* EVIDENCE-BASED ANSWER
When herpes simplex virus (HSV) type 1 lesions are in the papule or vesicle stage, there is no benefit to starting oral acyclovir (strength of recommendation [SOR]: C, based on expert opinion). However, topical acyclovir 5% cream applied 5 times a day decreases pain and the duration of hard crust (SOR: B, extrapolated from randomized controlled trials [RCTs]).
If started at the onset of symptoms (during the prodrome stage), acyclovir (400 mg 5 times daily for 5 days) decreases pain and healing time to loss of crust and valacyclovir (2 g twice daily for 1 day) reduces the lesion duration and time to healing and may prevent lesion development (SOR: A, based on RCTs).
* EVIDENCE SUMMARY
Cold sores, or herpes labialis, are caused by HSV. Recurrent lesions progress quickly through several stages (prodrome, erythema, papule, vesicle, ulcer, crust, residual swelling, healed). (1) Because of the rapid development of the vesicle stage (<12 hours) and the rapid decrease in detectable virus after 48 hours, studies of antiviral therapy empirically require early treatment within the first several hours of signs or symptoms of a recurrence. For this reason, there are no controlled trials of oral medications given later than 12 hours after the onset of recurrent symptoms.
Although limited, the clearest indication of appropriate timing for HSV 1 treatment with acyclovir comes from a well-designed, double-blinded RCT of 174 adults with a history of culture confirmed HSV labialis who initiated self-treatment with acyclovir 400 mg or placebo 5 times a day for 5 days. Patients were asked to defer treatment until the next episode if they awoke with the lesion or first noticed them in the vesicle or ulcer stage.
Ninety-seven percent of the patients started treatment within 1 hour of signs/symptoms of a recurrence. Of the 174 patients, 90 had lesions in the prodrome or erythema stage at the start of treatment and 84 had lesions in the papule or vesicle stage.
Overall, acyclovir did not effect lesion progression, size, or healing time to loss of hard crust or normal skin. However, the mean duration of pain for all patients significantly decreased (2.5 days vs 3.8 days for placebo, P=.01). For the subgroup of patients who started acyclovir treatment in the prodrome or erythema stage, the mean duration of pain significantly decreased (2.5 days vs 3.9 days for placebo, P=.02), as did healing time to loss of crust (5.8 days vs 7.9 days for placebo, P=.03). Among those who started acyclovir in the papular stage, the trend was toward drug benefit, but this was not statistically significant (mean pain duration: 2.5 vs. 3.6, P=.36; mean healing time to loss of crust: 8.0 vs. 7.2, P=.52). (2) This evidence supports early (prodrome or erythema stage) but not late (macule, papule, vesicle, or crusted stage) treatment of HSV 1 with oral acyclovir.
Topical application of 5% acyclovir cream significantly decreases clinician-assessed duration of the episode and duration of patient-reported pain, based on 2 double-blind, multicenter RCTs that used a vehicle control. In these trials, 686 and 699 patients self-initiated treatment 5 times a day for 4 days beginning within 1 hour of the onset of a recurrent lesion. In the first study, the mean clinician-assessed duration of the episode with topical acyclovir was 4.3 vs 4.8 days for placebo (hazard ratio [HR]=1.23; 95% confidence interval [CI], 1.06-1.44), and the mean duration of patient-assessed pain was 2.9 vs 3.2 days (HR=1.20; 95% CI, 1.03-1.40). The second study showed a mean clinician-assessed duration with topical acyclovir of 4.6 vs 5.2 days for control (HR=1.24; 95% CI, 1.06-1.44), and the mean duration of patient-assessed pain was 3.1 vs 3.5 days (HR=1.21; 95% CI, 1.04-1.40). Benefits were seen regardless of whether treatment was initiated early (prodrome or erythema stage) or late (macule, papule, vesicle or crusted stage). (3)
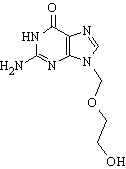
Recent studies of valacyclovir (the L-valine ester of acyclovir, which has 3 to 5 times greater bioavailability) offer the most promise for effective self-initiated treatment of recurrent herpes labialis. In a report of 2 well-designed, multicenter RCTs, valacyclovir at the FDA-approved dosage of 2 g twice daily for 1 day at the onset of symptoms (before visible signs of a cold sore) significantly decreased the mean duration of the lesion and time to lesion healing. In the first study (n=603), episode duration was decreased by 1.1 days (5.0 days vs 6.1 days for placebo; 95% CI, -1.6 to -0.6) and in the second study (n=605) by 1.0 day (5.3 vs 6.3 days for placebo; 95% CI, -1.0 to -0.5). In the first study, the time to lesion healing was decreased by 1.3 days (4.8 vs 6.1 days for placebo; 95% CI, -1.9 to -0.7) and in the second study by 1.2 days (5.1 vs. 6.4 days; 95% CI, -1.8 to -0.7). There also was a trend towards preventing the development of lesions, but this was not statistically significant. (4)
* RECOMMENDATIONS FROM OTHERS
The BMJ Clinical Evidence Guideline reiterates that no trials compare early vs late treatment, so no firm conclusions about the efficacy of delayed treatment can be drawn. (5) UpToDate reports that HSV 1 studies take into account that acyclovir acts only during active viral replication, which largely precedes symptoms, and thus suggest that it has little effect if begun after the appearance of lesions. (6)
Wendy S. Madigosky, MD, MS, Susan Meadows, MLS, Department of Family and Community Medicine, University of Missouri-Columbia
REFERENCES
(1.) Spruance S, Overall J, Kern E, Krueger G, Pliam V, Miller W. The natural history of recurrent herpes simplex labialis. JAMA 1977; 297:69-75.
(2.) Spruance S, Stewart J, Rowe N, McKoeugh M, Wenerstrom G, Freeman D. Treatment of recto-rent herpes simplex labialis with oral acyclovir. J Infect Dis 1990; 161:181-190.
(3.) Spruance S, Nett R, Marbury T, Wolff R, Johnson J, Spaulding T. Acyclovir cream for treatment of herpes simplex labialis: results of two randomized, double-blind, vehicle-controlled multicenter clinical trials. Antimicrobial Agents Chemother 2002; 46:2238-2243.
(4.) Spruance S, Jones T, Blatter M, et al. High-dose, short-duration, early valacyclovir therapy for episodic treatment of cold sores: results of two randomized, placebo-controlled, multicenter studies. Antimicrobial Agents Chemother 2003; 47:1072-1080.
(5.) Clin Evid [online], Issue 10, 2003. London: BMJ Publishing Group, last updated December 2002. Available at: http://clinicalevidence.com. Accessed on May 19, 2004.
(6.) Klein R. Treatment and prevention of herpes simplex virus type 1 infection. UpToDate version 12.2, last updated February 25, 2004. Available at: UpToDate.com. Accessed on July 14, 2004.
(7.) Available at: www.drugstore.com. Accessed on August 18, 2004.
CLINICAL COMMENTARY
For late presenters, review local care and hygiene; for all patients, review management of recurrences
Patients seek treatment for herpes labialis due to bothersome physical symptoms and psychosocial implications. Many patients can identify prodromal symptoms such as localized itching, burning, irritation, or pain. Diagnosis of the initial episode is frequently delayed as patients are evaluated after the time period when studies have shown the most benefit from antivirals. For the late presenters, I review local care and hygiene, and for all patients I review management of recurrences.
Patient-initiated treatment is effective for those who can recognize the earliest signs and symptoms and start treatment immediately with either a topical or systemic antiviral. Both formulations decrease the lesion time to healing and pain if started at the first onset of symptoms.
Cost is an important consideration when selecting a particular formulation. Approximate price for the regimens presented here are $12 for 5 days of oral acyclovir, $27 for 1 day of oral valacyclovir, and $37 for a 2-g tube of acyclovir cream, which can be used for more than 1 episode. (7) Other factors to consider are pill burden, duration of treatment, patient preference, and lifestyle. Patients can keep a refill or medicine on-hand to manage recurrences with the advice to begin immediately with onset of signs or symptoms.
Owen McCormack, DO, Baylor College of Medicine, Houston, TX
COPYRIGHT 2004 Dowden Health Media, Inc.
COPYRIGHT 2004 Gale Group