nitrogen are important nursing considerations in the immediate phase after administration of fenoldopam. (40) Patients should also be educated about and monitored for flushing and headache, common adverse effects of all vasodilators. Dose-related tachycardia may occur, particularly with higher doses, because of the vasodilatation. (39)
Choice of Therapy
In determining whether acetyl-cysteine or fenoldopam should be used, the following are considered:
* Nothing-by-mouth status: Use of acetylcysteine is precluded for patients who can take nothing by mouth for reasons other than just preparation for the radiological procedure.
* Cost: Acetylcysteine costs less than $2.50 per treatment, whereas fenoldopam costs $400.
* Baseline blood pressure: Patients with blood pressure less than 100 mm Hg before the procedure requiring contrast material are not candidates for fenoldopam.
* Time: Emergent situations require fenoldopam because administration of acetylcysteine must be started the day before the radiological procedure.
* Sulfite sensitivity: Fenoldopam cannot be used in patients with sensitivity to sulfites.
* Diabetes mellitus: Because of its more direct vasodilatory effect, fenoldopam is preferred over acetylcysteine in patients with diabetes mellitus who are normotensive.
Summary
The prevalence of nephrotoxic effects after administration of contrast material is increasing. Other than good hydration before the radiological procedure, previous attempts to prevent the effects of contrast nephrotoxicity have been ineffective. Fenoldopam and acetyl-cysteine are possible preventive medications being used in selected cases. Both drugs await approval from the Food and Drug Administration for use in preventing contrast-induced nephrotoxic effects. The onset of action of the 2 drugs differs, and each drug has different pharmacological actions. Determining which drug should be used is based on whether the patient can be given anything by mouth, whether the procedure is emergent, cost, degree of renal insufficiency before the radiological procedure, blood pressure, and whether the patient has diabetes. Further studies will determine if one drug is preferred over the other or if their combined use is the preferred approach for high-risk patients. Future options could include an intravenous form of acetylcysteine and an oral form of fenoldopam.
Acknowledgments
The authors thank Marc H. Weiner, MD, Laurence E. Carroll, Mo, and Leigh Shuman, MD, for their assistance in preparing the manuscript.
References
(1.) King SB III. The development of interventional cardiology. J Am Coil Cordial. 1998;31(4 suppl B):64B-88B.
(2.) Mccullough PA, Wolyn R Rocher LL, Levin RN, O'Neill WW. Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality. Am J Med. 1997;103:368-375.
(3.) Gruberg L, Mintz GS, Mehran R, et al. The prognostic implications of further renal function deterioration within 48 h of interventional coronary procedures in patients with pre-existent chronic renal insufficiency. J Am Call Cardiol. 2000;36:1542-1548.
(4.) Parfrey PS, Griffiths SM, Barrett BJ, et al. Contrast material-induced renal failure in patients with diabetes mellitus, renal insufficiency, or both: a prospective controlled study. N Engl J Med. 1989;32t1:143-149.
(5.) Porter GA. Contrast-associated nephropathy. Am J Cardiol 1989;64:22E-26E.
(6.) Lepor NE. Radiocontrast nephropathy: the dye is not cast. Rev Cardiovasc Med. 2000;1:43-54.
(7.) Solomon R. Radiocontrast-induced nephropathy. Semin Nephrol. 1998:18:551-557.
(8.) Berns AS. Nephrotoxicity of contrast media. Kidney Int. 1989;36:730-740.
(9.) Waybill MM, Waybill PN. Contrast media-induced nephrotoxicity: identification of patients at risk and algorithms for prevention. J Vasc Interv Radiol. 2001;12:3-9.
(10.) Gerlach AT, Pickworth KK. Contrast medium-induced nephrotoxicity: patho-physiology and prevention. Pharmacotherapy. 2000;20:540-548.
(11.) Bellomo R, Chapman M, Finfer S, Hickling K, Myburgh J. Low-dose dopamine in patients with early renal dysfunction: a placebo-controlled randomised trial. Australian and New Zealand Intensive Care Society (ANZICS) Clinical Trial Group. Lancet. 2000;356:2139-2143.
(12.) DiMari J, Megyesi J, Udvarhelyi N, Price P. Davis R, Safirstein R. N-acetyl cysteine ameliorates ischemic renal failure. Am J Physiol. 1997;272(3 pt 2):F292-F298.
(13.) Tepel M, van der Giet M. Schwarzfeld C, Laufer U, Liermann D, Zidek W. Prevention of radiographic-contrast-agent-induced reductions in renal function by acetylcysteine. N Engl J Med. 2000;343:180-184.
(14.) Diaz-Sandoval LJ, Kosowaky BD, Losordo OW. Acetylcysteine to prevent angiography-related renal tissue injury (the APART trial). Am J Cardiol. 2002;89:356-358.
(15.) Tumlin JA, Wang A. Murray PT, Mathur VS. Fenoldopam mesylate blocks reductions in renal plasma blood flow after radiocontrast dye infusion: a pilot trial in the prevention of contrast nephropathy. Am Heart J. 2002;143:894-903.
(16.) Chamsuddin AA, Kowalik KJ, Bjarnason H, et al. Using a dopamine type 1A receptor agonist in high-risk patients to ameliorate contrast-associated nephropathy. A JR Am J Roentgenol. 2002;179:591-596.
(17.) Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: anew prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461-470.
(18.) Lasser EC. Contrast media for urography: In: Pollack HM, ed. Clinical Urograplzy: An Atlas and Textbook of Urological Imaging. Vol. 1. Philadelphia, Pa: WB Saunders Co; 1990:23-36.
(19.) Moore RD. Steinberg EP, Powe NR, et al. Nephrotoxicity of high-osmolality versus low-osmolality contrast media: randomized clinical trial. Radiology. 1992:182:649-655.
(20.) Visipaque [package insert]. Princeton, NJ: Nycomed Amerisham Imaging; 2000.
(21.) Salom MG, Ramerez P. Carbonell LF, et al. Protective effect of N-acetyl-L-cysteine on the renal failure induced by inferior cava occlusion. Transplantation. 1998;65:1315-1321.
(22.) Katholi RE, Woods WT Jr, Taylor GJ, et al. Oxygen free radicals and contrast nephropathy. Am J Kidney Dis. 1998;32:64-71.
(23.) Baliga R, Ueda N, Walker, PD, Shah SV. Oxidant mechanisms in toxic acute renal failure. Am J Kidney Dis. 1997;29:465-477.
(24.) Kerr ME, Bender CM, Monti EJ. An introduction to oxygen free radicals. Heart Lung. 1996;25:200-209.
(25.) Safirstein K, Andrade L, Vieira JM. Acetylcysteine and nephrotoxic effects of radiographic contrast agents: a new use for an old drug. N Engl J Med. 2000;343:210-212.
(26.) Yaqoob MM, Alkhunaizi AA, Edeisteine CL, Conger JD, Schrier RW. Acute renal failure: pathogenesis, diagnosis, and management. In: Schrier RW, ed. Renal and Electrolyte Disorders. 5th ed. Philadelphia, Pa: Lippincott-Raven; 1997:449-452.
(27.) Nursing 200l Drug Handbook. 21st ed. Springhouse, Pa: Springhouse Publishing Co; 2001.
(28.) Brady HR, Singer GG. Acute renal failure. Lancer. 1995;346:1553-1540.
(29.) Baim DS, Grossman W, eds. Grossman's Cardiac Catheterization, Angiography, and Intervention. 6th ed. Philadelphia, Pa: Lippincott Williams & Wilkins; 2000:30-32.
(30.) Acetylcysteine solution USP [package insert]. Shirley, NY: American Regent Laboratories Inc; 1998.
(31.) Vale JA, Proudfoot AT. Paracetamol (areta-minophen) poisoning. Lancet. 1995;346:547-552.
(32.) Sheikh-Hamid D, Timmins K, Jalali Z. Cisplatin-induced renal toxicity: possible reversal by N-acetylcysteine treasment J Am Soc Nephrol. 1997;8:1640-1644.
(33.) Carey RM, Siragy HM, Ragsdale NV, et al. Dopamine-1 and dopamine-2 mechanisms in the control of renal function. Am J Hypertens. 1990;3(6 Pt 2):59S-63S.
(34.) Singer I, Epstein M. Potential of dopamine A-1 agonists in the management of acute renal failure. Am J Kidney Dis. 1998;31:743-755.
(35.) Allison NL, Dubb JW, Ziemniak JA, Alexander F, Stote RM. The effect of fenoldopam, a dopaminergic agonist, on renal hemodynamics. Clin Pharmacol Ther. 1987;11:282-288.
(36.) Bakris GL, Lass NA, Glock D. Renal hemo-dynamics in radiocontrast medium-induced renal dysfunction: a role for dopamine-1 receptors. Kidney Int. 1999;56:206-210.
(37.) Lokhandwala MF. Preclinical and clinical studies on cardiovascular and renal effects of fenoldopam: a DA-1 receptor agonist. Drug Dev Res. 1987;10:123-134.
(38.) Mathur VS. Swan SK, Lambrechr LJ, et al. The effects of fenoldopam, a selective dopamine receptor agonist, on systemic and renal hemodynamics in normotensive subjects. Crit Care Med. 1999;27:1832-1837.
(39.) Corlopam [package insert]. Abbott Park, Ill: Abbott Laboratories; 2000.
(40.) Chase SL. The newest critical care drugs. RN. May 1999;62:34-39.
RELATED ARTICLE: Risk factors for nephrotoxic effects induced by radiological contrast material
Preexisting renal insufficiency
Diabetes mellitus
History of multiple interventional procedures in which contrast material was used
Dehydration
Congestive heart failure
Increased age
Multiple myeloma
Need for large doses of contrast material, particularly high-osmolality media
Use of nonsteroidal anti-inflammatory drugs
Use of angiotensin-converting enzyme inhibitors
Use of metformin
Authors
Elizabeth J. Thompson is the nurse manager in a medical cardiac telemetry unit at Lancaster General Hospital, Lancaster, Pa.
Stacey L. King works is the nurse manager in a medical cardiac telemetry unit at Lancaster General Hospital, Lancaster, Pa.
COPYRIGHT 2003 American Association of Critical-Care Nurses
COPYRIGHT 2003 Gale Group